Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the most effective treatment method for lymphoid, haematopoietic and related tissue malignancies as well as non-malignant disorders. In 2017, 18.281 number of allo-HSCT were performed in Europe and associated countries reported by 683 centers in 50 countries, with acute leukemia being the main indication [1]. The approachability and outcome of allo-HSCT are steadily improving due to wide application of reduced-intensity conditioning (RIC), new methods of graft-versus-host disease (GvHD) prophylaxis, haploidentical transplantation, and introduction of novel molecules and drugs for bridge therapy before allo-HSCT, along with prevention and treatment of relapses after allo-HSCT both in adults and pediatric patients [2-8] Invasive fungal disease (IFD) is a common infectious complication during remission-induction and/or consolidation chemotherapy for aggressive hematologic malignancies. The patients with acute leukemia and high-risk myelodysplastic syndrome are also at high risk for IFD [9-10]. Some patients with relapsed/refractory lymphoma could be, under some circumstances, also attributed to the high-risk group [11]. Introducing new antifungal drugs and diagnostic procedures has improved prognosis of IFD in hematological disorders. Many of these patients will subsequently be referred for allo-HSCT because of high-risk hematological malignances. The number of patients with IFD who are candidates for allo-HSCT has been also increased, and the problems related to the transplant procedure are pressing now. An observational study of the Transplant Associated Infection Surveillance Network (TRANSNET) suggests that the post-transplant IFD remains problematic, with cumulative incidence rates varying between 5.8 and 7.7% [12]. The role of IFD revealed prior to allo-HSCT is still a subject of controversy. Historically, IFD has been a major barrier for allo-HSCT. Previous studies have shown that invasive aspergillosis (IA) may have a significant role in clinical outcome of allo-HSCT [13-15]. Fukuda et al. have summarized the 10-year experience of Fred Hutchinson Cancer Research Center, having shown that the post-transplant IA occurred in 13 of 45 patients with a pre-transplant IA history (29%) [16]. Nine infectious events were considered to be recurrent by anatomic site and timing. Compared with all other patients who received allo-HSCT over the same period, the patients with IA history had lower 1-year overall survival rate (56% versus 77%; P=0.0001), and higher transplant-related mortality (38% versus 21%; P=0.0001) by 100 days after HSCT, associated mainly with IA and other pulmonary complications. The CIBMTR data also confirm that 5-year overall survival was 30% (95% Confidence interval (CI): 26-34%) at 5 years in patients with pre-transplant IFD versus 45% (95% CI: 44-46%) in control population (p <0.0001). The lower overall survival seems to be a composite result of higher relapse rates and higher non-relapse mortality in the patients with pre-existing IFD [17].
Historically, pre-transplant IFD was considered a relative contraindication to HSCT. However, recent studies have demonstrated a controversial point, e.g., a single-center study on behalf of CIC 725 suggested that IA prior to allo-HSCT did not impair the outcome of transplantation procedure with effective diagnosis and secondary prophylaxis of IFD, as reported at the 41st Annual EBMT Meeting and 57th Annual ASH Meeting in 2015 [18, 19]. A retrospective EBMT analysis by the Infectious Diseases and Acute Leukemia Working Parties concerning influence of pre-existing invasive aspergillosis upon allo-HSCT outcome in acute leukemia patients (published online in October 2015 in Bone Marrow Transplantation) confirm our data that, in general, a history of IA should not be a contraindication when considering allo-HSCT in acute leukemia patients [20]. Penack O. et al. found only a trend toward lower overall survival (P=0.078, hazard ratio (HR) [95% confidence interval (CI): 1.16 (0.98, 1.36)], and higher non-relapse mortality [P=0.150, HR (95% CI): 1.19 (0.94, 1.50)] in allo-HSCT recipients with pre-existing IA [20]. So far, there are no available data on clinical effects of other then IA pre-existing IFD and in pediatric allo-HSCT recipients.
The aim of this study was to estimate impact of prior proven or probable invasive fungal diseases on clinical outcome of allo-HSCT in children and adults.
Patients and methods
We have conducted a prospective single center study, where 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016, with median follow-up time of 20 months and median age of 24 y.o. [2 months to 76 years]. The study cohort included 164 children (<18 yo), 340 adults, 52% were males. Most patients had high-risk acute leukemia (74.6%). Allo-HSCT from MUD was performed in 58.5%; MRD, 22.5%; haplo-HSCT, 19%. Reduced-intensity conditioning regimens (RIC) were predominant (67% of the cases). General characteristics of patients, donors and transplants are outlined in Tables 1, 2. The patients with lymphoid, haematopoietic and related tissue malignancies as well as non-malignant disorders received primary chemotherapy and other treatment in various regions of Russian Federation, from where most of the data including history of prior IFD were collected. All the patients with CT-detectable lesions at the time of transplantation were subjected to diagnostic bronchoscopy with bronchoalveolar lavage (BAL) microscopy, microbiological cultures and galactomannan (GM) test. EORTC/MSG 2008 criteria were used for the diagnosis of proven and probable IFD as well as to evaluate response to therapy. An “active” invasive fungal disease means IFD diagnosed just before allo-HSCT during examination at <1 month before starting the conditioning regimen.

The following primary endpoints were used: incidence of pre-existing IFD, incidence of relapse or progression of IFD after allo-HSCT, and overall survival (OS). The secondary endpoints included influence of pre-existing IFD on other outcomes of allo-HSCT, i.e., acute GvHD, chronic GvHD, relapse of underlying disease.
Overall survival was estimated using the Kaplan–Meier method. Mortality due to any cause was considered as a distinct event. Patients alive at the end of the follow-up were censored at this date. Patients with pre-existing IFD and without pre-existing IFD will be compared by the log-rank test. A Cox regression was applied, in order to compare the outcomes the study groups.
Results

The overall incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria 90.8% of patients had probable IFD, and 9.2% exhibited proven fungal invasion. Patients with lymphoma, as well as those with acute myeloid leukemia had a higher rate of pre-existing IFD at the time of allo-HSCT (Fig. 1).
The pathogens detected in IFD prior to allo-HSCT were as follows: invasive aspergillosis, 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; Pneumocystis pneumoniae (PCP), 1,3%; combination of IA with Mu was found in 2 patients, IC in one case, and PCP, in one another case (Fig. 2). The main sites of infection were lungs (95%), other affected sites were predominantly combined with lung lesions, i.e., maxillary or frontal sinuses, 9%; spleen, 6%; liver, 6%, and soft tissues, 3% (Fig. 3).

The median time from IFD to allo-HSCT was 86 days [1 day to 4.5 years]. Antifungal therapy before allo-HSCT was administered in 75% patients. The median duration of antifungal therapy before allo-HSCT was 65 days [1 day-11 months]. Complete response to antifungal treatment was achieved in 38.2% patients, partial response or stabilization were observed in 35.5%, and 26.3% patients had “active IFD”. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology, with median duration of clinical effect for 78 [21-217] days, and median therapy length for 166 [32 to 394 days].
Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5% (Fig. 4). Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% vs 21.1%, p=0.03) (Fig. 5). We detected no significant differences in cumulative incidence of acute or chronic GVHD, and relapse rates in the study group as compared to the patients without history of IFD. Patients and HSCT characteristics, CMV reactivation, graft hypofunction did not show any significant association with incidence of relapse, or progression of IFD after allo-HSCT. The characteristics related to pre-existing IFD (status of IFD at the HSCT, time from IFD to HSCT, duration of antifungal therapy before HSCT) also had no impact on probability of relapse or progression of IFD after allo-HSCT.

Three-year OS after allo-HSCT was 67.5%. The impact of prior IFD upon overall survival in allo-HSCT recipients was not statistically significant in the entire group (60.5% vs 68.7%, p=0.1) (Fig. 6). Similar results were obtained for the separate groups of children (50.0% vs 57.4%, p=0.3), and adults (63.3% vs 74.6%, p=0.09). The main outcomes of allo-HSCT are presented in Table 3.
The worst outcome was observed in patients with “active IFD” and active underlying disease at the moment of allo- HSCT (3-year OS – 20%, p<0.001; HR (95% CI): 5.81 (2.81 – 11.87)). However, OS values in patients with “active IFD” and remission of underlying disease were similar to survival rate of patients without history of IFD (80% vs 68.7%, p=0.2, p=0.57, HR [(95% CI): 0.67 (0.16 – 2.71)] (Fig. 7).

Table 3. The main outcomes of allo-HSCT in patients with history of prior IFD as compared to patients without history of IFD

Discussion
In the present study, we analyzed large data set of patients with different hematological malignancies and non-malignant disorders undergoing allo-HSCT between 2013 and 2016 in a single BMT center (CIC 725). We would highlight the real-life character of study. The entire cohort of allo-HSCT recipients was included in the observation period without exception of any patients, regardless of underlying disease or status at the moment of allo-HSCT. Also we would emphasize the participation of pediatric cohort that was presented by 164 children.
In our population of allo-HSCT recipients, 15% had proven and probable invasive fungal disease before transplantation. Moreover, most of them (>60%) had signs of the infection at the moment of allo-HSCT. We believe that there are several factors that could contribute to our results. Out BMT team has wide diagnostic opportunities and an active diagnostic strategy related to infections, and is able to perform the on-place assessment of infectious state of the patient before allo-HSCT, because of lacking necessary diagnostic procedures in most regions where the patients were initially treated. Due to successful implementation of such strategy, we are more often prone for active treatment and avoiding delays with allo-HSCT. An unexpected result for us is the fact that a quarter of patients with lymphomas had IFD before allo-HSCT. This result may be due to high pre-treatment burden in these patients, most of them were patients with Hodgkin lymphoma who underwent more than 6 lines of chemotherapy before allo-HSCT.
Our study has also shown that the cumulative incidence of relapse or progression of invasive fungal disease after allo-HSCT was 14.5%. The only risk factor for relapse or progression of IFD was lack of complete remission of the underlying disease at the moment of HSCT. That result corresponded to the earlier reported data [16], but we didn’t find any additional risk factors associated with bone marrow transplant procedure or antifungal treatment before allo-HSCT.
In the present study, we demonstrated that invasive fungal disease prior to the allo-HSCT did not impact on outcome of this treatment in children and adults. We suggest that there are several features that may have endow to obtained results.
Firstly, our study included allo-HSCT recipients who have been transplanted over recent years, in comparison with published studies [13-16, 20]. An overall better supportive care management was applied over last years, thus improving, specifically the outcome of allo-HSCT in patients with infectious complications including IFD. We believe that active diagnostic strategy and wide implementation of modern medications for secondary prophylaxis in our center played a role in improving the outcome of allo-HSCT in the patients with pre-existing IFD. It has been shown in several trials that secondary antifungal prophylaxis with voriconazole leads to considerably lower IA relapse rates as compared with those reported in historical controls, since Aspergillus spp. is a prevailing pathogen in pre-transplant IFD in our study [21-23].
Secondly, this study demonstrated the central role of the underlying disease status upon outcome of the allo-HSCT, and influence on the course of the infectious complications after HSCT, IFD in our case. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT. This hypothesis is supported by publications from a French-Belgium study group, demonstrating that the outcome of severe infectious complications in patients with hematological malignancies has been considerably improved during the last decade and is mostly determined by the status of the underlying disease [24-25].
Thirdly, our study has limitations due to relatively small study cohort from a single center data. That is why the result may be not accurate enough to evaluate the effect of IFD upon allo-HSCT outcome. At the same time, it reflects the situation during certain time which significantly affects the results obtained. Therefore, we cannot exclude the possibility that pre-existing IFD has a higher adverse impact on allo-HSCT outcome than our data may suggest.
In conclusion, we found out no significant impact upon important allo-HSCT transplant outcomes, such as survival, GvHD and relapse. Our data suggest that a history of IFD should not be considered a contraindication for allo-HSCT. We are currently continuous an observational prospective study to be able to more precisely investigate the impact of IFD on allo-HSCT.
Acknowledgments
The authors would like to acknowledge all medical staff at our University’ BMT clinic CIC725. Special thanks to our ICU department, our transplant nurses’ team for their particular care of our patients. Many thanks to specialists of Department of Clinical Microbiology at the First Pavlov State Medical University of Saint-Petersburg, especially to dr. Olga Pinegina and Chief of the Department, and special gratitude to patients and their relatives.
Conflict of interest
No conflict of interests is declared.
References
- Passweg JR, Baldomero H, Basak GW, Chabannon C, Corbacioglu S, Duarte R, Kuball J, Lankester A, Montoto S, de Latour RP, Snowden JA, Styczynski J, Yakoub-Agha I, Arat M, Mohty M, Kröger N; European Society for Blood and Marrow Transplantation (EBMT). The EBMT activity survey report 2017: a focus on allogeneic HCT for nonmalignant indications and on the use of non-HCT cell therapies. Bone Marrow Transplant 2019, Feb 6. doi: 10.1038/s41409-019-0465-9.
- Afanasyev BV, Zubarovskaya LS, Semenova EV, Ivanova NE, Alyanskiy AL, Morozova EV, Mikhailova NB, Darskaya EI, Estrina MA, Golovacheva AA, Babenko EV, Bondarenko SN, Ganapiev AA, Bogomolny MP. The experience in non-relative allogenic transplantation of stem hemopoietic cells in the clinic of bone marrow transplantation at I. P. Pavlov St. Petersburg Medical Academy. Terapevticheskii Arkhiv 2007, 79 (7):36-43 (In Russian).
- Bondarenko SN, Moiseev IS, Slesarchuk OA, Darskaya EI, Ekushev KA, Smirnova AG, Alyanskiy AL, Gindina TL, Babenko EV, Kuzmich EV, Semenova EV, Kulagin AD, Zubarovskaya LS, Afanasyev BV. Allogeneic hematopoietic stem cell transplantation in children and adults with acute lymphoblastic leukemia. Cell Ther Transplant. 2016, 5 (2):12-20.
- Afanasyev BV, Zubarovskaya LS, Moiseev IS. Allogeneic hematopoietic stem cell transplantation in children: now, problems and prospects. Russian Journal of Children Hematology and Oncology. 2015, 2: 28-42 (In Russian).
- Baron F, Labopin M, Peniket A, Jindra P, Afanasyev B, Sanz M.A, Deconinck E, Nagler A, Mohty M. Reduced-intensity conditioning with fludarabine and busulfan versus fludarabine and melphalan for patients with acute myeloid leukemia: A report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Cancer 2015; 121(7): 1048-1055.
- Moiseev IS, Pirogova OV, Babenko EV, Gindina TL, Darskaya EI, Morozova EV, Bondarenko SN, Afanasyev BV. Single-agent post-transplantation cyclophosphamide versus calcineurin-based graft-versus-host disease prophylaxis in matched related bone marrow transplantation. Cell Ther Transplant. 2017; 6 (4): 52-59.
- Bykova TA, Borovkova AS, Osipova AA, Ovechkina VN, Sheveleva PV, Nadzhafava KU, Yager VU, Paina OV, Kozhokar PV, Alyanskyi AL, Kulagin AD, Semenova EV, Smirnov BI, Zubarovskaya LS, Afanasyev BV. Acute GvHD prophylaxis with posttransplant cyclophosphamide after hematopoietic stem cell transplantation (HSCT) for non-malignant disorders. Pediatric Hematology/Oncology and Immunopathology 2018, 17 (2), pp. 51-58 (In Russian).
- Moiseev IS, Darskaya EI, Bykova TA, Morozova EV, Alyanskiy AL, Babenko EV, Bondarenko SN, Markova IV, Afanasyev BV. Different risk factors of acute and chronic graft-versus-host disease with conventional prophylaxis and posttransplantation cyclophosphamide in matched related and unrelated donor transplantation. Cell Ther Transplant. 2018; 7 (4): 29-37. DOI: 10.18620/ctt-1866-8836-2018-7-4-29-37.
- Shadrivova OV, Khostelidi SN, Chudinovskikh YA, Zabirov VS, Borzova YV, Desyatik EA, Volkova AG, Popova MO, Markova IV, Uspenskaya OS, Ruzhinskaya OS, Shneyder TV, Bogomolova TS, Ignatyeva SM, Zubarovskaya LS, Afanasyev BV, Klimko NN. Invasive aspergillosis and mucormycosis in oncohematological patients. Oncohematology 2018, 13(2):39-47. DOI: 10.17650/1818-8346-2018-13-2-39-47. (In Russian).
- Klimko NN, Khostelidi SN, Volkova AG, Popova MO, Bogomolova TS, Zubarovskaya LS, Kolbin AS, Medvedeva NV, Zuzgin IS, Simkin SM, Vasilyeva NV. Afanasyev BV. Mucormycosis in haematological patients: case report and results of prospective study in Saint Petersburg, Russia. Mycoses 2014, 57: 91-96. doi:10.1111/myc.12247.
- Teng JC, Slavin MA, Teh BW, Lingaratnam SM, Ananda-Rajah MR, Worth LJ, Seymour JF, Thursky KA. Epidemiology of invasive fungal disease in lymphoproliferative disorders. Haematologica. 2015; 100(11):e462-6. doi: 10.3324/haematol.2015.126698.
- Kontoyiannis DP, Marr KA, Park BJ, Alexander BD, Anaissie EJ, Walsh TJ, Ito J, Andes DR, Baddley JW, Brown JM, Brumble LM, Freifeld AG, Hadley S, Herwaldt LA, Kauffman CA, Knapp K, Lyon GM, Morrison VA, Papanicolaou G, Patterson TF, Perl TM, Schuster MG, Walker R, Wannemuehler KA, Wingard JR, Chiller TM, Pappas PG. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the transplant-associated infection surveillance network (TRANSNET) database. Clin Infect Dis. 2010, 50:1091–1100. DOI: 10.1086/651263.
- Martino R, Lopez R, Sureda A, Brunet S, Domingo-Albos A. Risk of reactivation of a recent invasive fungal infection in patients with hematological malignancies undergoing further intensive chemo-radiotherapy. A single-center experience and review of the literature. Haematologica. 1997; 82:297–304.
- Offner F, Cordonnier C, Ljungman P, Prentice HG, Engelhard D, De Bacquer D, Meunier F, De Pauw B. Impact of previous aspergillosis on the outcome of bone marrow transplantation. Clin Infect Dis. 1998, 26:1098–1103. DOI: 10.1086/520274.
- Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 2002;34: 909-917. DOI: 10.1086/339202.
- Fukuda T, Boeckh M, Guthrie KA, Mattson DK, Owens S, Wald A, Sandmaier BM, Corey L, Storb RF, Marr KA. Invasive aspergillosis before allogeneic hematopoietic stem cell transplantation: 10-year experience at a single transplant center. Biol Blood Marrow Transplant. 2004; 10: 494-503. DOI: 10.1016/j.bbmt.2004.02.006.
- Maziarz RT, Brazauskas R, Chen M, McLeod AA, Martino R, Wingard JR, Aljurf M, Battiwalla M, Dvorak CC, Geroge B, Guinan EC, Hale GA, Lazarus HM, Lee JW, Liesveld JL, Ramanathan M, Reddy V, Savani BN, Smith FO, Strasfeld L, Taplitz RA, Ustun C, Boeckh MJ, Gea-Banacloche J, Lindemans CA, Auletta JJ, Riches ML. Pre-existing invasive fungal infection is not a contraindication for allogeneic HSCT for patients with hematologic malignancies: a CIBMTR study. Bone Marrow Transplant. 2017; 52(2):270-278. DOI: 10.1038/bmt.2016.259.
- Popova MO, Volkova A, Elias Soulaiman S, Vavilov V, Bondarenko S, Slesarchuk O, Smirnova A, Shadrivova O, Khostelidi S, Ignatyeva S, Bogomolova T, Zubarovskaya L, Klimko N, Afanasyev B. Allogeneic hematopoietic stem cell transplantation in patients with invasive aspergillosis. Bone Marrow Transplantation. 2015, Volume 50, Supplement 1, S33.
- Popova MO, Volkova AG, Soulaiman SE, Pinegina ON, Ignatyeva SM, Bogomolova TS, Smirnova AG, Vladovskaya M D, Bondarenko SN, Zubarovskaya LS, Klimko NN, Afanasyev BV. Outcome of allogeneic hematopoietic stem cell transplantation in patients with prior invasive aspergillosis. Blood. 2015; 126(23):3123; DOI: https://doi.org/
- Penack O, Tridello G, Hoek J, Socié G, Blaise D, Passweg J, Chevallier P, Craddock C, Milpied N, Veelken H, Maertens J, Ljungman P, Cornelissen J, Thiebaut-Bertrand A, Lioure B, Michallet M, Iacobelli S, Nagler A, Mohty M, Cesaro S. Influence of pre-existing invasive aspergillosis on allo-HSCT outcome: a retrospective EBMT analysis by the Infectious Diseases and Acute Leukemia Working Parties. Bone Marrow Transplant. 2016; 51(3):418-23. doi: 10.1038/bmt.2015.237.
- Allinson K, Kolve H, Gumbinger HG, Vormoor HJ, Ehlert K, Groll AH. Secondary antifungal prophylaxis in paediatric allogeneic haematopoietic stem cell recipients. J Antimicrob Chemother. 2008;61:734-742.
- Cordonnier C, Maury S, Pautas C, Bastie JN, Chehata S, Castaigne S, Kuentz M, Bretagne S, Ribaud P. Secondary antifungal prophylaxis with voriconazole to adhere to scheduled treatment in leukemic patients and stem cell transplant recipients. Bone Marrow Transplant. 2004;33(9):943-948.
- Cordonnier C, Rovira M, Maertens J, Olavarria E, Faucher C, Bilger K, Pigneux A, Cornely OA, Ullmann AJ, Bofarull RM, de la Cámara R, Weisser M, Liakopoulou E, Abecasis M, Heussel CP, Pineau M, Ljungman P, Einsele H. Voriconazole for secondary prophylaxis of invasive fungal infections in patients with allogeneic stem cell transplants recipients: results of the VOSIFI Study Group; Infectious Diseases Working Party, European Group for Blood and Marrow Transplantation. Haematologica. 2010; 95(10):1762-1768. doi:10.3324/haematol.2009.020073.
- Azoulay E, Mokart D, Pène F, Lambert J, Kouatchet A, Mayaux J, Vincent F, Nyunga M, Bruneel F, Laisne LM, Rabbat A, Lebert C, Perez P, Chaize M, Renault A, Meert AP, Benoit D, Hamidfar R, Jourdain M, Darmon M, Schlemmer B, Chevret S, Lemiale V. Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium – a groupe de recherche respiratoire en reanimation onco-hematologique study. J Clin Oncol. 2013;31(22):2810-2818. doi: 10.1200/JCO.2012.47.2365.
- Legrand M, Max A, Peigne V, Mariotte E, Canet E, Debrumetz A, Lemiale V, Seguin A, Darmon M, Schlemmer B, Azoulay E. Survival in neutropenic patients with severe sepsis or septic shock. Crit Care Med. 2012;40(1):43-9. doi: 10.1097/CCM.0b013e31822b50c2.
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the most effective treatment method for lymphoid, haematopoietic and related tissue malignancies as well as non-malignant disorders. In 2017, 18.281 number of allo-HSCT were performed in Europe and associated countries reported by 683 centers in 50 countries, with acute leukemia being the main indication [1]. The approachability and outcome of allo-HSCT are steadily improving due to wide application of reduced-intensity conditioning (RIC), new methods of graft-versus-host disease (GvHD) prophylaxis, haploidentical transplantation, and introduction of novel molecules and drugs for bridge therapy before allo-HSCT, along with prevention and treatment of relapses after allo-HSCT both in adults and pediatric patients [2-8] Invasive fungal disease (IFD) is a common infectious complication during remission-induction and/or consolidation chemotherapy for aggressive hematologic malignancies. The patients with acute leukemia and high-risk myelodysplastic syndrome are also at high risk for IFD [9-10]. Some patients with relapsed/refractory lymphoma could be, under some circumstances, also attributed to the high-risk group [11]. Introducing new antifungal drugs and diagnostic procedures has improved prognosis of IFD in hematological disorders. Many of these patients will subsequently be referred for allo-HSCT because of high-risk hematological malignances. The number of patients with IFD who are candidates for allo-HSCT has been also increased, and the problems related to the transplant procedure are pressing now. An observational study of the Transplant Associated Infection Surveillance Network (TRANSNET) suggests that the post-transplant IFD remains problematic, with cumulative incidence rates varying between 5.8 and 7.7% [12]. The role of IFD revealed prior to allo-HSCT is still a subject of controversy. Historically, IFD has been a major barrier for allo-HSCT. Previous studies have shown that invasive aspergillosis (IA) may have a significant role in clinical outcome of allo-HSCT [13-15]. Fukuda et al. have summarized the 10-year experience of Fred Hutchinson Cancer Research Center, having shown that the post-transplant IA occurred in 13 of 45 patients with a pre-transplant IA history (29%) [16]. Nine infectious events were considered to be recurrent by anatomic site and timing. Compared with all other patients who received allo-HSCT over the same period, the patients with IA history had lower 1-year overall survival rate (56% versus 77%; P=0.0001), and higher transplant-related mortality (38% versus 21%; P=0.0001) by 100 days after HSCT, associated mainly with IA and other pulmonary complications. The CIBMTR data also confirm that 5-year overall survival was 30% (95% Confidence interval (CI): 26-34%) at 5 years in patients with pre-transplant IFD versus 45% (95% CI: 44-46%) in control population (p <0.0001). The lower overall survival seems to be a composite result of higher relapse rates and higher non-relapse mortality in the patients with pre-existing IFD [17].
Historically, pre-transplant IFD was considered a relative contraindication to HSCT. However, recent studies have demonstrated a controversial point, e.g., a single-center study on behalf of CIC 725 suggested that IA prior to allo-HSCT did not impair the outcome of transplantation procedure with effective diagnosis and secondary prophylaxis of IFD, as reported at the 41st Annual EBMT Meeting and 57th Annual ASH Meeting in 2015 [18, 19]. A retrospective EBMT analysis by the Infectious Diseases and Acute Leukemia Working Parties concerning influence of pre-existing invasive aspergillosis upon allo-HSCT outcome in acute leukemia patients (published online in October 2015 in Bone Marrow Transplantation) confirm our data that, in general, a history of IA should not be a contraindication when considering allo-HSCT in acute leukemia patients [20]. Penack O. et al. found only a trend toward lower overall survival (P=0.078, hazard ratio (HR) [95% confidence interval (CI): 1.16 (0.98, 1.36)], and higher non-relapse mortality [P=0.150, HR (95% CI): 1.19 (0.94, 1.50)] in allo-HSCT recipients with pre-existing IA [20]. So far, there are no available data on clinical effects of other then IA pre-existing IFD and in pediatric allo-HSCT recipients.
The aim of this study was to estimate impact of prior proven or probable invasive fungal diseases on clinical outcome of allo-HSCT in children and adults.
Patients and methods
We have conducted a prospective single center study, where 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016, with median follow-up time of 20 months and median age of 24 y.o. [2 months to 76 years]. The study cohort included 164 children (<18 yo), 340 adults, 52% were males. Most patients had high-risk acute leukemia (74.6%). Allo-HSCT from MUD was performed in 58.5%; MRD, 22.5%; haplo-HSCT, 19%. Reduced-intensity conditioning regimens (RIC) were predominant (67% of the cases). General characteristics of patients, donors and transplants are outlined in Tables 1, 2. The patients with lymphoid, haematopoietic and related tissue malignancies as well as non-malignant disorders received primary chemotherapy and other treatment in various regions of Russian Federation, from where most of the data including history of prior IFD were collected. All the patients with CT-detectable lesions at the time of transplantation were subjected to diagnostic bronchoscopy with bronchoalveolar lavage (BAL) microscopy, microbiological cultures and galactomannan (GM) test. EORTC/MSG 2008 criteria were used for the diagnosis of proven and probable IFD as well as to evaluate response to therapy. An “active” invasive fungal disease means IFD diagnosed just before allo-HSCT during examination at <1 month before starting the conditioning regimen.

The following primary endpoints were used: incidence of pre-existing IFD, incidence of relapse or progression of IFD after allo-HSCT, and overall survival (OS). The secondary endpoints included influence of pre-existing IFD on other outcomes of allo-HSCT, i.e., acute GvHD, chronic GvHD, relapse of underlying disease.
Overall survival was estimated using the Kaplan–Meier method. Mortality due to any cause was considered as a distinct event. Patients alive at the end of the follow-up were censored at this date. Patients with pre-existing IFD and without pre-existing IFD will be compared by the log-rank test. A Cox regression was applied, in order to compare the outcomes the study groups.
Results

The overall incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria 90.8% of patients had probable IFD, and 9.2% exhibited proven fungal invasion. Patients with lymphoma, as well as those with acute myeloid leukemia had a higher rate of pre-existing IFD at the time of allo-HSCT (Fig. 1).
The pathogens detected in IFD prior to allo-HSCT were as follows: invasive aspergillosis, 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; Pneumocystis pneumoniae (PCP), 1,3%; combination of IA with Mu was found in 2 patients, IC in one case, and PCP, in one another case (Fig. 2). The main sites of infection were lungs (95%), other affected sites were predominantly combined with lung lesions, i.e., maxillary or frontal sinuses, 9%; spleen, 6%; liver, 6%, and soft tissues, 3% (Fig. 3).

The median time from IFD to allo-HSCT was 86 days [1 day to 4.5 years]. Antifungal therapy before allo-HSCT was administered in 75% patients. The median duration of antifungal therapy before allo-HSCT was 65 days [1 day-11 months]. Complete response to antifungal treatment was achieved in 38.2% patients, partial response or stabilization were observed in 35.5%, and 26.3% patients had “active IFD”. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology, with median duration of clinical effect for 78 [21-217] days, and median therapy length for 166 [32 to 394 days].
Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5% (Fig. 4). Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% vs 21.1%, p=0.03) (Fig. 5). We detected no significant differences in cumulative incidence of acute or chronic GVHD, and relapse rates in the study group as compared to the patients without history of IFD. Patients and HSCT characteristics, CMV reactivation, graft hypofunction did not show any significant association with incidence of relapse, or progression of IFD after allo-HSCT. The characteristics related to pre-existing IFD (status of IFD at the HSCT, time from IFD to HSCT, duration of antifungal therapy before HSCT) also had no impact on probability of relapse or progression of IFD after allo-HSCT.

Three-year OS after allo-HSCT was 67.5%. The impact of prior IFD upon overall survival in allo-HSCT recipients was not statistically significant in the entire group (60.5% vs 68.7%, p=0.1) (Fig. 6). Similar results were obtained for the separate groups of children (50.0% vs 57.4%, p=0.3), and adults (63.3% vs 74.6%, p=0.09). The main outcomes of allo-HSCT are presented in Table 3.
The worst outcome was observed in patients with “active IFD” and active underlying disease at the moment of allo- HSCT (3-year OS – 20%, p<0.001; HR (95% CI): 5.81 (2.81 – 11.87)). However, OS values in patients with “active IFD” and remission of underlying disease were similar to survival rate of patients without history of IFD (80% vs 68.7%, p=0.2, p=0.57, HR [(95% CI): 0.67 (0.16 – 2.71)] (Fig. 7).

Table 3. The main outcomes of allo-HSCT in patients with history of prior IFD as compared to patients without history of IFD

Discussion
In the present study, we analyzed large data set of patients with different hematological malignancies and non-malignant disorders undergoing allo-HSCT between 2013 and 2016 in a single BMT center (CIC 725). We would highlight the real-life character of study. The entire cohort of allo-HSCT recipients was included in the observation period without exception of any patients, regardless of underlying disease or status at the moment of allo-HSCT. Also we would emphasize the participation of pediatric cohort that was presented by 164 children.
In our population of allo-HSCT recipients, 15% had proven and probable invasive fungal disease before transplantation. Moreover, most of them (>60%) had signs of the infection at the moment of allo-HSCT. We believe that there are several factors that could contribute to our results. Out BMT team has wide diagnostic opportunities and an active diagnostic strategy related to infections, and is able to perform the on-place assessment of infectious state of the patient before allo-HSCT, because of lacking necessary diagnostic procedures in most regions where the patients were initially treated. Due to successful implementation of such strategy, we are more often prone for active treatment and avoiding delays with allo-HSCT. An unexpected result for us is the fact that a quarter of patients with lymphomas had IFD before allo-HSCT. This result may be due to high pre-treatment burden in these patients, most of them were patients with Hodgkin lymphoma who underwent more than 6 lines of chemotherapy before allo-HSCT.
Our study has also shown that the cumulative incidence of relapse or progression of invasive fungal disease after allo-HSCT was 14.5%. The only risk factor for relapse or progression of IFD was lack of complete remission of the underlying disease at the moment of HSCT. That result corresponded to the earlier reported data [16], but we didn’t find any additional risk factors associated with bone marrow transplant procedure or antifungal treatment before allo-HSCT.
In the present study, we demonstrated that invasive fungal disease prior to the allo-HSCT did not impact on outcome of this treatment in children and adults. We suggest that there are several features that may have endow to obtained results.
Firstly, our study included allo-HSCT recipients who have been transplanted over recent years, in comparison with published studies [13-16, 20]. An overall better supportive care management was applied over last years, thus improving, specifically the outcome of allo-HSCT in patients with infectious complications including IFD. We believe that active diagnostic strategy and wide implementation of modern medications for secondary prophylaxis in our center played a role in improving the outcome of allo-HSCT in the patients with pre-existing IFD. It has been shown in several trials that secondary antifungal prophylaxis with voriconazole leads to considerably lower IA relapse rates as compared with those reported in historical controls, since Aspergillus spp. is a prevailing pathogen in pre-transplant IFD in our study [21-23].
Secondly, this study demonstrated the central role of the underlying disease status upon outcome of the allo-HSCT, and influence on the course of the infectious complications after HSCT, IFD in our case. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT. This hypothesis is supported by publications from a French-Belgium study group, demonstrating that the outcome of severe infectious complications in patients with hematological malignancies has been considerably improved during the last decade and is mostly determined by the status of the underlying disease [24-25].
Thirdly, our study has limitations due to relatively small study cohort from a single center data. That is why the result may be not accurate enough to evaluate the effect of IFD upon allo-HSCT outcome. At the same time, it reflects the situation during certain time which significantly affects the results obtained. Therefore, we cannot exclude the possibility that pre-existing IFD has a higher adverse impact on allo-HSCT outcome than our data may suggest.
In conclusion, we found out no significant impact upon important allo-HSCT transplant outcomes, such as survival, GvHD and relapse. Our data suggest that a history of IFD should not be considered a contraindication for allo-HSCT. We are currently continuous an observational prospective study to be able to more precisely investigate the impact of IFD on allo-HSCT.
Acknowledgments
The authors would like to acknowledge all medical staff at our University’ BMT clinic CIC725. Special thanks to our ICU department, our transplant nurses’ team for their particular care of our patients. Many thanks to specialists of Department of Clinical Microbiology at the First Pavlov State Medical University of Saint-Petersburg, especially to dr. Olga Pinegina and Chief of the Department, and special gratitude to patients and their relatives.
Conflict of interest
No conflict of interests is declared.
References
- Passweg JR, Baldomero H, Basak GW, Chabannon C, Corbacioglu S, Duarte R, Kuball J, Lankester A, Montoto S, de Latour RP, Snowden JA, Styczynski J, Yakoub-Agha I, Arat M, Mohty M, Kröger N; European Society for Blood and Marrow Transplantation (EBMT). The EBMT activity survey report 2017: a focus on allogeneic HCT for nonmalignant indications and on the use of non-HCT cell therapies. Bone Marrow Transplant 2019, Feb 6. doi: 10.1038/s41409-019-0465-9.
- Afanasyev BV, Zubarovskaya LS, Semenova EV, Ivanova NE, Alyanskiy AL, Morozova EV, Mikhailova NB, Darskaya EI, Estrina MA, Golovacheva AA, Babenko EV, Bondarenko SN, Ganapiev AA, Bogomolny MP. The experience in non-relative allogenic transplantation of stem hemopoietic cells in the clinic of bone marrow transplantation at I. P. Pavlov St. Petersburg Medical Academy. Terapevticheskii Arkhiv 2007, 79 (7):36-43 (In Russian).
- Bondarenko SN, Moiseev IS, Slesarchuk OA, Darskaya EI, Ekushev KA, Smirnova AG, Alyanskiy AL, Gindina TL, Babenko EV, Kuzmich EV, Semenova EV, Kulagin AD, Zubarovskaya LS, Afanasyev BV. Allogeneic hematopoietic stem cell transplantation in children and adults with acute lymphoblastic leukemia. Cell Ther Transplant. 2016, 5 (2):12-20.
- Afanasyev BV, Zubarovskaya LS, Moiseev IS. Allogeneic hematopoietic stem cell transplantation in children: now, problems and prospects. Russian Journal of Children Hematology and Oncology. 2015, 2: 28-42 (In Russian).
- Baron F, Labopin M, Peniket A, Jindra P, Afanasyev B, Sanz M.A, Deconinck E, Nagler A, Mohty M. Reduced-intensity conditioning with fludarabine and busulfan versus fludarabine and melphalan for patients with acute myeloid leukemia: A report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Cancer 2015; 121(7): 1048-1055.
- Moiseev IS, Pirogova OV, Babenko EV, Gindina TL, Darskaya EI, Morozova EV, Bondarenko SN, Afanasyev BV. Single-agent post-transplantation cyclophosphamide versus calcineurin-based graft-versus-host disease prophylaxis in matched related bone marrow transplantation. Cell Ther Transplant. 2017; 6 (4): 52-59.
- Bykova TA, Borovkova AS, Osipova AA, Ovechkina VN, Sheveleva PV, Nadzhafava KU, Yager VU, Paina OV, Kozhokar PV, Alyanskyi AL, Kulagin AD, Semenova EV, Smirnov BI, Zubarovskaya LS, Afanasyev BV. Acute GvHD prophylaxis with posttransplant cyclophosphamide after hematopoietic stem cell transplantation (HSCT) for non-malignant disorders. Pediatric Hematology/Oncology and Immunopathology 2018, 17 (2), pp. 51-58 (In Russian).
- Moiseev IS, Darskaya EI, Bykova TA, Morozova EV, Alyanskiy AL, Babenko EV, Bondarenko SN, Markova IV, Afanasyev BV. Different risk factors of acute and chronic graft-versus-host disease with conventional prophylaxis and posttransplantation cyclophosphamide in matched related and unrelated donor transplantation. Cell Ther Transplant. 2018; 7 (4): 29-37. DOI: 10.18620/ctt-1866-8836-2018-7-4-29-37.
- Shadrivova OV, Khostelidi SN, Chudinovskikh YA, Zabirov VS, Borzova YV, Desyatik EA, Volkova AG, Popova MO, Markova IV, Uspenskaya OS, Ruzhinskaya OS, Shneyder TV, Bogomolova TS, Ignatyeva SM, Zubarovskaya LS, Afanasyev BV, Klimko NN. Invasive aspergillosis and mucormycosis in oncohematological patients. Oncohematology 2018, 13(2):39-47. DOI: 10.17650/1818-8346-2018-13-2-39-47. (In Russian).
- Klimko NN, Khostelidi SN, Volkova AG, Popova MO, Bogomolova TS, Zubarovskaya LS, Kolbin AS, Medvedeva NV, Zuzgin IS, Simkin SM, Vasilyeva NV. Afanasyev BV. Mucormycosis in haematological patients: case report and results of prospective study in Saint Petersburg, Russia. Mycoses 2014, 57: 91-96. doi:10.1111/myc.12247.
- Teng JC, Slavin MA, Teh BW, Lingaratnam SM, Ananda-Rajah MR, Worth LJ, Seymour JF, Thursky KA. Epidemiology of invasive fungal disease in lymphoproliferative disorders. Haematologica. 2015; 100(11):e462-6. doi: 10.3324/haematol.2015.126698.
- Kontoyiannis DP, Marr KA, Park BJ, Alexander BD, Anaissie EJ, Walsh TJ, Ito J, Andes DR, Baddley JW, Brown JM, Brumble LM, Freifeld AG, Hadley S, Herwaldt LA, Kauffman CA, Knapp K, Lyon GM, Morrison VA, Papanicolaou G, Patterson TF, Perl TM, Schuster MG, Walker R, Wannemuehler KA, Wingard JR, Chiller TM, Pappas PG. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the transplant-associated infection surveillance network (TRANSNET) database. Clin Infect Dis. 2010, 50:1091–1100. DOI: 10.1086/651263.
- Martino R, Lopez R, Sureda A, Brunet S, Domingo-Albos A. Risk of reactivation of a recent invasive fungal infection in patients with hematological malignancies undergoing further intensive chemo-radiotherapy. A single-center experience and review of the literature. Haematologica. 1997; 82:297–304.
- Offner F, Cordonnier C, Ljungman P, Prentice HG, Engelhard D, De Bacquer D, Meunier F, De Pauw B. Impact of previous aspergillosis on the outcome of bone marrow transplantation. Clin Infect Dis. 1998, 26:1098–1103. DOI: 10.1086/520274.
- Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis 2002;34: 909-917. DOI: 10.1086/339202.
- Fukuda T, Boeckh M, Guthrie KA, Mattson DK, Owens S, Wald A, Sandmaier BM, Corey L, Storb RF, Marr KA. Invasive aspergillosis before allogeneic hematopoietic stem cell transplantation: 10-year experience at a single transplant center. Biol Blood Marrow Transplant. 2004; 10: 494-503. DOI: 10.1016/j.bbmt.2004.02.006.
- Maziarz RT, Brazauskas R, Chen M, McLeod AA, Martino R, Wingard JR, Aljurf M, Battiwalla M, Dvorak CC, Geroge B, Guinan EC, Hale GA, Lazarus HM, Lee JW, Liesveld JL, Ramanathan M, Reddy V, Savani BN, Smith FO, Strasfeld L, Taplitz RA, Ustun C, Boeckh MJ, Gea-Banacloche J, Lindemans CA, Auletta JJ, Riches ML. Pre-existing invasive fungal infection is not a contraindication for allogeneic HSCT for patients with hematologic malignancies: a CIBMTR study. Bone Marrow Transplant. 2017; 52(2):270-278. DOI: 10.1038/bmt.2016.259.
- Popova MO, Volkova A, Elias Soulaiman S, Vavilov V, Bondarenko S, Slesarchuk O, Smirnova A, Shadrivova O, Khostelidi S, Ignatyeva S, Bogomolova T, Zubarovskaya L, Klimko N, Afanasyev B. Allogeneic hematopoietic stem cell transplantation in patients with invasive aspergillosis. Bone Marrow Transplantation. 2015, Volume 50, Supplement 1, S33.
- Popova MO, Volkova AG, Soulaiman SE, Pinegina ON, Ignatyeva SM, Bogomolova TS, Smirnova AG, Vladovskaya M D, Bondarenko SN, Zubarovskaya LS, Klimko NN, Afanasyev BV. Outcome of allogeneic hematopoietic stem cell transplantation in patients with prior invasive aspergillosis. Blood. 2015; 126(23):3123; DOI: https://doi.org/
- Penack O, Tridello G, Hoek J, Socié G, Blaise D, Passweg J, Chevallier P, Craddock C, Milpied N, Veelken H, Maertens J, Ljungman P, Cornelissen J, Thiebaut-Bertrand A, Lioure B, Michallet M, Iacobelli S, Nagler A, Mohty M, Cesaro S. Influence of pre-existing invasive aspergillosis on allo-HSCT outcome: a retrospective EBMT analysis by the Infectious Diseases and Acute Leukemia Working Parties. Bone Marrow Transplant. 2016; 51(3):418-23. doi: 10.1038/bmt.2015.237.
- Allinson K, Kolve H, Gumbinger HG, Vormoor HJ, Ehlert K, Groll AH. Secondary antifungal prophylaxis in paediatric allogeneic haematopoietic stem cell recipients. J Antimicrob Chemother. 2008;61:734-742.
- Cordonnier C, Maury S, Pautas C, Bastie JN, Chehata S, Castaigne S, Kuentz M, Bretagne S, Ribaud P. Secondary antifungal prophylaxis with voriconazole to adhere to scheduled treatment in leukemic patients and stem cell transplant recipients. Bone Marrow Transplant. 2004;33(9):943-948.
- Cordonnier C, Rovira M, Maertens J, Olavarria E, Faucher C, Bilger K, Pigneux A, Cornely OA, Ullmann AJ, Bofarull RM, de la Cámara R, Weisser M, Liakopoulou E, Abecasis M, Heussel CP, Pineau M, Ljungman P, Einsele H. Voriconazole for secondary prophylaxis of invasive fungal infections in patients with allogeneic stem cell transplants recipients: results of the VOSIFI Study Group; Infectious Diseases Working Party, European Group for Blood and Marrow Transplantation. Haematologica. 2010; 95(10):1762-1768. doi:10.3324/haematol.2009.020073.
- Azoulay E, Mokart D, Pène F, Lambert J, Kouatchet A, Mayaux J, Vincent F, Nyunga M, Bruneel F, Laisne LM, Rabbat A, Lebert C, Perez P, Chaize M, Renault A, Meert AP, Benoit D, Hamidfar R, Jourdain M, Darmon M, Schlemmer B, Chevret S, Lemiale V. Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium – a groupe de recherche respiratoire en reanimation onco-hematologique study. J Clin Oncol. 2013;31(22):2810-2818. doi: 10.1200/JCO.2012.47.2365.
- Legrand M, Max A, Peigne V, Mariotte E, Canet E, Debrumetz A, Lemiale V, Seguin A, Darmon M, Schlemmer B, Azoulay E. Survival in neutropenic patients with severe sepsis or septic shock. Crit Care Med. 2012;40(1):43-9. doi: 10.1097/CCM.0b013e31822b50c2.
Марина О. Попова 1, Алиса Г. Волкова 1, Инна В. Маркова 1, Оксана В. Айзсилниекс 1, Юлия А. Рогачева 1, Анастасия С. Фролова 1, Александр Н. Швецов 1, Илья Ю. Николаев 1, Светлана М. Игнатьева 2, Татьяна С. Богомолова 2, Асмик Г. Геворгян 1, Олеся В. Паина 1, Татьяна А. Быкова 1, Елена И. Дарская 1, Мария В. Владовская 1, Иван С. Моисеев 1, Людмила С. Зубаровская 1, Николай Н. Климко 1,2, Борис В. Афанасьев 1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23051" ["VALUE"]=> array(2) { ["TEXT"]=> string(690) "<p><sup>1</sup> НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургсий государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия<br> <sup>2</sup> НИИ Медицинской микологии им. П. Н. Кашкина, Северо-западный государственный медицинский университет им. И. И. Мечникова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(648) "1 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургсий государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 НИИ Медицинской микологии им. П. Н. Кашкина, Северо-западный государственный медицинский университет им. И. И. Мечникова, Санкт-Петербург, Россия
Внедрение новых противогрибковых средств и диагностических процедур улучшило прогноз гематологических пациентов с инвазивными микозами (ИМ). Увеличилось число пациентов с ИМ, кандидатов на аллогенную трансплантацию гемопоэтических стволовых клеток (алло-ТГСК). Роль ИМ, развившихся до алло-ТГСК, по-прежнему не определена. Нет опубликованных данных о результатах алло-ТГСК у педиатрических пациентов с предшествующим ИМ. Цель исследования – оценить влияние предшествующего ИМ на результаты алло-ТГСК.
Пациенты и методы
В проспективное исследование были включены 504 реципиента алло-ТГСК в период с января 2013 года по июль 2016 года. Средний возраст составил 24 года (2 месяца – 76 лет), дети (<18 лет) – 164, взрослые – 340, мужчины – 52%. Преимущественно пациенты с диагнозом острый лейкоз группы высокого риска (74,6%). Алло-ТГСК от неродственного совместимого донора были выполнены у 58,5%, совместимого родственного донора – 22,5%, гаплоидентичного – 19%, преимущественно с использованием режима кондиционирования со сниженной интенсивностью (67%). Непосредственно перед алло-ТГСК всем пациентам с обнаруженными изменениями ткани легких, в результате компьютерной томографии органов грудной клетки, выполнялась бронхоскопия с исследованием жидкости бронхоальвеолярного лаважа: микроскопии, культуры и теста на галактоманнан. Для диагностики доказанного и вероятного ИМ и оценки ответа на терапию были использованы критерии EORTC/MSG 2008. «Активный ИМ» – ИМ, диагностированный непосредственно перед трансплантацией. Медиана наблюдения составила 20 месяцев. Основными конечными точками были общая выживаемость (ОВ), частота рецидива или прогрессирования ИМ после алло-ТГСК; вторичные точки – частота острой и хронической РТПХ, рецидива основного заболевания.
Результаты
Частота ИМ до алло-ТГСК составила 15% (n=76). Согласно критериям EORTS/MSG 2008, 90,8% пациентов имели вероятный и 9,2% доказанный ИМ. Этиология ИМ до трансплантации: инвазивный аспергиллез (ИА) – 75%, инвазивный кандидоз (ИК) – 13%, мукормикоз (М) – 4%, пневмоцистная пневмония (ПП) – 1,3% и комбинация ИА с М диагностирована у 2 пациентов, с ИК – 1, с ПП – 1. Основным органом поражения были легкие – 95%, другие локализации, преимущественно в сочетании с вовлечением легких: синусы – 9%, селезенка – 6%, печень – 6%, и мягкие ткани – 3%. Противогрибковая терапия перед алло-ТГСК применялась у 75% пациентов с медианой продолжительности – 2 месяца. Полный ответ на противогрибковую терапию был достигнут у 38,2% пациентов, частичный ответ или стабилизация – 35,5%, а у 26,3% пациентов был «активный ИМ». После алло-ТГСК все пациенты получали противогрибковую терапию или вторичную профилактику в соответствии с этиологией ИМ. Кумулятивная частота рецидива или прогрессирования ИМ после алло-ТГСК составила 14,5%. Отсутствие ремиссии основного заболевания в момент трансплантации был единственным фактором риска рецидива или прогрессирования ИМ после алло-ТГСК (11,5% против 21,1%, p=0,03). Существенных различий в кумулятивной частоте острой (p=0,28), хронической РТПХ (p=0,25) и рецидива (p=0,31) не было обнаружено в сравнении с группой пациентов без ИМ в анамнезе. 3-летняя ОВ после алло-ТГСК составила 67,5%. Общая выживаемость у реципиентов аллоТГСК без ИМ и имевших ИМ в анамнезе статистически не различалась во всех группах (60,5% против 68,7%, р=0,1), как отдельно у детей (50,0% против 57,4% , P=0,32) так и у взрослых (63,3% против 74,6%, p=0,09). Наихудший результат наблюдался у пациентов с «активным ИМ» и отсутствием ремиссии основного заболевания на момент трансплантации (3-летняя ОВ – 20%, р <0,001). Однако у пациентов с «активным ИМ» и ремиссией основного заболевания ОВ была аналогична выживаемости пациентов без ИМ в ананмнезе (80% против 68,7%, р=0,57).
Выводы
Пятнадцать процентов реципиентов алло-ТГСК имели инвазивный микоз в анамнезе. Кумулятивная частота рецидива или прогрессирования инвазивных микозов после алло-ТГСК составила 14,5%. Предшествующий инвазивный микоз не оказывал существенного влияния на результаты трансплантации и общую выживаемость детей и взрослых после алло-ТГСК. Отсутствие ремиссии основного заболевания на момент трансплантации было единственным фактором риска рецидива или прогрессирования инвазивного микоза, и ухудшения результатов алло-ТГСК.
Ключевые слова
Предшествующие инвазивные микозы, аллогенная трансплантация гемопоэтических стволовых клеток, дети и взрослые, клинические исходы.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23026" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-17-25" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-17-25" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23073" ["VALUE"]=> array(2) { ["TEXT"]=> string(877) "<p>Marina O. Popova <sup>1</sup>, Alisa G. Volkova <sup>1</sup>, Inna V. Markova <sup>1</sup>, Oksana V. Ayzsilnieks <sup>1</sup>, Yulia A. Rogacheva <sup>1</sup>, Anastasia S. Frolova <sup>1</sup>, Aleksandr N. Shvetcov <sup>1</sup>, Ilya Y. Nikolaev <sup>1</sup>, Svetlana M. Ignatyeva <sup>2</sup>, Tatyana S. Bogomolova <sup>2</sup>, Asmic G. Gevorgian <sup>1</sup>, Olesya V. Paina <sup>1</sup>, Tatiana A. Bykova <sup>1</sup>, Elena I. Darskaya <sup>1</sup>, Maria V. Vladovskaya <sup>1</sup>, Ivan S. Moiseev <sup>1</sup>, Ludmila S. Zubarovskaya <sup>1</sup>, Nikolay N. Klimko <sup>1,2</sup>, Boris V. Afanasyev <sup>1</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(637) "Marina O. Popova 1, Alisa G. Volkova 1, Inna V. Markova 1, Oksana V. Ayzsilnieks 1, Yulia A. Rogacheva 1, Anastasia S. Frolova 1, Aleksandr N. Shvetcov 1, Ilya Y. Nikolaev 1, Svetlana M. Ignatyeva 2, Tatyana S. Bogomolova 2, Asmic G. Gevorgian 1, Olesya V. Paina 1, Tatiana A. Bykova 1, Elena I. Darskaya 1, Maria V. Vladovskaya 1, Ivan S. Moiseev 1, Ludmila S. Zubarovskaya 1, Nikolay N. Klimko 1,2, Boris V. Afanasyev 1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23074" ["VALUE"]=> array(2) { ["TEXT"]=> string(419) "<p><sup>1</sup> Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br> <sup>2</sup> Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(377) "1 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia
Invasive fungal diseases (IFD) are a major cause of morbidity and mortality in hematological patients, but prognosis of IFD has improved recently, due to introduction of new antifungals and efficient diagnostic procedures. Number of patients with IFD who are candidates for allogeneic hematopoietic stem cell transplant (allo-HSCT) increased. However, publications on the field are limited and there are no data on results of pediatric allo-HSCT patients with prior IFD. This study focuses on the outcomes of allo-HSCT in children and adults with prior IFD.
Patients and methods
In a prospective study, 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016. The median age was 24 y.o. [2 months to 76 years] including 164 children (<18 yo) and 340 adults. The cohort included 52% male patients. Most patients (74.6%) were diagnosed with high-risk acute leukemia. Allo-HSCT from HLA-matched unrelated donors (MUD) was performed in 58.5%, from matched related donors (MRD), 22.5%; haploidentical HSCT was performed in 19% of patients, predominantly with RIC (67%). EORTC/MSG 2008 criteria for diagnosis and response to therapy were used. In the patients with pre-transplant lung lesions detected by CT scan, bronchoscopy with BAL was used. “Active IFD” means IFD diagnosed just before HSCT.
Results
Incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria, 90.8% of patients had probable and 9.2% presented with proven IFD. Etiology of IFD prior to HSCT was as follows: invasive aspergillosis (IA), 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; Pneumocystis pneumoniae (PCP), 1.3%, and combination of IA with Mu (2 cases), IC (n=1), PCP (n=1). The main sites of infection were lungs (95%), other localizations were predominantly combined with lung involvement: sinuses (9%), spleen (6%), liver (6%), and soft tissues (3%). Antifungal therapy before allo-HSCT was used in 75% patients with median duration of 2 months. Complete response to antifungal therapy was observed in 38.2% of the cases, partial response or stabilization was achieved in 35.5%, and “active IFD” was detected in 26.3% of the patients. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology. Cumulative incidence of relapse or progression of IFD after allo-HSCT was observed in 14.5%. Active underlying disease (hematology malignancy) at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% vs 21.1%, p=0,03). We detected no significant differences in the cumulative incidence of acute, chronic GVHD and relapse in the study group as compared to the patients without history of IFD. 3-year overall survival (OS) after allo-HSCT was 67.5%. The impact of prior IFD on overall survival in allo-HSCT recipients was not statistically significant for the entire group (60.5% vs 68.7%, p=0.1), and, separately, for children (50.0% vs 57.4%, p=0,3) and adults (63.3% vs 74.6%, p=0.09). The worst outcome was observed in the patients with “active IFD” and active underlying disease at the moment of HSCT (3-year OS was 20%, p<0.001 compared to patients without history of IFD). However, in the patients with “active IFD” and remission of underlying disease, OS value was similar to survival rate of patients without history of IFD (80% vs 68.7%, p=0.2).
Conclusion
Incidence of IFD before allo-HSCT was 15%. Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5%. Prior IFD had no significant impact on transplant-related complications and overall survival in children and adults undergoing allo-HSCT. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT.
Keywords
Invasive fungal disease, pre-existing IFD, allogeneic hematopoietic stem cell transplantation, children and adults, clinical outcomes.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23027" ["VALUE"]=> string(121) "Outcomes of allogeneic hematopoietic stem cell transplantation in children and adults with prior invasive fungal diseases" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(121) "Outcomes of allogeneic hematopoietic stem cell transplantation in children and adults with prior invasive fungal diseases" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> &array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23053" ["VALUE"]=> string(4) "1662" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1662" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23076" ["VALUE"]=> string(4) "1663" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1663" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(12) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23073" ["VALUE"]=> array(2) { ["TEXT"]=> string(877) "<p>Marina O. Popova <sup>1</sup>, Alisa G. Volkova <sup>1</sup>, Inna V. Markova <sup>1</sup>, Oksana V. Ayzsilnieks <sup>1</sup>, Yulia A. Rogacheva <sup>1</sup>, Anastasia S. Frolova <sup>1</sup>, Aleksandr N. Shvetcov <sup>1</sup>, Ilya Y. Nikolaev <sup>1</sup>, Svetlana M. Ignatyeva <sup>2</sup>, Tatyana S. Bogomolova <sup>2</sup>, Asmic G. Gevorgian <sup>1</sup>, Olesya V. Paina <sup>1</sup>, Tatiana A. Bykova <sup>1</sup>, Elena I. Darskaya <sup>1</sup>, Maria V. Vladovskaya <sup>1</sup>, Ivan S. Moiseev <sup>1</sup>, Ludmila S. Zubarovskaya <sup>1</sup>, Nikolay N. Klimko <sup>1,2</sup>, Boris V. Afanasyev <sup>1</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(637) "Marina O. Popova 1, Alisa G. Volkova 1, Inna V. Markova 1, Oksana V. Ayzsilnieks 1, Yulia A. Rogacheva 1, Anastasia S. Frolova 1, Aleksandr N. Shvetcov 1, Ilya Y. Nikolaev 1, Svetlana M. Ignatyeva 2, Tatyana S. Bogomolova 2, Asmic G. Gevorgian 1, Olesya V. Paina 1, Tatiana A. Bykova 1, Elena I. Darskaya 1, Maria V. Vladovskaya 1, Ivan S. Moiseev 1, Ludmila S. Zubarovskaya 1, Nikolay N. Klimko 1,2, Boris V. Afanasyev 1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(637) "Marina O. Popova 1, Alisa G. Volkova 1, Inna V. Markova 1, Oksana V. Ayzsilnieks 1, Yulia A. Rogacheva 1, Anastasia S. Frolova 1, Aleksandr N. Shvetcov 1, Ilya Y. Nikolaev 1, Svetlana M. Ignatyeva 2, Tatyana S. Bogomolova 2, Asmic G. Gevorgian 1, Olesya V. Paina 1, Tatiana A. Bykova 1, Elena I. Darskaya 1, Maria V. Vladovskaya 1, Ivan S. Moiseev 1, Ludmila S. Zubarovskaya 1, Nikolay N. Klimko 1,2, Boris V. Afanasyev 1
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23075" ["VALUE"]=> array(2) { ["TEXT"]=> string(4452) "<p style="text-align:justify";>Invasive fungal diseases (IFD) are a major cause of morbidity and mortality in hematological patients, but prognosis of IFD has improved recently, due to introduction of new antifungals and efficient diagnostic procedures. Number of patients with IFD who are candidates for allogeneic hematopoietic stem cell transplant (allo-HSCT) increased. However, publications on the field are limited and there are no data on results of pediatric allo-HSCT patients with prior IFD. This study focuses on the outcomes of allo-HSCT in children and adults with prior IFD.</p> <h3>Patients and methods</h3> <p style="text-align:justify";>In a prospective study, 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016. The median age was 24 y.o. [2 months to 76 years] including 164 children (<18 yo) and 340 adults. The cohort included 52% male patients. Most patients (74.6%) were diagnosed with high-risk acute leukemia. Allo-HSCT from HLA-matched unrelated donors (MUD) was performed in 58.5%, from matched related donors (MRD), 22.5%; haploidentical HSCT was performed in 19% of patients, predominantly with RIC (67%). EORTC/MSG 2008 criteria for diagnosis and response to therapy were used. In the patients with pre-transplant lung lesions detected by CT scan, bronchoscopy with BAL was used. “Active IFD” means IFD diagnosed just before HSCT.</p> <h3>Results</h3> <p style="text-align:justify";>Incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria, 90.8% of patients had probable and 9.2% presented with proven IFD. Etiology of IFD prior to HSCT was as follows: invasive aspergillosis (IA), 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; <i>Pneumocystis pneumoniae</i> (PCP), 1.3%, and combination of IA with Mu (2 cases), IC (n=1), PCP (n=1). The main sites of infection were lungs (95%), other localizations were predominantly combined with lung involvement: sinuses (9%), spleen (6%), liver (6%), and soft tissues (3%). Antifungal therapy before allo-HSCT was used in 75% patients with median duration of 2 months. Complete response to antifungal therapy was observed in 38.2% of the cases, partial response or stabilization was achieved in 35.5%, and “active IFD” was detected in 26.3% of the patients. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology. Cumulative incidence of relapse or progression of IFD after allo-HSCT was observed in 14.5%. Active underlying disease (hematology malignancy) at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% <i>vs</i> 21.1%, p=0,03). We detected no significant differences in the cumulative incidence of acute, chronic GVHD and relapse in the study group as compared to the patients without history of IFD. 3-year overall survival (OS) after allo-HSCT was 67.5%. The impact of prior IFD on overall survival in allo-HSCT recipients was not statistically significant for the entire group (60.5% <i>vs</i> 68.7%, p=0.1), and, separately, for children (50.0% <i>vs</i> 57.4%, p=0,3) and adults (63.3% <i>vs</i> 74.6%, p=0.09). The worst outcome was observed in the patients with “active IFD” and active underlying disease at the moment of HSCT (3-year OS was 20%, p<0.001 compared to patients without history of IFD). However, in the patients with “active IFD” and remission of underlying disease, OS value was similar to survival rate of patients without history of IFD (80% <i>vs</i> 68.7%, p=0.2). </p> <h3>Conclusion</h3> <p style="text-align:justify";>Incidence of IFD before allo-HSCT was 15%. Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5%. Prior IFD had no significant impact on transplant-related complications and overall survival in children and adults undergoing allo-HSCT. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT.</p> <h2>Keywords</h2> <p style="text-align:justify";>Invasive fungal disease, pre-existing IFD, allogeneic hematopoietic stem cell transplantation, children and adults, clinical outcomes.</p> " ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(4216) "Invasive fungal diseases (IFD) are a major cause of morbidity and mortality in hematological patients, but prognosis of IFD has improved recently, due to introduction of new antifungals and efficient diagnostic procedures. Number of patients with IFD who are candidates for allogeneic hematopoietic stem cell transplant (allo-HSCT) increased. However, publications on the field are limited and there are no data on results of pediatric allo-HSCT patients with prior IFD. This study focuses on the outcomes of allo-HSCT in children and adults with prior IFD.
Patients and methods
In a prospective study, 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016. The median age was 24 y.o. [2 months to 76 years] including 164 children (<18 yo) and 340 adults. The cohort included 52% male patients. Most patients (74.6%) were diagnosed with high-risk acute leukemia. Allo-HSCT from HLA-matched unrelated donors (MUD) was performed in 58.5%, from matched related donors (MRD), 22.5%; haploidentical HSCT was performed in 19% of patients, predominantly with RIC (67%). EORTC/MSG 2008 criteria for diagnosis and response to therapy were used. In the patients with pre-transplant lung lesions detected by CT scan, bronchoscopy with BAL was used. “Active IFD” means IFD diagnosed just before HSCT.
Results
Incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria, 90.8% of patients had probable and 9.2% presented with proven IFD. Etiology of IFD prior to HSCT was as follows: invasive aspergillosis (IA), 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; Pneumocystis pneumoniae (PCP), 1.3%, and combination of IA with Mu (2 cases), IC (n=1), PCP (n=1). The main sites of infection were lungs (95%), other localizations were predominantly combined with lung involvement: sinuses (9%), spleen (6%), liver (6%), and soft tissues (3%). Antifungal therapy before allo-HSCT was used in 75% patients with median duration of 2 months. Complete response to antifungal therapy was observed in 38.2% of the cases, partial response or stabilization was achieved in 35.5%, and “active IFD” was detected in 26.3% of the patients. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology. Cumulative incidence of relapse or progression of IFD after allo-HSCT was observed in 14.5%. Active underlying disease (hematology malignancy) at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% vs 21.1%, p=0,03). We detected no significant differences in the cumulative incidence of acute, chronic GVHD and relapse in the study group as compared to the patients without history of IFD. 3-year overall survival (OS) after allo-HSCT was 67.5%. The impact of prior IFD on overall survival in allo-HSCT recipients was not statistically significant for the entire group (60.5% vs 68.7%, p=0.1), and, separately, for children (50.0% vs 57.4%, p=0,3) and adults (63.3% vs 74.6%, p=0.09). The worst outcome was observed in the patients with “active IFD” and active underlying disease at the moment of HSCT (3-year OS was 20%, p<0.001 compared to patients without history of IFD). However, in the patients with “active IFD” and remission of underlying disease, OS value was similar to survival rate of patients without history of IFD (80% vs 68.7%, p=0.2).
Conclusion
Incidence of IFD before allo-HSCT was 15%. Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5%. Prior IFD had no significant impact on transplant-related complications and overall survival in children and adults undergoing allo-HSCT. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT.
Keywords
Invasive fungal disease, pre-existing IFD, allogeneic hematopoietic stem cell transplantation, children and adults, clinical outcomes.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(4216) "Invasive fungal diseases (IFD) are a major cause of morbidity and mortality in hematological patients, but prognosis of IFD has improved recently, due to introduction of new antifungals and efficient diagnostic procedures. Number of patients with IFD who are candidates for allogeneic hematopoietic stem cell transplant (allo-HSCT) increased. However, publications on the field are limited and there are no data on results of pediatric allo-HSCT patients with prior IFD. This study focuses on the outcomes of allo-HSCT in children and adults with prior IFD.
Patients and methods
In a prospective study, 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016. The median age was 24 y.o. [2 months to 76 years] including 164 children (<18 yo) and 340 adults. The cohort included 52% male patients. Most patients (74.6%) were diagnosed with high-risk acute leukemia. Allo-HSCT from HLA-matched unrelated donors (MUD) was performed in 58.5%, from matched related donors (MRD), 22.5%; haploidentical HSCT was performed in 19% of patients, predominantly with RIC (67%). EORTC/MSG 2008 criteria for diagnosis and response to therapy were used. In the patients with pre-transplant lung lesions detected by CT scan, bronchoscopy with BAL was used. “Active IFD” means IFD diagnosed just before HSCT.
Results
Incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria, 90.8% of patients had probable and 9.2% presented with proven IFD. Etiology of IFD prior to HSCT was as follows: invasive aspergillosis (IA), 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; Pneumocystis pneumoniae (PCP), 1.3%, and combination of IA with Mu (2 cases), IC (n=1), PCP (n=1). The main sites of infection were lungs (95%), other localizations were predominantly combined with lung involvement: sinuses (9%), spleen (6%), liver (6%), and soft tissues (3%). Antifungal therapy before allo-HSCT was used in 75% patients with median duration of 2 months. Complete response to antifungal therapy was observed in 38.2% of the cases, partial response or stabilization was achieved in 35.5%, and “active IFD” was detected in 26.3% of the patients. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology. Cumulative incidence of relapse or progression of IFD after allo-HSCT was observed in 14.5%. Active underlying disease (hematology malignancy) at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% vs 21.1%, p=0,03). We detected no significant differences in the cumulative incidence of acute, chronic GVHD and relapse in the study group as compared to the patients without history of IFD. 3-year overall survival (OS) after allo-HSCT was 67.5%. The impact of prior IFD on overall survival in allo-HSCT recipients was not statistically significant for the entire group (60.5% vs 68.7%, p=0.1), and, separately, for children (50.0% vs 57.4%, p=0,3) and adults (63.3% vs 74.6%, p=0.09). The worst outcome was observed in the patients with “active IFD” and active underlying disease at the moment of HSCT (3-year OS was 20%, p<0.001 compared to patients without history of IFD). However, in the patients with “active IFD” and remission of underlying disease, OS value was similar to survival rate of patients without history of IFD (80% vs 68.7%, p=0.2).
Conclusion
Incidence of IFD before allo-HSCT was 15%. Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5%. Prior IFD had no significant impact on transplant-related complications and overall survival in children and adults undergoing allo-HSCT. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT.
Keywords
Invasive fungal disease, pre-existing IFD, allogeneic hematopoietic stem cell transplantation, children and adults, clinical outcomes.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23026" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-17-25" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-17-25" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-17-25" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23027" ["VALUE"]=> string(121) "Outcomes of allogeneic hematopoietic stem cell transplantation in children and adults with prior invasive fungal diseases" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(121) "Outcomes of allogeneic hematopoietic stem cell transplantation in children and adults with prior invasive fungal diseases" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(121) "Outcomes of allogeneic hematopoietic stem cell transplantation in children and adults with prior invasive fungal diseases" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23074" ["VALUE"]=> array(2) { ["TEXT"]=> string(419) "<p><sup>1</sup> Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br> <sup>2</sup> Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(377) "1 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia
1 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia
Марина О. Попова 1, Алиса Г. Волкова 1, Инна В. Маркова 1, Оксана В. Айзсилниекс 1, Юлия А. Рогачева 1, Анастасия С. Фролова 1, Александр Н. Швецов 1, Илья Ю. Николаев 1, Светлана М. Игнатьева 2, Татьяна С. Богомолова 2, Асмик Г. Геворгян 1, Олеся В. Паина 1, Татьяна А. Быкова 1, Елена И. Дарская 1, Мария В. Владовская 1, Иван С. Моисеев 1, Людмила С. Зубаровская 1, Николай Н. Климко 1,2, Борис В. Афанасьев 1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(907) "Марина О. Попова 1, Алиса Г. Волкова 1, Инна В. Маркова 1, Оксана В. Айзсилниекс 1, Юлия А. Рогачева 1, Анастасия С. Фролова 1, Александр Н. Швецов 1, Илья Ю. Николаев 1, Светлана М. Игнатьева 2, Татьяна С. Богомолова 2, Асмик Г. Геворгян 1, Олеся В. Паина 1, Татьяна А. Быкова 1, Елена И. Дарская 1, Мария В. Владовская 1, Иван С. Моисеев 1, Людмила С. Зубаровская 1, Николай Н. Климко 1,2, Борис В. Афанасьев 1
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23004" ["VALUE"]=> string(22) "07/30/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "07/30/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "07/30/2019 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23005" ["VALUE"]=> string(22) "08/09/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "08/09/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "08/09/2019 12:00:00 am" } ["CONTACT"]=> array(38) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23006" ["VALUE"]=> string(4) "1241" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1241" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(60) "Marina O. Popova" ["LINK_ELEMENT_VALUE"]=> bool(false) } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23052" ["VALUE"]=> array(2) { ["TEXT"]=> string(8272) "<p style="text-align:justify";>Внедрение новых противогрибковых средств и диагностических процедур улучшило прогноз гематологических пациентов с инвазивными микозами (ИМ). Увеличилось число пациентов с ИМ, кандидатов на аллогенную трансплантацию гемопоэтических стволовых клеток (алло-ТГСК). Роль ИМ, развившихся до алло-ТГСК, по-прежнему не определена. Нет опубликованных данных о результатах алло-ТГСК у педиатрических пациентов с предшествующим ИМ. Цель исследования – оценить влияние предшествующего ИМ на результаты алло-ТГСК. </p> <h3>Пациенты и методы</h3> <p style="text-align:justify";>В проспективное исследование были включены 504 реципиента алло-ТГСК в период с января 2013 года по июль 2016 года. Средний возраст составил 24 года (2 месяца – 76 лет), дети (<18 лет) – 164, взрослые – 340, мужчины – 52%. Преимущественно пациенты с диагнозом острый лейкоз группы высокого риска (74,6%). Алло-ТГСК от неродственного совместимого донора были выполнены у 58,5%, совместимого родственного донора – 22,5%, гаплоидентичного – 19%, преимущественно с использованием режима кондиционирования со сниженной интенсивностью (67%). Непосредственно перед алло-ТГСК всем пациентам с обнаруженными изменениями ткани легких, в результате компьютерной томографии органов грудной клетки, выполнялась бронхоскопия с исследованием жидкости бронхоальвеолярного лаважа: микроскопии, культуры и теста на галактоманнан. Для диагностики доказанного и вероятного ИМ и оценки ответа на терапию были использованы критерии EORTC/MSG 2008. «Активный ИМ» – ИМ, диагностированный непосредственно перед трансплантацией. Медиана наблюдения составила 20 месяцев. Основными конечными точками были общая выживаемость (ОВ), частота рецидива или прогрессирования ИМ после алло-ТГСК; вторичные точки – частота острой и хронической РТПХ, рецидива основного заболевания.</p> <h3>Результаты</h3> <p style="text-align:justify";>Частота ИМ до алло-ТГСК составила 15% (n=76). Согласно критериям EORTS/MSG 2008, 90,8% пациентов имели вероятный и 9,2% доказанный ИМ. Этиология ИМ до трансплантации: инвазивный аспергиллез (ИА) – 75%, инвазивный кандидоз (ИК) – 13%, мукормикоз (М) – 4%, пневмоцистная пневмония (ПП) – 1,3% и комбинация ИА с М диагностирована у 2 пациентов, с ИК – 1, с ПП – 1. Основным органом поражения были легкие – 95%, другие локализации, преимущественно в сочетании с вовлечением легких: синусы – 9%, селезенка – 6%, печень – 6%, и мягкие ткани – 3%. Противогрибковая терапия перед алло-ТГСК применялась у 75% пациентов с медианой продолжительности – 2 месяца. Полный ответ на противогрибковую терапию был достигнут у 38,2% пациентов, частичный ответ или стабилизация – 35,5%, а у 26,3% пациентов был «активный ИМ». После алло-ТГСК все пациенты получали противогрибковую терапию или вторичную профилактику в соответствии с этиологией ИМ. Кумулятивная частота рецидива или прогрессирования ИМ после алло-ТГСК составила 14,5%. Отсутствие ремиссии основного заболевания в момент трансплантации был единственным фактором риска рецидива или прогрессирования ИМ после алло-ТГСК (11,5% против 21,1%, p=0,03). Существенных различий в кумулятивной частоте острой (p=0,28), хронической РТПХ (p=0,25) и рецидива (p=0,31) не было обнаружено в сравнении с группой пациентов без ИМ в анамнезе. 3-летняя ОВ после алло-ТГСК составила 67,5%. Общая выживаемость у реципиентов аллоТГСК без ИМ и имевших ИМ в анамнезе статистически не различалась во всех группах (60,5% против 68,7%, р=0,1), как отдельно у детей (50,0% против 57,4% , P=0,32) так и у взрослых (63,3% против 74,6%, p=0,09). Наихудший результат наблюдался у пациентов с «активным ИМ» и отсутствием ремиссии основного заболевания на момент трансплантации (3-летняя ОВ – 20%, р <0,001). Однако у пациентов с «активным ИМ» и ремиссией основного заболевания ОВ была аналогична выживаемости пациентов без ИМ в ананмнезе (80% против 68,7%, р=0,57).</p> <h3>Выводы</h3> <p style="text-align:justify";>Пятнадцать процентов реципиентов алло-ТГСК имели инвазивный микоз в анамнезе. Кумулятивная частота рецидива или прогрессирования инвазивных микозов после алло-ТГСК составила 14,5%. Предшествующий инвазивный микоз не оказывал существенного влияния на результаты трансплантации и общую выживаемость детей и взрослых после алло-ТГСК. Отсутствие ремиссии основного заболевания на момент трансплантации было единственным фактором риска рецидива или прогрессирования инвазивного микоза, и ухудшения результатов алло-ТГСК.</p> <h2>Ключевые слова</h2> <p style="text-align:justify";>Предшествующие инвазивные микозы, аллогенная трансплантация гемопоэтических стволовых клеток, дети и взрослые, клинические исходы.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(8108) "Внедрение новых противогрибковых средств и диагностических процедур улучшило прогноз гематологических пациентов с инвазивными микозами (ИМ). Увеличилось число пациентов с ИМ, кандидатов на аллогенную трансплантацию гемопоэтических стволовых клеток (алло-ТГСК). Роль ИМ, развившихся до алло-ТГСК, по-прежнему не определена. Нет опубликованных данных о результатах алло-ТГСК у педиатрических пациентов с предшествующим ИМ. Цель исследования – оценить влияние предшествующего ИМ на результаты алло-ТГСК.
Пациенты и методы
В проспективное исследование были включены 504 реципиента алло-ТГСК в период с января 2013 года по июль 2016 года. Средний возраст составил 24 года (2 месяца – 76 лет), дети (<18 лет) – 164, взрослые – 340, мужчины – 52%. Преимущественно пациенты с диагнозом острый лейкоз группы высокого риска (74,6%). Алло-ТГСК от неродственного совместимого донора были выполнены у 58,5%, совместимого родственного донора – 22,5%, гаплоидентичного – 19%, преимущественно с использованием режима кондиционирования со сниженной интенсивностью (67%). Непосредственно перед алло-ТГСК всем пациентам с обнаруженными изменениями ткани легких, в результате компьютерной томографии органов грудной клетки, выполнялась бронхоскопия с исследованием жидкости бронхоальвеолярного лаважа: микроскопии, культуры и теста на галактоманнан. Для диагностики доказанного и вероятного ИМ и оценки ответа на терапию были использованы критерии EORTC/MSG 2008. «Активный ИМ» – ИМ, диагностированный непосредственно перед трансплантацией. Медиана наблюдения составила 20 месяцев. Основными конечными точками были общая выживаемость (ОВ), частота рецидива или прогрессирования ИМ после алло-ТГСК; вторичные точки – частота острой и хронической РТПХ, рецидива основного заболевания.
Результаты
Частота ИМ до алло-ТГСК составила 15% (n=76). Согласно критериям EORTS/MSG 2008, 90,8% пациентов имели вероятный и 9,2% доказанный ИМ. Этиология ИМ до трансплантации: инвазивный аспергиллез (ИА) – 75%, инвазивный кандидоз (ИК) – 13%, мукормикоз (М) – 4%, пневмоцистная пневмония (ПП) – 1,3% и комбинация ИА с М диагностирована у 2 пациентов, с ИК – 1, с ПП – 1. Основным органом поражения были легкие – 95%, другие локализации, преимущественно в сочетании с вовлечением легких: синусы – 9%, селезенка – 6%, печень – 6%, и мягкие ткани – 3%. Противогрибковая терапия перед алло-ТГСК применялась у 75% пациентов с медианой продолжительности – 2 месяца. Полный ответ на противогрибковую терапию был достигнут у 38,2% пациентов, частичный ответ или стабилизация – 35,5%, а у 26,3% пациентов был «активный ИМ». После алло-ТГСК все пациенты получали противогрибковую терапию или вторичную профилактику в соответствии с этиологией ИМ. Кумулятивная частота рецидива или прогрессирования ИМ после алло-ТГСК составила 14,5%. Отсутствие ремиссии основного заболевания в момент трансплантации был единственным фактором риска рецидива или прогрессирования ИМ после алло-ТГСК (11,5% против 21,1%, p=0,03). Существенных различий в кумулятивной частоте острой (p=0,28), хронической РТПХ (p=0,25) и рецидива (p=0,31) не было обнаружено в сравнении с группой пациентов без ИМ в анамнезе. 3-летняя ОВ после алло-ТГСК составила 67,5%. Общая выживаемость у реципиентов аллоТГСК без ИМ и имевших ИМ в анамнезе статистически не различалась во всех группах (60,5% против 68,7%, р=0,1), как отдельно у детей (50,0% против 57,4% , P=0,32) так и у взрослых (63,3% против 74,6%, p=0,09). Наихудший результат наблюдался у пациентов с «активным ИМ» и отсутствием ремиссии основного заболевания на момент трансплантации (3-летняя ОВ – 20%, р <0,001). Однако у пациентов с «активным ИМ» и ремиссией основного заболевания ОВ была аналогична выживаемости пациентов без ИМ в ананмнезе (80% против 68,7%, р=0,57).
Выводы
Пятнадцать процентов реципиентов алло-ТГСК имели инвазивный микоз в анамнезе. Кумулятивная частота рецидива или прогрессирования инвазивных микозов после алло-ТГСК составила 14,5%. Предшествующий инвазивный микоз не оказывал существенного влияния на результаты трансплантации и общую выживаемость детей и взрослых после алло-ТГСК. Отсутствие ремиссии основного заболевания на момент трансплантации было единственным фактором риска рецидива или прогрессирования инвазивного микоза, и ухудшения результатов алло-ТГСК.
Ключевые слова
Предшествующие инвазивные микозы, аллогенная трансплантация гемопоэтических стволовых клеток, дети и взрослые, клинические исходы.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(8108) "Внедрение новых противогрибковых средств и диагностических процедур улучшило прогноз гематологических пациентов с инвазивными микозами (ИМ). Увеличилось число пациентов с ИМ, кандидатов на аллогенную трансплантацию гемопоэтических стволовых клеток (алло-ТГСК). Роль ИМ, развившихся до алло-ТГСК, по-прежнему не определена. Нет опубликованных данных о результатах алло-ТГСК у педиатрических пациентов с предшествующим ИМ. Цель исследования – оценить влияние предшествующего ИМ на результаты алло-ТГСК.
Пациенты и методы
В проспективное исследование были включены 504 реципиента алло-ТГСК в период с января 2013 года по июль 2016 года. Средний возраст составил 24 года (2 месяца – 76 лет), дети (<18 лет) – 164, взрослые – 340, мужчины – 52%. Преимущественно пациенты с диагнозом острый лейкоз группы высокого риска (74,6%). Алло-ТГСК от неродственного совместимого донора были выполнены у 58,5%, совместимого родственного донора – 22,5%, гаплоидентичного – 19%, преимущественно с использованием режима кондиционирования со сниженной интенсивностью (67%). Непосредственно перед алло-ТГСК всем пациентам с обнаруженными изменениями ткани легких, в результате компьютерной томографии органов грудной клетки, выполнялась бронхоскопия с исследованием жидкости бронхоальвеолярного лаважа: микроскопии, культуры и теста на галактоманнан. Для диагностики доказанного и вероятного ИМ и оценки ответа на терапию были использованы критерии EORTC/MSG 2008. «Активный ИМ» – ИМ, диагностированный непосредственно перед трансплантацией. Медиана наблюдения составила 20 месяцев. Основными конечными точками были общая выживаемость (ОВ), частота рецидива или прогрессирования ИМ после алло-ТГСК; вторичные точки – частота острой и хронической РТПХ, рецидива основного заболевания.
Результаты
Частота ИМ до алло-ТГСК составила 15% (n=76). Согласно критериям EORTS/MSG 2008, 90,8% пациентов имели вероятный и 9,2% доказанный ИМ. Этиология ИМ до трансплантации: инвазивный аспергиллез (ИА) – 75%, инвазивный кандидоз (ИК) – 13%, мукормикоз (М) – 4%, пневмоцистная пневмония (ПП) – 1,3% и комбинация ИА с М диагностирована у 2 пациентов, с ИК – 1, с ПП – 1. Основным органом поражения были легкие – 95%, другие локализации, преимущественно в сочетании с вовлечением легких: синусы – 9%, селезенка – 6%, печень – 6%, и мягкие ткани – 3%. Противогрибковая терапия перед алло-ТГСК применялась у 75% пациентов с медианой продолжительности – 2 месяца. Полный ответ на противогрибковую терапию был достигнут у 38,2% пациентов, частичный ответ или стабилизация – 35,5%, а у 26,3% пациентов был «активный ИМ». После алло-ТГСК все пациенты получали противогрибковую терапию или вторичную профилактику в соответствии с этиологией ИМ. Кумулятивная частота рецидива или прогрессирования ИМ после алло-ТГСК составила 14,5%. Отсутствие ремиссии основного заболевания в момент трансплантации был единственным фактором риска рецидива или прогрессирования ИМ после алло-ТГСК (11,5% против 21,1%, p=0,03). Существенных различий в кумулятивной частоте острой (p=0,28), хронической РТПХ (p=0,25) и рецидива (p=0,31) не было обнаружено в сравнении с группой пациентов без ИМ в анамнезе. 3-летняя ОВ после алло-ТГСК составила 67,5%. Общая выживаемость у реципиентов аллоТГСК без ИМ и имевших ИМ в анамнезе статистически не различалась во всех группах (60,5% против 68,7%, р=0,1), как отдельно у детей (50,0% против 57,4% , P=0,32) так и у взрослых (63,3% против 74,6%, p=0,09). Наихудший результат наблюдался у пациентов с «активным ИМ» и отсутствием ремиссии основного заболевания на момент трансплантации (3-летняя ОВ – 20%, р <0,001). Однако у пациентов с «активным ИМ» и ремиссией основного заболевания ОВ была аналогична выживаемости пациентов без ИМ в ананмнезе (80% против 68,7%, р=0,57).
Выводы
Пятнадцать процентов реципиентов алло-ТГСК имели инвазивный микоз в анамнезе. Кумулятивная частота рецидива или прогрессирования инвазивных микозов после алло-ТГСК составила 14,5%. Предшествующий инвазивный микоз не оказывал существенного влияния на результаты трансплантации и общую выживаемость детей и взрослых после алло-ТГСК. Отсутствие ремиссии основного заболевания на момент трансплантации было единственным фактором риска рецидива или прогрессирования инвазивного микоза, и ухудшения результатов алло-ТГСК.
Ключевые слова
Предшествующие инвазивные микозы, аллогенная трансплантация гемопоэтических стволовых клеток, дети и взрослые, клинические исходы.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "23051" ["VALUE"]=> array(2) { ["TEXT"]=> string(690) "<p><sup>1</sup> НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургсий государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия<br> <sup>2</sup> НИИ Медицинской микологии им. П. Н. Кашкина, Северо-западный государственный медицинский университет им. И. И. Мечникова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(648) "1 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургсий государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 НИИ Медицинской микологии им. П. Н. Кашкина, Северо-западный государственный медицинский университет им. И. И. Мечникова, Санкт-Петербург, Россия
1 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургсий государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 НИИ Медицинской микологии им. П. Н. Кашкина, Северо-западный государственный медицинский университет им. И. И. Мечникова, Санкт-Петербург, Россия
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the standard treatment option in a significant proportion of patients suffering from malignant (acute and chronic leukemias, lymphomas, primary myelofibrosis, myelodysplastic syndrome, etc.) and non-malignant blood diseases (aplastic anemia, primary immunodeficiency, inherited metabolic disorders, hemoglobinopathies, etc.) [1-4]. Despite high therapeutic efficacy, allo-HSCT is associated with the risk of disability and death caused by various post-transplant complications such as graft-versus-host disease (GVHD), severe organ toxicity, infections, and worsening of concomitant diseases causing nonrelapse mortality (NRM). Careful donor selection, flexible conditioning regimens, using of novel strategies for GVHD prevention and prophylaxis of infectious complications reduce the risk of the allo-HSCT procedure [5, 6]. Nevertheless, the problem of NRM remains relevant what determines the need to evaluate all potential pre-transplant risk factors associated with both the underlying disease and its treatment, as well as with comorbid conditions.
In 1987 M. Charlson proposed a comorbidity index, in order to stratify the risk of post-transplant complications. The Charlson Comorbidity Index (CCI) was being used for a long time, but it had several significant limitations and low sensitivity [7]. In 2005, M. Sorror and colleagues modified the CCI and proposed the first specific Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) which was amended in 2014 [8, 9]. HCT-CI differed from CCI, e.g., in grading the severity of pulmonary comorbidities by introducing specific parameters of pulmonary function test (PFT), i.e., forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco). The Fred Hutchinson Cancer Research Center study demonstrated high prognostic significance of these PFT parameters in relation to the risk of severe respiratory failure development and mortality within the first 120 days after HSCT [10]. Importantly, the described cohort consisted by 95% of patients given myeloablative conditioning (MAC). At the same time, in a number of studies using reduced intensity conditioning (RIC), the total lung capacity (TLC) and the forced vital capacity (FVC) had a more prognostic significance rather than FEV1 and DLco parameters [11].
The evolving concept of evaluating comorbidities during HSCT is to identify subclinical organ dysfunctions, which cannot be evaluated by means of HCT-CI index. The most progress in this area has been reached in evaluation and prediction of acute kidney injury and cardiotoxicity using highly sensitive biomarkers [12, 13]. However, currently there are not such biomarkers for detection of subclinical lung injury in the context of HSCT [14].
The frequency of detection and prognostic significance of abnormal pulmonary functional tests (PFT) during HSCT was significantly increased due to implication of novel diagnostic criteria. In the original retrospective study of M. Sorror et al., among 347 patients with moderate or high severity of pulmonary comorbidity, 122 patients died without signs of relapse, including 24% of deaths directly from the toxic lung injury [9].
Currently, all potential allo-HSCT recipients are undergoing PFTs. However, the pre-transplant examination in real clinical practice is limited to the screening level, often with incorrect spirometry manoeuvres, and the data are interpreted without taking into account all the potential factors that compromise pulmonary health before allo-HSCT procedure. Previous pulmonary infections, an extremely wide range of medical drugs are able to induce pulmonary toxicity, history of mediastinal radiation therapy, lung involvement due to underlying diseases, and other factors, along with chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) are of importance in the risk of post-transplantation pulmonary complications and NRM. At the same time, a novel unexplored landscape of pulmonary comorbidity is being observed in the context of expanding indications for allo-HSCT, new treatment modalities before allo-HSCT, increasing age limit for recipients, widespread usage of non-myeloablative conditioning and GVHD prophylaxis based on post-transplant cyclophosphamide.
Hence, the aim of our work was to perform a comprehensive evaluation of all potential pre-transplant factors of lung injury and integral PFT data in a large cohort of adult allo-HSCT patients suffering from malignant and non-malignant blood diseases.
Patients and methods
The present study was carried out at the Raisa Gorbacheva Memorial Research Institute for Pediatric Oncology, Hematology and Transplantation, M. Chernorutskiy Department of Hospital Therapy, and Department of Functional Diagnostics № 2 at Scientific and Clinical Research Center of the Fist St. Petersburg State I. Pavlov Medical University. The study was approved by the local ethics committee. All the patients gave written informed consent.
The study was both retrospective (data analysis until December 31, 2017) and prospective (data analysis after January 1, 2017). The analysis included patients with various malignant and non-malignant blood diseases who underwent allo-HSCT (in retrospective phase) or were scheduled for it (in prospective phase). The inclusion criteria for the study were as follows: 1. Patients’ age at the time of allo-HSCT over 18 years old; 2. Availability of sufficient anamnestic data about previous respiratory diseases, or risk factors for bronchopulmonary system; 3. Presence of pre-transplant PFT results.
The study was based on real clinical practice, so it was not limited by the characteristics of the donor (HLA-matched sibling, unrelated, haploidentical), graft source (bone marrow, peripheral blood), conditioning regimen (MAC, RIC), and regimen of GVHD prophylaxis.
Identification of pre-transplant risk factors for lung injury was based on a detailed history taking and analysis of available medical records (case histories, outpatient records, etc.). Pulmonary symptoms within one month before the start of conditioning (shortness of breath, cough, etc.), history of BA, COPD, previous pulmonary infections, administration of drugs causing potential pulmonary toxicity (bleomycin, carmustine, cytosine arabinoside, methotrexate) and immune checkpoint inhibitors (nivolumab, pembrolizumab), previous mediastinal radiation therapy, proven or suspected specific lung involvement and the status of the underlying blood disease at the moment of allo-HSCT were documented.
The data analysis included results of PFTs performed within 4 weeks before the allo-HSCT procedure. PFTs included spirometry and DLco measurement. All the PFTs were performed with MasterScreen equipment (CareFusion 234 GmbH, Erich Jaeger, Höchberg, Germany) according to the standards of the American Thoracic Society and European Respiratory Society (ATS/ERS) [15]. DLco measurement was performed with single-breath hold technique, using a gas mixture consisting of CO (0.25-0.30%), helium (8.9-10.0%) and synthetic air. DLco value was adjusted for hemoglobin concentration at the time of PFTs performance [16, 17]. The analyzed PFT parameters included spirometric vital capacity (VC), FVC, FEV1, FEV1/VC ratio (Tiffeneau index), DLco (adjusted for hemoglobin concentration), alveolar volume (Va), carbon monoxide transfer coefficient (Krogh factor, Kco). The absolute values of the PFT parameters and their percentage to predicted values were evaluated using formulas for predicted PFT values by R. Clement et al. [18].
Severity of pulmonary comorbidity was evaluated according to criteria of HCT-CI [8, 9]. Mild pulmonary comorbidity was defined as DLco and/or FEV1 values of 81%-90%, or dyspnea at moderate physical activity. Moderate pulmonary comorbidity was defined as DLco and/or FEV1 values of 66%-80%, or dyspnea at minimal activity. Severe pulmonary comorbidity was defined as DLco and/or FEV1 values of ≤65% or dyspnea at rest, or requirement for oxygen therapy.
Statistical evaluation of the cohort and outcomes of allo-HSCT was performed as of May 1, 2019. Descriptive characteristics included the number of observations and proportions for discrete factors, medianes, range of values, interquartile ranges and 95% confidence intervals (CI) for continuous values. Differences between the analyzed groups were evaluated using Kruskal-Wallis test (quantitative characteristics), Fisher's exact test and Pearson chi-square (categorical characteristics).
The cumulative incidence of mechanical ventilation (MV) and NRM rates were calculated from the date of allo-HSCT to the date of the beginning of the MV and death unrelated to the relapse of the underlying disease, respectively. Death prior to the onset of mechanical ventilation and relapses were considered competing risks. Prognostic value of the severity of pulmonary comorbidity and other potential risk factors for NRM (age, diagnosis, disease status at the time of HSCT, type of donor, protocol of GVHD prophylaxis, year of HSCT, severe acute GVHD) was performed in the Fine-Gray regression model for competing events. Overall survival (OS) was estimated using the Kaplan-Meier method from the date of allo-HSCT to the date of death, or the last contact with the patient. Comparison of survival was performed using the log-rank test.
The two-sided alternative testing hypothesis was applied, being statistically significant at the p-value of <0.05. Statistical analysis was performed using EZR statistical software, version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Clinical characteristics
As of May 1, 2019, 355 patients were included in the study, among them 206 (58%) and 149 (42%) in the retrospective and prospective phases, respectively. The basic demographic and clinical characteristics of the patient cohort are presented in Table 1.
In terms of age, gender, diagnosis and clinical indications for allo-HSCT, donor characteristics, conditioning regimens, the analyzed cohort appears to be representative and generally reflects the current transplant activity in adult patients.
Table 1. The basic demographic and clinical characteristics of patient cohort

Baseline factors of pulmonary comorbidity
At the first stage of the study, we analyzed the baseline potential risk factors and causes of pulmonary comorbidity in the entire patient cohort, as listed in Table 2.
Table 2. Risk factors for pulmonary comorbidity

Tobacco smoking, including high pack-year rates (> 20) for every fourth smoker was most frequent (32%) among the basic risk factors unrelated to the underlying disease and its treatment. A documented diagnosis of COPD and BA was present in, respectively, 15 (4.2%) and 4 (1.1%) of HSCT recipients. It should be noted that the majority of COPD patients (13/15) had a mild-severity disease, and intermittent BA was diagnosed in all 4 cases. The leading group of lung diseases reported before allo-HSCT was presented by pulmonary infections (44.9%), dominated by clinically proven pneumonia (35.8%). In general, microbiological verification of the pathogens in available medical documentation was low, and to a greater extent concerned only invasive mycoses with lung involvement (16%). Ten patients (2.8%) had the history of pulmonary tuberculosis, or radiological signs of previous tuberculosis which required secondary prophylaxis with tuberculostatic drugs.
Frequently used medical drugs with known lung toxicity, e.g., cytarabine (65%), as well as bleomycin (8.2%) and carmustine (5.2%) applied in anticancer chemotherapy before allo-HSCT were also identified as potential risk factors. In addition, 30 (8.5%) and 22 (6.2%) patients had the history of high-dose chemotherapy followed by autologous HSCT and mediastinal therapeutic irradiation, respectively. Use of immune checkpoint inhibitors was considered another particular potential risk factor of pre-HSCT pulmonary injury (5.4% of entire cohort).
In general, statistical evaluation of the potential factors predisposing for pulmonary compromise allowed us to identify two of the most characteristic disease-specific profiles associated with clinical course of the underlying disease and its treatment. The greatest number of risk factors for pulmonary comorbidity was revealed among the patients with lymphomas who received treatment with bleomycin, carmustine, cytarabine, immune checkpoint inhibitors, radiation therapy and autologous HSCT. The second group was represented by patients with acute leukemia and a part of MDS patients who received chemotherapy with cytarabine and showed high incidence of neutropenic pulmonary infections before allo-HSCT. Patients with AA did not exhibit specific drug pulmonary toxicity in anamnesis. However, this group of patients had an increased risk of iron overload, having been associated with multiple blood transfusions.
The proportion of smokers was higher among the patients with lymphomas (41%) and myeloproliferative diseases, and MDS (39%) compared with acute leukemia (30%) and, especially, AA group (19%). However, 48% of smokers with MPD and MDS had a smoking index of more than 20 pack-years, which was significantly higher than for with acute leukemia (22%) and lymphoma patients (21%) (p=0.0461). The frequency of concomitant COPD was significantly higher among patients with MPD and MDS, i.e., 7/54 (13%), compared with 0/27 (0%), 5/215 (2%) and 3/59 (5%) with AA, acute leukemia and lymphomas respectively (p=0.0038).
These patterns are partly explained by differences in the age and the duration of the disease at the time of allo-HSCT. The median age was 28, 32, 37 and 45 years in patients with SAA, acute leukemia, lymphomas and MPD and MDS respectively (p <0.0001). Accordingly, the median time between the diagnosis and allo-HSCT was 1.9, 1.1, 3.6, and 1.4 years (p <0.0001).
Table 3. Frequency of individual pulmonary CT symptoms before allo-HSCT (n=270)

Chest computed tomography (CT) findings at the time of allo-HSCT were available in 270 (76%) patients. Pathological changes in lung structures were documented in 190 (70.6%) of the examined patients (Table 3). The signs of local pulmonary fibrosis and focal changes were the most frequent CT symptoms detected in more than 50% and 30% of patients, respectively.
Pulmonary function tests (PFT)
At the next step of our study, we analyzed data from a pre-HSCT PFT with a focus on the key FEV1 and DLco parameters which are included in HCT-CI comorbidity criteria. Testing of FEV1 and other standard spirometry parameters covered the entire cohort (n=355), while the data on the pulmonary diffusing capacity, including DLco were obtained from 76 patients, predominantly in the prospective phase of the study. The main parameters of spirometry and pulmonary diffusing capacity are presented in Table 4.
FEV1 varied within 49-145% of predicted, the median was 100.6%, the interquartile range was 90-109.6%. According to HCT-CI criteria, 90 (25%) patients had low FEV1 value, including 14%, 9% and 2% of mild, moderate and severe grade respectively.
When verifying alterations of the pulmonary diffusing capacity, two methods were used to adjust the obtained DLco values for the hemoglobin levels. The median hemoglobin level at the time of DLco testing was 10.3 g/dL (5.8-16.4). There was decreased hemoglobin level in 80% of women and 57% of men. Frequency of diffusion disorders by the DLco values seems to be definitely overestimated (96%) when using the Cotes hemoglobin correction method, which is routinely recommended by ATS/ERS experts and used by default in pulmonary practice. The Dinakara method aiming to adjust DLco for hemoglobin levels provided a more accurate assessment and showed DLco disorders in 69% of the examined patients, including 29%, 28% and 12% frequency rates for mild-, moderate- and severe-grade alterations respectively.
Table 4. Pulmonary function tests characteristics before allo-HSCT

When analyzing PFT data in patients with different diagnoses, more frequent bronchial obstruction according to the FEV1/VC parameter was found in the patients with MPD and MDS, whereas disorders of pulmonary diffusing capacity according to the adjusted DLco were more pronounced in patients with lymphomas (Table 5). Other tested parameters did not show significant dependence on the underlying disease.
Table 5. Pulmonary function tests before allo-HSCT according to the diagnosis

In general, taking into account the maximum contribution of FEV1 or DLco data 68 (19%), 49 (14%) and 14 (4%) patients corresponded to the criteria for mild, moderate and severe pulmonary comorbidity, respectively (Table 6).
Table 6. Severity of pulmonary function abnormalities before allo-HSCT


Figure 1. NRM with stratification of patients according to the severity of pulmonary comorbidity

Figure 2. Cumulative incidence of mechanical ventilation with stratification of patients according to the severity of pulmonary comorbidity

Figure 3. Overall survival after allo-HSCT with stratification of patients according to the severity of pulmonary comorbidity
Prognostic value of pulmonary comorbidity for the outcome of allo-HSCT
The prognostic value of pulmonary comorbidity parameters was tested by its analyzing against cumulative incidence of NRM and overall survival (OS) after allo-HSCT. In the whole cohort, NRM and cumulative incidence of relapse in 2 years were 21.0% (95% CI, 16.4-25.9) and 10.5% (95% CI, 7.3-14.3).
Stratification of patients according to the severity of pulmonary comorbidity revealed significant differences in NRM (Fig. 1). The cumulative incidence of death without signs of relapse of the underlying disease within 12 months after allo-HSCT was 13.8% (CI 95%, 9.5-18.9), 14.1% (CI 95%, 6.4-24.7), 26.7% (CI 95%, 14.5-40.4) and 53.2% (CI 95%, 22.1-76.9) with pulmonary comorbidity 0, 1, 2, 3 degrees respectively (p=0.0004).
The value of pulmonary comorbidity was further evaluated by a surrogate criterion of severe respiratory failure with need for mechanical ventilation (MV). Indications for MV occurred in 34 (9.6%) and 54 (15.2%) patients during the first 100 days and 1 year after allo-HSCT, respectively. In two other cases, MV was performed later. In order to reduce the significance of the primary disease relapse, further analysis was carried out for patients who developed severe respiratory failure during the first 100 days after allo-HSCT.
Stratification of patients according to the pulmonary comorbidity revealed a significant increased risk of switching to MV in high-risk patients (Fig. 2). Cumulative incidence of the MV within 100 days from allo-HSCT was 7.2% (CI 95%, 3.8-10.6), 10.9% (CI 95%, 2.9-18.2), 16.7% (CI 95%, 5.4-26.6) and 22.1% (CI 95%, 0-41.3) in patients with pulmonary comorbidity of 0, 1, 2 and 3 degree, respectively (p=0.0176).
Prognostic significance of the degree of pulmonary comorbidity for the risk of NRM was confirmed in a multivariate analysis, using the Fine-Gray regression model for competing events (Table 7). Other factors associated with increased risk of NRM were: primary diagnosis (maximum risk for MPD and MDS, minimum for SAA), lack of remission at the time of allo-HSCT, MAC regimen, type of donor (maximum risk for a haploidentical donor), year of HSCT and the presence of severe acute GVHD (aGVHD).
In contrast to the severity of PFT disorders, none of the potential pulmonary comorbidity factors discussed above (smoking, presence of lung diseases before HSCT, pulmonary toxicity, radiation therapy), as well as the age of patients at the time of allo-HSCT, did not have independent prognostic value.
The risk of relapse after allo-HSCT as expected did not depend from the degree of pulmonary comorbidity. Despite this, due to significant differences in NRM, pulmonary comorbidity was associated with a decrease in overall survival: 71.9% (95% CI, 63.8-78.5), 61.9% (95% CI, 42.5-76.4), 54.3% (95% CI, 36.2-69.1) and 39.0 (95% CI, 14.3-63.3) at 5 years after allo-HSCT with 0, 1, 2, and 3 degrees respectively (p=0.0014) (Fig. 3).
Table 7. Multivariate analysis of characteristics affecting non-relapse mortality

Discussion
The HCT-CI is an important diagnostic tool in screening candidates for allo-HSCT [8, 9, 17]. Despite some inaccuracies with HCT-CI as prognostic indicators, a score of 3 and above always remains a sign of a high-degree risk for relapse-unrelated deaths. Currently, the assessment of the bronchopulmonary condition is one of essential components in pre-transplant examination of the patients, including PFTs with FEV1 and DLco, assessment, as well as chest CT evaluation [19].
The study by M. Sorror and colleagues has revealed that FEV1 and/or DLco reflect a correlation between causes of death and pulmonary comorbid pathology when assessing NRM rates [8]. Of the 347 patients who had moderate or severe degrees of pulmonary comorbidity, 122 died from causes unrelated to the relapse of primary disease. The causes of NRM were severe pulmonary toxicity (24%), pulmonary complications of cGVHD (11%), lower respiratory tract infections (45%) that were associated (18%), or non-associated (27%) with cGVHD, and other causes (20%) [8].
Conventional spirometry is the most common screening method in examining the function of respiratory system. Spirometry is aimed to identify and determine the type of pulmonary function disorders, primarily obstructive, with the Tiffeneau index and FEV1 [20, 21]. Spirometry makes it possible to diagnose broncho-obstructive diseases (BA, COPD, etc.), like as to predict clinical outcomes of the scheduled allo-HSCT [9, 19].
The DLco test is another functional method for assessing the state of lower respiratory tract. It is used to evaluate gas exchange via the alveolar-capillary membrane [20, 21]. The DLco test detects probable interstitial changes of pulmonary tissue in patients with a history of using pulmonary toxic drugs (cytarabine, bleomycin, carmustine, nivolumab, etc.), radiation therapy, as well as changes associated with the course of the underlying disease (specific pulmonary tissue involvement, iron overload, etc.) [20-27].
Despite its obvious diagnostic advantage in identifying “subclinical” pulmonary injuries associated with the course or therapy of oncohematological disease, the DLco study is technically difficult for real clinical practice, thus being rarely performed in routine functional diagnostics.
The main objective of this study was to perform comprehensive analysis of lung health before allo-HSCT, and its connection with development of infectious and non-infectious bronchopulmonary complications in the post-transplant period, as well as NRM rates. Our analysis included 355 adult patients with various neoplastic and benign blood diseases who received allo-HSCT from a related, unrelated, and haploidentical donors. In contrast to previously published data, the analyzed cohort was balanced in terms of conditioning regimen (MAC 40%, RIC 60%) and graft source (BM 38%, G-PBSC 62%) [8-11]. Median age of the patients at the time of allo-HSCT (33 years old) was lower compared with other observations, but the distribution of primary diagnoses did not significantly differ [8, 10, 11]. For the first time, adult patients with SAA (8%) were presented in the cohort.
The study assessed anamnestic data on pre-existing chronic respiratory diseases (COPD, BA) and previous bronchopulmonary infections (pneumonia, invasive mycosis, TBC). In addition, the presence of risk factors for the development of bronchopulmonary diseases (smoking, chemotherapy with pulmonary toxic drugs, mediastinal radiation therapy) was taken into account. In the observed cohort, COPD and BA were documented in 4.2% and 1.1% of patients, respectively, which is significantly lower than the data of the largest international and Russian population-based studies concerning general prevalence of COPD and BA (11.7% and 6.9%) [28]. According to literature data, the prevalence of COPD and BA among HSCT recipients was 2% and 12.2% [8, 29]. This fact can be explained by the negative selection of patients with severe forms of disease at earlier stages of treatment, even before their admission to the HSCT center.
A third of patients had a history of smoking, but a high smoking index was only 8% of patients from the entire cohort, which is comparable with another study, where the incidence of high smoking experience was 14% [30]. Pulmonary infections before allo-HSCT were in 44.9% of patients, among which pneumonia (35.8%), invasive mycosis (16%) and TBC (2.8%) prevailed. These data are similar to the results previously published by our group [31]. History of potential pulmonary toxic chemotherapy was documented in 72% of patients. However, no cases of drug-induced interstitial lung disease (DIILD) were detected in the analyzed cohort. According to available literature, the frequency of cytarabine-related DIILD varies from 15 to 44%, whereas for bleomycin, this condition is found in 6.8-21% of the patients [32-36]. The novel form of DIILD caused by nivolumab may be as frequent as in 11.7% of cases [37].
Pulmonary changes according to chest CT before allo-HSCT were detected in 71% of patients, including signs of local pulmonary fibrosis (58%) and focal changes (38%). An earlier study detected CT changes in 48% of patients with AML, ALL, and MDS before allo-HSCT [38]. Unlike our data, the foci in pulmonary tissue (46%) and ground-glass opacities (17%) were the most frequent CT symptoms. CT signs of terminal bronchiolitis, cavities and pleural effusion have also been detected relatively rarely.
Analysis of PFT parameters was carried out in the entire cohort of patients, as well as in groups of patients with different hematological disorders. Based on the HCT-CI criteria, we analyzed patients with mild, moderate, and severe degrees of pulmonary comorbidity [8]. The median FEV1 (106%) was higher than that shown in other multicenter studies, while the frequency of FEV1 decline was mild (14%), moderate (9%) and severe (2%), which did not significantly differ from earlier literature data [10-11].
In the present study we compared two methods of DLco adjustment for hemoglobin level: the method proposed by J.E. Cotes et al., recommended by ATS/ERS which is more commonly used in pulmonary practice, as well as the Dinakara method used by the Fred Hutchinson Cancer Research Center [15-18, 39-42]. According to our data, the Dinakara method seems to more precisely correct the impact of anemia to a decrease in DLco, which is comparable with similar results from another clinical study [42]. As a result, there was a decrease in DLco of mild (29%), moderate (28%) and severe (12%) degrees, which is comparable with the reported results of other observations [10-11].
Analysis of PFT parameters in patients with various hematological diseases revealed a decrease in the Tiffeneau index in patients with MPD and MDS, as well as a reduced DLco in patients with lymphomas. This relationship is not described in the literature, which is probably due to the previously low transplant activity in these groups of patients. It can be assumed that these disease-specific relationships are caused by the age of the patients, the history of pulmonary toxicity and radiation therapy, the length of smoking and proven COPD.
The key result of the study was a strong confirmation of the high prognostic significance of pulmonary comorbidity for allo-HSCT outcomes in the real-world practice and in context of changing transplant landscape [8, 10]. The patients with moderate and severe pulmonary comorbidity showed a 2- 3 fold increase in the cumulative incidence of MV requirements in the early post-transplant period. At the same time, the risk of NRM increased 2-4 times if compared to the patients without documented pulmonary comorbidity. Despite lacking differences in the frequency of relapses of the underlying disease, an association was found between moderate and, especially, severe degrees of pulmonary comorbidity and a decrease in overall survival.
Our study had a number of limitations, in particular, incomplete coverage of the cohort with DLco testing data in retrospective phase, which could cause underestimation of pulmonary comorbidity. However, taking into account the above-described features of a cohort based on the representation of different diagnoses, donor types, transplant sources, conditioning regimens and GVHD prophylaxis, the independent prognostic value of pulmonary comorbidity, as confirmed by multivariate analysis, is of particular importance.
Conclusion
Adult recipients of allogeneic HSCs have a wide range of potential causes and a high incidence of pulmonary comorbidity: non-infectious (5%) and infectious (45%) lung diseases, history of potential pulmonary toxicity (72%), lung changes according to CT (70%), disorders of respiratory function according to FEV1 (25%) and aDLco (69%). Pulmonary comorbidity and the frequency of violations of respiratory function have some disease-specific features.
In real practice, the use of a screening level of the PFT (spirometry) underestimates or incorrectly assesses the frequency of respiratory disorders in patients before allo-HSCT. The traditional DLco correction for hemoglobin level according to the Cotes method does not accurately reflect the contribution of anemia to impaired pulmonary diffusion capacity in adult patients with blood diseases and leads to an overestimated frequency of detecting severe violations of respiratory function before allo-HSCT. The Dinakara method provides more accurate DLco correction for hemoglobin levels.
In the modern landscape of allo-HSCT with a changing spectrum of indications, age of patients, conditioning regimens, GVHD prophylaxis, the degree of pulmonary comorbidity according to HCT-CI still retains a high predictive value in terms of risk of the MV and NRM.
Conflict of interest
The authors report no conflicts of interest.
References
- Afanasyev BV, Zubarovskaya LS, Moiseev IS. Allogeneic hematopoietic stem cell transplantation in children: now, problems and prospects. Russian J Pediatric Hematol Oncol. 2015;2(2):28-42. (In Russian).
- Savchenko VG, Liubimova LS, Parovichnikova EN, Mendeleeva LP, Mamotiuk KS, Demidova IA, Gribanova EO, Gal'tseva IV, Pokrovskaia OS, Kuz'mina LA, Zhelnova EI, Kliasova GA, Glasko EN, Kaplanskaia IB, Poreshina LP, et al. Transplantations of allogenic and autologous hemopoietic stem cells in acute leukemia (results of 20-year experience). Terapevticheskiy arkhiv. 2007;79 (7):30-35. (In Russian).
- Rumyantsev AG, Maschan AA Hematopoietic stem cell transplantation in children. M.: Medical Information Agency, 2003. 909 pp. (In Russian.)
- Duarte RF, Labopin M, Bader P, Basak GW, Bonini C, Chabannon C, Corbacioglu S, Dreger P, Dufour C, Gennery AR, Kuball J, Lankester AC, Lanza F, Montoto S, Nagler A, de Latour RP, Snowden JA, Styczynski J, Yakoub-Agha I, Kröger N, Mohty M for the European Society for Blood and Marrow Transplantation (EBMT). Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant. 2019:1-28. Published: 05 April 2019. doi.org/10.1038/s41409-019-0516-2.
- Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, Martin PJ, Sandmaier BM, Marr KA, Appelbaum FR, Storb R, McDonald GB. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010;363(22):2091-2101.
- Horan JT, Logan BR, Agovi-Johnson M-A, Lazarus HM, Bacigalupo AA, Ballen KK, Bredeson CN, Carabasi MH, Gupta V, Hale GA, Khoury HJ, Juckett MB, Litzow MR, Martino R, McCarthy PL, Smith FO, Rizzo JD, Pasquini MC. Reducing the risk for transplantation-related mortality after allogeneic hematopoietic cell transplantation: how much progress has been made? J Clin Oncol. 2011;29(7):806-813.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383.
- Sorror ML, Maris MB, Storb RF, Sandmaier MB, Maloney DG, Storrer B. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912-2919.
- Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB, Bhatia S, Ostronoff F, Deeg MH, Syrjala KL, Estey E, Maloney DG, Appelbaum FR, Martin PJ, Storer BE. Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol. 2014;32(29):3249-3256.
- Parimon T, Madtes DK, Au DH, Clark JG, Chien JW. Pretransplant lung function, respiratory failure, and mortality after stem cell transplantation. Am J Respir Crit Care Med. 2005;172(3):384-390.
- Piñana JL, Martino L, Barba P, Bellido-Cassado J, Valcarcel D, Sureda A, Briones J, Brunet S, Rodriguez-Arias JM, Casan P, Sierra J. Pulmonary function testing prior to reduced intensity conditioning allogeneic stem cell transplantation in an unselected patient cohort predicts posttransplantation pulmonary complications and outcome. Am J Hematol. 2012;87(1):9-14.
- Dobronravov VA, Smirnov KA, Afanasiev BV, Galkina OV, Smirnov AV. Subclinical tubular epithelium damage and acute kidney injury following allogeneic hematopoietic stem cell transplantation. Cell Ther Transplant. 2016; 5(4):8-14.
- Roziakova L, Mistrik M, Batorova A, Kruzliak P, Bojtarova E, Dubrava J, Gergel J, Mladosievicova B. Can we predict clinical cardiotoxicity with cardiac biomarkers in patients after haematopoietic stem cell transplantation? Cardiovasc Toxicol. 2015;15(3):210-216.
- Wu AC, Kiley JP, Noel PJ, Amur S, Burghard EG, Clancy JP, Galanter J, Inada M, Jones TK, Kropski JA, Loyd JE, Nogee LM, Raby BA, Rogers AJ, Schwartz DA, Sin DD, Spira A, Weiss ST, Young LR, Himes BE. Current status and future opportunities in lung precision medicine research with a focus on biomarkers. An American Thoracic Society/National Heart, Lung, and Blood Institute Research Statement. Am J Respir Crit Care Med. 2018;198(12):116-136.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CPM, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre M, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J. Interpretive strategies for lung function tests. Eur Respir J. 2005;26(5):948–968.
- Cotes J. E. Measurement of the transfer factor (diffusing capacity) for the lung and its subdivisions. Lung function assessment application in medicine. 4th ed. Oxford, UK: Blackwell Scientific Publications. 1979:230-250.
- Dinakara P, Blumenthal WS, Johnston RF, Kauffman LA, Solnick PB. The effect of anemia on pulmonary diffusing capacity with derivation of a correction equation. Am Rev Respir Dis. 1970:102(6):965-969.
- Clement RF. Fundamental and methodological foundations for the development of a unified system of proper quantities. Current problems of clinical respiratory physiology. 1987:5-19. (In Russian).
- Carreras E, Dufor C, Mohty M, Kröger N. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies. Springer. 2019:77-86.
- Chuchalin AG. Pulmonology. National guidelines. Moscow: GEOTAR-Media. 2012: 117-135. (In Russian).
- Savushkina OI, Chernyak AV. Pulmonary functional tests: from theory to practice. A guide for doctors. Moscow: Strom. 2017:11-38; 63-82. (In Russian).
- Skeoch S, Weatherley N, Swift AJ, Oldroyd A, Johns C, Hayton C, Giollo A, Wild JM, Waterton JC, Buch M, Linton K, Bruce IN, Leonard C, Bianchi S, Chaudhuri N. Drug-induced interstitial lung disease: a systematic review. J Clin Med. 2018;7(10):1-30.
- DeMonaco NA, McCarty Jr KS, Joyce J, Jacobs SA. Focal radiation fibrosis after radioimmunotherapy for follicular non-Hodgkin lymphoma. Clin Lymphoma Myeloma. 2007;7(5):369-372.
- Guner SI, Yanmaz MT, Selvi A, Usul C. Chemotherapy and radiation induced pulmonary dysfunction in Hodgkin lymphoma patients. Indian J Hematol Blood Transfus. 2016;32(4):431-436.
- Berkman N, Breuer R, Kramer MR, Polliack A. Pulmonary involvement in lymphoma. Leuk Lymphoma. 1996;20(3-4):229-237.
- Mian M, Wasle I, Gritsch S, Willenbacher W, Fiegl M. B cell lymphoma with lung involvement: what is it about? Acta Haematol. 2015;133(2):221-225.
- Kamble R, Rosenzweig T. Diffuse pulmonary parenchymal involvement in multiple myeloma: antemortem diagnosis. Int J Hematol. 2006;83(3):259-261.
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2017 update. 2017:13-24. Available at: http://www.ginasthma.org. Accessed June 23, 2017.
- Chien SH, Liu C-J, Hong Y-C, Teng C-J, Hu Y-W, Shen C-C, Ku F-C, Chen S-C, Yeh C-M, Chiou T-J, Gau J-P, Tzeng C-H. Use of azathioprine for graft-vs-host disease is the major risk for development of secondary malignancies after haematopoietic stem cell transplantation: a nationwide population-based study. Br J Cancer. 2015;112(1):177-184.
- Mehdi A, Rybicki L, Mossad S, Yurch M, Sekeres M, Gerds AT, Jagadeesh D, Hamilton B, Liu H, Dean R, Pohlman B, Sobecks R, Andresen S, Kalaycio M, Bolwell BJ, Majhail MS, Copelan E, Hill BT. Impact of cigarette smoking on survival after myeloablative allogeneic hematopoietic stem cell transplantation and contribution of invasive fungal infection. Bone Marrow Transplant. 2017;52(12);1665-1667.
- Popova MO, Ekushov KA, Ayzsilnieks OV, Volkova AG, Pinegina ON, Ignatieva SM, Slesarchuk OA, Vladovskaya MD, Bondarenko SN, Zubarovskaya LS, Klimko NN, Afanasyev BV. Invasive fungal infections in recipients of allogeneic hematopoietic stem cell teens and young adults. Russian J Pediatric Hematol Oncol. 2016; (1):44-51. (In Russian).
- Ilkovich MM. Interstitial and orphan lung diseases. Moscow: GEOTAR-Media. 2016:289-316 (In Russian).
- Blum RH, Carter SK, Agre K. A clinical review of bleomycin – a new antineoplastic agent. Cancer. 1973;31(4):903-914.
- Hubbard SP, Chabner BA, Canellos GP, Young RC, DeVita Jr. VT. High dose intravenous bleomycin in the treatment of advanced lymphomas. Eur J Cancer. 1975;11(9):623-626.
- Ngeow J, Tan IB, Kanesvaran R, Tan HC, Tao M, Quek R, Lim ST. Prognostic impact of bleomycin-induced pneumonitis on the outcome of Hodgkin’s lymphoma. Ann Hematol. 2011;90(1):67-72.
- Stamatoullas A, Brice P, Bouabdallah R, Mareschal S, Camus V, Rahal I, Franchi P, Lanic H, Tilly H. Outcome of patients older than 60 years with classical Hodgkin lymphoma treated with front line ABVD chemotherapy: frequent pulmonary events suggest limiting the use of bleomycin in the elderly. Br J Haematol. 2015;170(2):179-184.
- Nishino M, Ramaiya NH, Awad MM, Sholl LM, Maattala JA, Taibi M, Hatabu H, Ott PA, Armand PF, Hodi FS. PD-1 inhibitor-related pneumonitis in advanced cancer patients: radiographic patterns and clinical course. Clin Cancer Res. 2016;22(24):6051-6060.
- El Boghdadly Z, Oran B, Rondon JG, Champlin R, Kontoiyannis DP. Pretransplant chest computed tomography screening in asymptomatic patients with leukemia and myelodysplastic syndrome. Bone Marrow Transplant. 2017;52(3):476-479.
- Sorror ML. How I assess comorbidities before hematopoietic cell transplantation. Blood. 2013;121(15):2854-2863.
- Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, Maziarz RT, Antin JH, Soiffer RJ, Weisdorf DJ, Rizzo D, Horowitz MM, Saber W. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123(23):3664-3671.
- Shouval R, Labopin M, Bondi O, Mishan Shamay H, Shimoni A, Ciceri F, Esteve Reiner J, Giebel S, Gorin NC, Schmid C, Polge E, Aljurf M, Kroger N, Craddock CF, Bacigalupo A, Cornelissen JJ, Baron F, Under R, Nagler A, Mohty M. Prediction of allogeneic hematopoietic stem-cell transplantation mortality 100 days after transplantation using a machine learning algorithm: a European Group for Blood and Marrow Transplantation Acute Leukemia Working Party Retrospective Data Mining Study. J Clin Oncol. 2015;33(28):3144-3151.
- Coffey DG, Pollyea DA, Myint H, Smith C, Gutman JA. Adjusting DLCO for Hb and its effects on the Hematopoietic Cell Transplantation-specific Comorbidity Index. Bone Marrow Transplant. 2013;48(9):1253-1256.
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the standard treatment option in a significant proportion of patients suffering from malignant (acute and chronic leukemias, lymphomas, primary myelofibrosis, myelodysplastic syndrome, etc.) and non-malignant blood diseases (aplastic anemia, primary immunodeficiency, inherited metabolic disorders, hemoglobinopathies, etc.) [1-4]. Despite high therapeutic efficacy, allo-HSCT is associated with the risk of disability and death caused by various post-transplant complications such as graft-versus-host disease (GVHD), severe organ toxicity, infections, and worsening of concomitant diseases causing nonrelapse mortality (NRM). Careful donor selection, flexible conditioning regimens, using of novel strategies for GVHD prevention and prophylaxis of infectious complications reduce the risk of the allo-HSCT procedure [5, 6]. Nevertheless, the problem of NRM remains relevant what determines the need to evaluate all potential pre-transplant risk factors associated with both the underlying disease and its treatment, as well as with comorbid conditions.
In 1987 M. Charlson proposed a comorbidity index, in order to stratify the risk of post-transplant complications. The Charlson Comorbidity Index (CCI) was being used for a long time, but it had several significant limitations and low sensitivity [7]. In 2005, M. Sorror and colleagues modified the CCI and proposed the first specific Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) which was amended in 2014 [8, 9]. HCT-CI differed from CCI, e.g., in grading the severity of pulmonary comorbidities by introducing specific parameters of pulmonary function test (PFT), i.e., forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco). The Fred Hutchinson Cancer Research Center study demonstrated high prognostic significance of these PFT parameters in relation to the risk of severe respiratory failure development and mortality within the first 120 days after HSCT [10]. Importantly, the described cohort consisted by 95% of patients given myeloablative conditioning (MAC). At the same time, in a number of studies using reduced intensity conditioning (RIC), the total lung capacity (TLC) and the forced vital capacity (FVC) had a more prognostic significance rather than FEV1 and DLco parameters [11].
The evolving concept of evaluating comorbidities during HSCT is to identify subclinical organ dysfunctions, which cannot be evaluated by means of HCT-CI index. The most progress in this area has been reached in evaluation and prediction of acute kidney injury and cardiotoxicity using highly sensitive biomarkers [12, 13]. However, currently there are not such biomarkers for detection of subclinical lung injury in the context of HSCT [14].
The frequency of detection and prognostic significance of abnormal pulmonary functional tests (PFT) during HSCT was significantly increased due to implication of novel diagnostic criteria. In the original retrospective study of M. Sorror et al., among 347 patients with moderate or high severity of pulmonary comorbidity, 122 patients died without signs of relapse, including 24% of deaths directly from the toxic lung injury [9].
Currently, all potential allo-HSCT recipients are undergoing PFTs. However, the pre-transplant examination in real clinical practice is limited to the screening level, often with incorrect spirometry manoeuvres, and the data are interpreted without taking into account all the potential factors that compromise pulmonary health before allo-HSCT procedure. Previous pulmonary infections, an extremely wide range of medical drugs are able to induce pulmonary toxicity, history of mediastinal radiation therapy, lung involvement due to underlying diseases, and other factors, along with chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) are of importance in the risk of post-transplantation pulmonary complications and NRM. At the same time, a novel unexplored landscape of pulmonary comorbidity is being observed in the context of expanding indications for allo-HSCT, new treatment modalities before allo-HSCT, increasing age limit for recipients, widespread usage of non-myeloablative conditioning and GVHD prophylaxis based on post-transplant cyclophosphamide.
Hence, the aim of our work was to perform a comprehensive evaluation of all potential pre-transplant factors of lung injury and integral PFT data in a large cohort of adult allo-HSCT patients suffering from malignant and non-malignant blood diseases.
Patients and methods
The present study was carried out at the Raisa Gorbacheva Memorial Research Institute for Pediatric Oncology, Hematology and Transplantation, M. Chernorutskiy Department of Hospital Therapy, and Department of Functional Diagnostics № 2 at Scientific and Clinical Research Center of the Fist St. Petersburg State I. Pavlov Medical University. The study was approved by the local ethics committee. All the patients gave written informed consent.
The study was both retrospective (data analysis until December 31, 2017) and prospective (data analysis after January 1, 2017). The analysis included patients with various malignant and non-malignant blood diseases who underwent allo-HSCT (in retrospective phase) or were scheduled for it (in prospective phase). The inclusion criteria for the study were as follows: 1. Patients’ age at the time of allo-HSCT over 18 years old; 2. Availability of sufficient anamnestic data about previous respiratory diseases, or risk factors for bronchopulmonary system; 3. Presence of pre-transplant PFT results.
The study was based on real clinical practice, so it was not limited by the characteristics of the donor (HLA-matched sibling, unrelated, haploidentical), graft source (bone marrow, peripheral blood), conditioning regimen (MAC, RIC), and regimen of GVHD prophylaxis.
Identification of pre-transplant risk factors for lung injury was based on a detailed history taking and analysis of available medical records (case histories, outpatient records, etc.). Pulmonary symptoms within one month before the start of conditioning (shortness of breath, cough, etc.), history of BA, COPD, previous pulmonary infections, administration of drugs causing potential pulmonary toxicity (bleomycin, carmustine, cytosine arabinoside, methotrexate) and immune checkpoint inhibitors (nivolumab, pembrolizumab), previous mediastinal radiation therapy, proven or suspected specific lung involvement and the status of the underlying blood disease at the moment of allo-HSCT were documented.
The data analysis included results of PFTs performed within 4 weeks before the allo-HSCT procedure. PFTs included spirometry and DLco measurement. All the PFTs were performed with MasterScreen equipment (CareFusion 234 GmbH, Erich Jaeger, Höchberg, Germany) according to the standards of the American Thoracic Society and European Respiratory Society (ATS/ERS) [15]. DLco measurement was performed with single-breath hold technique, using a gas mixture consisting of CO (0.25-0.30%), helium (8.9-10.0%) and synthetic air. DLco value was adjusted for hemoglobin concentration at the time of PFTs performance [16, 17]. The analyzed PFT parameters included spirometric vital capacity (VC), FVC, FEV1, FEV1/VC ratio (Tiffeneau index), DLco (adjusted for hemoglobin concentration), alveolar volume (Va), carbon monoxide transfer coefficient (Krogh factor, Kco). The absolute values of the PFT parameters and their percentage to predicted values were evaluated using formulas for predicted PFT values by R. Clement et al. [18].
Severity of pulmonary comorbidity was evaluated according to criteria of HCT-CI [8, 9]. Mild pulmonary comorbidity was defined as DLco and/or FEV1 values of 81%-90%, or dyspnea at moderate physical activity. Moderate pulmonary comorbidity was defined as DLco and/or FEV1 values of 66%-80%, or dyspnea at minimal activity. Severe pulmonary comorbidity was defined as DLco and/or FEV1 values of ≤65% or dyspnea at rest, or requirement for oxygen therapy.
Statistical evaluation of the cohort and outcomes of allo-HSCT was performed as of May 1, 2019. Descriptive characteristics included the number of observations and proportions for discrete factors, medianes, range of values, interquartile ranges and 95% confidence intervals (CI) for continuous values. Differences between the analyzed groups were evaluated using Kruskal-Wallis test (quantitative characteristics), Fisher's exact test and Pearson chi-square (categorical characteristics).
The cumulative incidence of mechanical ventilation (MV) and NRM rates were calculated from the date of allo-HSCT to the date of the beginning of the MV and death unrelated to the relapse of the underlying disease, respectively. Death prior to the onset of mechanical ventilation and relapses were considered competing risks. Prognostic value of the severity of pulmonary comorbidity and other potential risk factors for NRM (age, diagnosis, disease status at the time of HSCT, type of donor, protocol of GVHD prophylaxis, year of HSCT, severe acute GVHD) was performed in the Fine-Gray regression model for competing events. Overall survival (OS) was estimated using the Kaplan-Meier method from the date of allo-HSCT to the date of death, or the last contact with the patient. Comparison of survival was performed using the log-rank test.
The two-sided alternative testing hypothesis was applied, being statistically significant at the p-value of <0.05. Statistical analysis was performed using EZR statistical software, version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Clinical characteristics
As of May 1, 2019, 355 patients were included in the study, among them 206 (58%) and 149 (42%) in the retrospective and prospective phases, respectively. The basic demographic and clinical characteristics of the patient cohort are presented in Table 1.
In terms of age, gender, diagnosis and clinical indications for allo-HSCT, donor characteristics, conditioning regimens, the analyzed cohort appears to be representative and generally reflects the current transplant activity in adult patients.
Table 1. The basic demographic and clinical characteristics of patient cohort

Baseline factors of pulmonary comorbidity
At the first stage of the study, we analyzed the baseline potential risk factors and causes of pulmonary comorbidity in the entire patient cohort, as listed in Table 2.
Table 2. Risk factors for pulmonary comorbidity

Tobacco smoking, including high pack-year rates (> 20) for every fourth smoker was most frequent (32%) among the basic risk factors unrelated to the underlying disease and its treatment. A documented diagnosis of COPD and BA was present in, respectively, 15 (4.2%) and 4 (1.1%) of HSCT recipients. It should be noted that the majority of COPD patients (13/15) had a mild-severity disease, and intermittent BA was diagnosed in all 4 cases. The leading group of lung diseases reported before allo-HSCT was presented by pulmonary infections (44.9%), dominated by clinically proven pneumonia (35.8%). In general, microbiological verification of the pathogens in available medical documentation was low, and to a greater extent concerned only invasive mycoses with lung involvement (16%). Ten patients (2.8%) had the history of pulmonary tuberculosis, or radiological signs of previous tuberculosis which required secondary prophylaxis with tuberculostatic drugs.
Frequently used medical drugs with known lung toxicity, e.g., cytarabine (65%), as well as bleomycin (8.2%) and carmustine (5.2%) applied in anticancer chemotherapy before allo-HSCT were also identified as potential risk factors. In addition, 30 (8.5%) and 22 (6.2%) patients had the history of high-dose chemotherapy followed by autologous HSCT and mediastinal therapeutic irradiation, respectively. Use of immune checkpoint inhibitors was considered another particular potential risk factor of pre-HSCT pulmonary injury (5.4% of entire cohort).
In general, statistical evaluation of the potential factors predisposing for pulmonary compromise allowed us to identify two of the most characteristic disease-specific profiles associated with clinical course of the underlying disease and its treatment. The greatest number of risk factors for pulmonary comorbidity was revealed among the patients with lymphomas who received treatment with bleomycin, carmustine, cytarabine, immune checkpoint inhibitors, radiation therapy and autologous HSCT. The second group was represented by patients with acute leukemia and a part of MDS patients who received chemotherapy with cytarabine and showed high incidence of neutropenic pulmonary infections before allo-HSCT. Patients with AA did not exhibit specific drug pulmonary toxicity in anamnesis. However, this group of patients had an increased risk of iron overload, having been associated with multiple blood transfusions.
The proportion of smokers was higher among the patients with lymphomas (41%) and myeloproliferative diseases, and MDS (39%) compared with acute leukemia (30%) and, especially, AA group (19%). However, 48% of smokers with MPD and MDS had a smoking index of more than 20 pack-years, which was significantly higher than for with acute leukemia (22%) and lymphoma patients (21%) (p=0.0461). The frequency of concomitant COPD was significantly higher among patients with MPD and MDS, i.e., 7/54 (13%), compared with 0/27 (0%), 5/215 (2%) and 3/59 (5%) with AA, acute leukemia and lymphomas respectively (p=0.0038).
These patterns are partly explained by differences in the age and the duration of the disease at the time of allo-HSCT. The median age was 28, 32, 37 and 45 years in patients with SAA, acute leukemia, lymphomas and MPD and MDS respectively (p <0.0001). Accordingly, the median time between the diagnosis and allo-HSCT was 1.9, 1.1, 3.6, and 1.4 years (p <0.0001).
Table 3. Frequency of individual pulmonary CT symptoms before allo-HSCT (n=270)

Chest computed tomography (CT) findings at the time of allo-HSCT were available in 270 (76%) patients. Pathological changes in lung structures were documented in 190 (70.6%) of the examined patients (Table 3). The signs of local pulmonary fibrosis and focal changes were the most frequent CT symptoms detected in more than 50% and 30% of patients, respectively.
Pulmonary function tests (PFT)
At the next step of our study, we analyzed data from a pre-HSCT PFT with a focus on the key FEV1 and DLco parameters which are included in HCT-CI comorbidity criteria. Testing of FEV1 and other standard spirometry parameters covered the entire cohort (n=355), while the data on the pulmonary diffusing capacity, including DLco were obtained from 76 patients, predominantly in the prospective phase of the study. The main parameters of spirometry and pulmonary diffusing capacity are presented in Table 4.
FEV1 varied within 49-145% of predicted, the median was 100.6%, the interquartile range was 90-109.6%. According to HCT-CI criteria, 90 (25%) patients had low FEV1 value, including 14%, 9% and 2% of mild, moderate and severe grade respectively.
When verifying alterations of the pulmonary diffusing capacity, two methods were used to adjust the obtained DLco values for the hemoglobin levels. The median hemoglobin level at the time of DLco testing was 10.3 g/dL (5.8-16.4). There was decreased hemoglobin level in 80% of women and 57% of men. Frequency of diffusion disorders by the DLco values seems to be definitely overestimated (96%) when using the Cotes hemoglobin correction method, which is routinely recommended by ATS/ERS experts and used by default in pulmonary practice. The Dinakara method aiming to adjust DLco for hemoglobin levels provided a more accurate assessment and showed DLco disorders in 69% of the examined patients, including 29%, 28% and 12% frequency rates for mild-, moderate- and severe-grade alterations respectively.
Table 4. Pulmonary function tests characteristics before allo-HSCT

When analyzing PFT data in patients with different diagnoses, more frequent bronchial obstruction according to the FEV1/VC parameter was found in the patients with MPD and MDS, whereas disorders of pulmonary diffusing capacity according to the adjusted DLco were more pronounced in patients with lymphomas (Table 5). Other tested parameters did not show significant dependence on the underlying disease.
Table 5. Pulmonary function tests before allo-HSCT according to the diagnosis

In general, taking into account the maximum contribution of FEV1 or DLco data 68 (19%), 49 (14%) and 14 (4%) patients corresponded to the criteria for mild, moderate and severe pulmonary comorbidity, respectively (Table 6).
Table 6. Severity of pulmonary function abnormalities before allo-HSCT


Figure 1. NRM with stratification of patients according to the severity of pulmonary comorbidity

Figure 2. Cumulative incidence of mechanical ventilation with stratification of patients according to the severity of pulmonary comorbidity

Figure 3. Overall survival after allo-HSCT with stratification of patients according to the severity of pulmonary comorbidity
Prognostic value of pulmonary comorbidity for the outcome of allo-HSCT
The prognostic value of pulmonary comorbidity parameters was tested by its analyzing against cumulative incidence of NRM and overall survival (OS) after allo-HSCT. In the whole cohort, NRM and cumulative incidence of relapse in 2 years were 21.0% (95% CI, 16.4-25.9) and 10.5% (95% CI, 7.3-14.3).
Stratification of patients according to the severity of pulmonary comorbidity revealed significant differences in NRM (Fig. 1). The cumulative incidence of death without signs of relapse of the underlying disease within 12 months after allo-HSCT was 13.8% (CI 95%, 9.5-18.9), 14.1% (CI 95%, 6.4-24.7), 26.7% (CI 95%, 14.5-40.4) and 53.2% (CI 95%, 22.1-76.9) with pulmonary comorbidity 0, 1, 2, 3 degrees respectively (p=0.0004).
The value of pulmonary comorbidity was further evaluated by a surrogate criterion of severe respiratory failure with need for mechanical ventilation (MV). Indications for MV occurred in 34 (9.6%) and 54 (15.2%) patients during the first 100 days and 1 year after allo-HSCT, respectively. In two other cases, MV was performed later. In order to reduce the significance of the primary disease relapse, further analysis was carried out for patients who developed severe respiratory failure during the first 100 days after allo-HSCT.
Stratification of patients according to the pulmonary comorbidity revealed a significant increased risk of switching to MV in high-risk patients (Fig. 2). Cumulative incidence of the MV within 100 days from allo-HSCT was 7.2% (CI 95%, 3.8-10.6), 10.9% (CI 95%, 2.9-18.2), 16.7% (CI 95%, 5.4-26.6) and 22.1% (CI 95%, 0-41.3) in patients with pulmonary comorbidity of 0, 1, 2 and 3 degree, respectively (p=0.0176).
Prognostic significance of the degree of pulmonary comorbidity for the risk of NRM was confirmed in a multivariate analysis, using the Fine-Gray regression model for competing events (Table 7). Other factors associated with increased risk of NRM were: primary diagnosis (maximum risk for MPD and MDS, minimum for SAA), lack of remission at the time of allo-HSCT, MAC regimen, type of donor (maximum risk for a haploidentical donor), year of HSCT and the presence of severe acute GVHD (aGVHD).
In contrast to the severity of PFT disorders, none of the potential pulmonary comorbidity factors discussed above (smoking, presence of lung diseases before HSCT, pulmonary toxicity, radiation therapy), as well as the age of patients at the time of allo-HSCT, did not have independent prognostic value.
The risk of relapse after allo-HSCT as expected did not depend from the degree of pulmonary comorbidity. Despite this, due to significant differences in NRM, pulmonary comorbidity was associated with a decrease in overall survival: 71.9% (95% CI, 63.8-78.5), 61.9% (95% CI, 42.5-76.4), 54.3% (95% CI, 36.2-69.1) and 39.0 (95% CI, 14.3-63.3) at 5 years after allo-HSCT with 0, 1, 2, and 3 degrees respectively (p=0.0014) (Fig. 3).
Table 7. Multivariate analysis of characteristics affecting non-relapse mortality

Discussion
The HCT-CI is an important diagnostic tool in screening candidates for allo-HSCT [8, 9, 17]. Despite some inaccuracies with HCT-CI as prognostic indicators, a score of 3 and above always remains a sign of a high-degree risk for relapse-unrelated deaths. Currently, the assessment of the bronchopulmonary condition is one of essential components in pre-transplant examination of the patients, including PFTs with FEV1 and DLco, assessment, as well as chest CT evaluation [19].
The study by M. Sorror and colleagues has revealed that FEV1 and/or DLco reflect a correlation between causes of death and pulmonary comorbid pathology when assessing NRM rates [8]. Of the 347 patients who had moderate or severe degrees of pulmonary comorbidity, 122 died from causes unrelated to the relapse of primary disease. The causes of NRM were severe pulmonary toxicity (24%), pulmonary complications of cGVHD (11%), lower respiratory tract infections (45%) that were associated (18%), or non-associated (27%) with cGVHD, and other causes (20%) [8].
Conventional spirometry is the most common screening method in examining the function of respiratory system. Spirometry is aimed to identify and determine the type of pulmonary function disorders, primarily obstructive, with the Tiffeneau index and FEV1 [20, 21]. Spirometry makes it possible to diagnose broncho-obstructive diseases (BA, COPD, etc.), like as to predict clinical outcomes of the scheduled allo-HSCT [9, 19].
The DLco test is another functional method for assessing the state of lower respiratory tract. It is used to evaluate gas exchange via the alveolar-capillary membrane [20, 21]. The DLco test detects probable interstitial changes of pulmonary tissue in patients with a history of using pulmonary toxic drugs (cytarabine, bleomycin, carmustine, nivolumab, etc.), radiation therapy, as well as changes associated with the course of the underlying disease (specific pulmonary tissue involvement, iron overload, etc.) [20-27].
Despite its obvious diagnostic advantage in identifying “subclinical” pulmonary injuries associated with the course or therapy of oncohematological disease, the DLco study is technically difficult for real clinical practice, thus being rarely performed in routine functional diagnostics.
The main objective of this study was to perform comprehensive analysis of lung health before allo-HSCT, and its connection with development of infectious and non-infectious bronchopulmonary complications in the post-transplant period, as well as NRM rates. Our analysis included 355 adult patients with various neoplastic and benign blood diseases who received allo-HSCT from a related, unrelated, and haploidentical donors. In contrast to previously published data, the analyzed cohort was balanced in terms of conditioning regimen (MAC 40%, RIC 60%) and graft source (BM 38%, G-PBSC 62%) [8-11]. Median age of the patients at the time of allo-HSCT (33 years old) was lower compared with other observations, but the distribution of primary diagnoses did not significantly differ [8, 10, 11]. For the first time, adult patients with SAA (8%) were presented in the cohort.
The study assessed anamnestic data on pre-existing chronic respiratory diseases (COPD, BA) and previous bronchopulmonary infections (pneumonia, invasive mycosis, TBC). In addition, the presence of risk factors for the development of bronchopulmonary diseases (smoking, chemotherapy with pulmonary toxic drugs, mediastinal radiation therapy) was taken into account. In the observed cohort, COPD and BA were documented in 4.2% and 1.1% of patients, respectively, which is significantly lower than the data of the largest international and Russian population-based studies concerning general prevalence of COPD and BA (11.7% and 6.9%) [28]. According to literature data, the prevalence of COPD and BA among HSCT recipients was 2% and 12.2% [8, 29]. This fact can be explained by the negative selection of patients with severe forms of disease at earlier stages of treatment, even before their admission to the HSCT center.
A third of patients had a history of smoking, but a high smoking index was only 8% of patients from the entire cohort, which is comparable with another study, where the incidence of high smoking experience was 14% [30]. Pulmonary infections before allo-HSCT were in 44.9% of patients, among which pneumonia (35.8%), invasive mycosis (16%) and TBC (2.8%) prevailed. These data are similar to the results previously published by our group [31]. History of potential pulmonary toxic chemotherapy was documented in 72% of patients. However, no cases of drug-induced interstitial lung disease (DIILD) were detected in the analyzed cohort. According to available literature, the frequency of cytarabine-related DIILD varies from 15 to 44%, whereas for bleomycin, this condition is found in 6.8-21% of the patients [32-36]. The novel form of DIILD caused by nivolumab may be as frequent as in 11.7% of cases [37].
Pulmonary changes according to chest CT before allo-HSCT were detected in 71% of patients, including signs of local pulmonary fibrosis (58%) and focal changes (38%). An earlier study detected CT changes in 48% of patients with AML, ALL, and MDS before allo-HSCT [38]. Unlike our data, the foci in pulmonary tissue (46%) and ground-glass opacities (17%) were the most frequent CT symptoms. CT signs of terminal bronchiolitis, cavities and pleural effusion have also been detected relatively rarely.
Analysis of PFT parameters was carried out in the entire cohort of patients, as well as in groups of patients with different hematological disorders. Based on the HCT-CI criteria, we analyzed patients with mild, moderate, and severe degrees of pulmonary comorbidity [8]. The median FEV1 (106%) was higher than that shown in other multicenter studies, while the frequency of FEV1 decline was mild (14%), moderate (9%) and severe (2%), which did not significantly differ from earlier literature data [10-11].
In the present study we compared two methods of DLco adjustment for hemoglobin level: the method proposed by J.E. Cotes et al., recommended by ATS/ERS which is more commonly used in pulmonary practice, as well as the Dinakara method used by the Fred Hutchinson Cancer Research Center [15-18, 39-42]. According to our data, the Dinakara method seems to more precisely correct the impact of anemia to a decrease in DLco, which is comparable with similar results from another clinical study [42]. As a result, there was a decrease in DLco of mild (29%), moderate (28%) and severe (12%) degrees, which is comparable with the reported results of other observations [10-11].
Analysis of PFT parameters in patients with various hematological diseases revealed a decrease in the Tiffeneau index in patients with MPD and MDS, as well as a reduced DLco in patients with lymphomas. This relationship is not described in the literature, which is probably due to the previously low transplant activity in these groups of patients. It can be assumed that these disease-specific relationships are caused by the age of the patients, the history of pulmonary toxicity and radiation therapy, the length of smoking and proven COPD.
The key result of the study was a strong confirmation of the high prognostic significance of pulmonary comorbidity for allo-HSCT outcomes in the real-world practice and in context of changing transplant landscape [8, 10]. The patients with moderate and severe pulmonary comorbidity showed a 2- 3 fold increase in the cumulative incidence of MV requirements in the early post-transplant period. At the same time, the risk of NRM increased 2-4 times if compared to the patients without documented pulmonary comorbidity. Despite lacking differences in the frequency of relapses of the underlying disease, an association was found between moderate and, especially, severe degrees of pulmonary comorbidity and a decrease in overall survival.
Our study had a number of limitations, in particular, incomplete coverage of the cohort with DLco testing data in retrospective phase, which could cause underestimation of pulmonary comorbidity. However, taking into account the above-described features of a cohort based on the representation of different diagnoses, donor types, transplant sources, conditioning regimens and GVHD prophylaxis, the independent prognostic value of pulmonary comorbidity, as confirmed by multivariate analysis, is of particular importance.
Conclusion
Adult recipients of allogeneic HSCs have a wide range of potential causes and a high incidence of pulmonary comorbidity: non-infectious (5%) and infectious (45%) lung diseases, history of potential pulmonary toxicity (72%), lung changes according to CT (70%), disorders of respiratory function according to FEV1 (25%) and aDLco (69%). Pulmonary comorbidity and the frequency of violations of respiratory function have some disease-specific features.
In real practice, the use of a screening level of the PFT (spirometry) underestimates or incorrectly assesses the frequency of respiratory disorders in patients before allo-HSCT. The traditional DLco correction for hemoglobin level according to the Cotes method does not accurately reflect the contribution of anemia to impaired pulmonary diffusion capacity in adult patients with blood diseases and leads to an overestimated frequency of detecting severe violations of respiratory function before allo-HSCT. The Dinakara method provides more accurate DLco correction for hemoglobin levels.
In the modern landscape of allo-HSCT with a changing spectrum of indications, age of patients, conditioning regimens, GVHD prophylaxis, the degree of pulmonary comorbidity according to HCT-CI still retains a high predictive value in terms of risk of the MV and NRM.
Conflict of interest
The authors report no conflicts of interest.
References
- Afanasyev BV, Zubarovskaya LS, Moiseev IS. Allogeneic hematopoietic stem cell transplantation in children: now, problems and prospects. Russian J Pediatric Hematol Oncol. 2015;2(2):28-42. (In Russian).
- Savchenko VG, Liubimova LS, Parovichnikova EN, Mendeleeva LP, Mamotiuk KS, Demidova IA, Gribanova EO, Gal'tseva IV, Pokrovskaia OS, Kuz'mina LA, Zhelnova EI, Kliasova GA, Glasko EN, Kaplanskaia IB, Poreshina LP, et al. Transplantations of allogenic and autologous hemopoietic stem cells in acute leukemia (results of 20-year experience). Terapevticheskiy arkhiv. 2007;79 (7):30-35. (In Russian).
- Rumyantsev AG, Maschan AA Hematopoietic stem cell transplantation in children. M.: Medical Information Agency, 2003. 909 pp. (In Russian.)
- Duarte RF, Labopin M, Bader P, Basak GW, Bonini C, Chabannon C, Corbacioglu S, Dreger P, Dufour C, Gennery AR, Kuball J, Lankester AC, Lanza F, Montoto S, Nagler A, de Latour RP, Snowden JA, Styczynski J, Yakoub-Agha I, Kröger N, Mohty M for the European Society for Blood and Marrow Transplantation (EBMT). Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant. 2019:1-28. Published: 05 April 2019. doi.org/10.1038/s41409-019-0516-2.
- Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, Martin PJ, Sandmaier BM, Marr KA, Appelbaum FR, Storb R, McDonald GB. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010;363(22):2091-2101.
- Horan JT, Logan BR, Agovi-Johnson M-A, Lazarus HM, Bacigalupo AA, Ballen KK, Bredeson CN, Carabasi MH, Gupta V, Hale GA, Khoury HJ, Juckett MB, Litzow MR, Martino R, McCarthy PL, Smith FO, Rizzo JD, Pasquini MC. Reducing the risk for transplantation-related mortality after allogeneic hematopoietic cell transplantation: how much progress has been made? J Clin Oncol. 2011;29(7):806-813.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383.
- Sorror ML, Maris MB, Storb RF, Sandmaier MB, Maloney DG, Storrer B. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106(8):2912-2919.
- Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB, Bhatia S, Ostronoff F, Deeg MH, Syrjala KL, Estey E, Maloney DG, Appelbaum FR, Martin PJ, Storer BE. Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol. 2014;32(29):3249-3256.
- Parimon T, Madtes DK, Au DH, Clark JG, Chien JW. Pretransplant lung function, respiratory failure, and mortality after stem cell transplantation. Am J Respir Crit Care Med. 2005;172(3):384-390.
- Piñana JL, Martino L, Barba P, Bellido-Cassado J, Valcarcel D, Sureda A, Briones J, Brunet S, Rodriguez-Arias JM, Casan P, Sierra J. Pulmonary function testing prior to reduced intensity conditioning allogeneic stem cell transplantation in an unselected patient cohort predicts posttransplantation pulmonary complications and outcome. Am J Hematol. 2012;87(1):9-14.
- Dobronravov VA, Smirnov KA, Afanasiev BV, Galkina OV, Smirnov AV. Subclinical tubular epithelium damage and acute kidney injury following allogeneic hematopoietic stem cell transplantation. Cell Ther Transplant. 2016; 5(4):8-14.
- Roziakova L, Mistrik M, Batorova A, Kruzliak P, Bojtarova E, Dubrava J, Gergel J, Mladosievicova B. Can we predict clinical cardiotoxicity with cardiac biomarkers in patients after haematopoietic stem cell transplantation? Cardiovasc Toxicol. 2015;15(3):210-216.
- Wu AC, Kiley JP, Noel PJ, Amur S, Burghard EG, Clancy JP, Galanter J, Inada M, Jones TK, Kropski JA, Loyd JE, Nogee LM, Raby BA, Rogers AJ, Schwartz DA, Sin DD, Spira A, Weiss ST, Young LR, Himes BE. Current status and future opportunities in lung precision medicine research with a focus on biomarkers. An American Thoracic Society/National Heart, Lung, and Blood Institute Research Statement. Am J Respir Crit Care Med. 2018;198(12):116-136.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CPM, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre M, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J. Interpretive strategies for lung function tests. Eur Respir J. 2005;26(5):948–968.
- Cotes J. E. Measurement of the transfer factor (diffusing capacity) for the lung and its subdivisions. Lung function assessment application in medicine. 4th ed. Oxford, UK: Blackwell Scientific Publications. 1979:230-250.
- Dinakara P, Blumenthal WS, Johnston RF, Kauffman LA, Solnick PB. The effect of anemia on pulmonary diffusing capacity with derivation of a correction equation. Am Rev Respir Dis. 1970:102(6):965-969.
- Clement RF. Fundamental and methodological foundations for the development of a unified system of proper quantities. Current problems of clinical respiratory physiology. 1987:5-19. (In Russian).
- Carreras E, Dufor C, Mohty M, Kröger N. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies. Springer. 2019:77-86.
- Chuchalin AG. Pulmonology. National guidelines. Moscow: GEOTAR-Media. 2012: 117-135. (In Russian).
- Savushkina OI, Chernyak AV. Pulmonary functional tests: from theory to practice. A guide for doctors. Moscow: Strom. 2017:11-38; 63-82. (In Russian).
- Skeoch S, Weatherley N, Swift AJ, Oldroyd A, Johns C, Hayton C, Giollo A, Wild JM, Waterton JC, Buch M, Linton K, Bruce IN, Leonard C, Bianchi S, Chaudhuri N. Drug-induced interstitial lung disease: a systematic review. J Clin Med. 2018;7(10):1-30.
- DeMonaco NA, McCarty Jr KS, Joyce J, Jacobs SA. Focal radiation fibrosis after radioimmunotherapy for follicular non-Hodgkin lymphoma. Clin Lymphoma Myeloma. 2007;7(5):369-372.
- Guner SI, Yanmaz MT, Selvi A, Usul C. Chemotherapy and radiation induced pulmonary dysfunction in Hodgkin lymphoma patients. Indian J Hematol Blood Transfus. 2016;32(4):431-436.
- Berkman N, Breuer R, Kramer MR, Polliack A. Pulmonary involvement in lymphoma. Leuk Lymphoma. 1996;20(3-4):229-237.
- Mian M, Wasle I, Gritsch S, Willenbacher W, Fiegl M. B cell lymphoma with lung involvement: what is it about? Acta Haematol. 2015;133(2):221-225.
- Kamble R, Rosenzweig T. Diffuse pulmonary parenchymal involvement in multiple myeloma: antemortem diagnosis. Int J Hematol. 2006;83(3):259-261.
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2017 update. 2017:13-24. Available at: http://www.ginasthma.org. Accessed June 23, 2017.
- Chien SH, Liu C-J, Hong Y-C, Teng C-J, Hu Y-W, Shen C-C, Ku F-C, Chen S-C, Yeh C-M, Chiou T-J, Gau J-P, Tzeng C-H. Use of azathioprine for graft-vs-host disease is the major risk for development of secondary malignancies after haematopoietic stem cell transplantation: a nationwide population-based study. Br J Cancer. 2015;112(1):177-184.
- Mehdi A, Rybicki L, Mossad S, Yurch M, Sekeres M, Gerds AT, Jagadeesh D, Hamilton B, Liu H, Dean R, Pohlman B, Sobecks R, Andresen S, Kalaycio M, Bolwell BJ, Majhail MS, Copelan E, Hill BT. Impact of cigarette smoking on survival after myeloablative allogeneic hematopoietic stem cell transplantation and contribution of invasive fungal infection. Bone Marrow Transplant. 2017;52(12);1665-1667.
- Popova MO, Ekushov KA, Ayzsilnieks OV, Volkova AG, Pinegina ON, Ignatieva SM, Slesarchuk OA, Vladovskaya MD, Bondarenko SN, Zubarovskaya LS, Klimko NN, Afanasyev BV. Invasive fungal infections in recipients of allogeneic hematopoietic stem cell teens and young adults. Russian J Pediatric Hematol Oncol. 2016; (1):44-51. (In Russian).
- Ilkovich MM. Interstitial and orphan lung diseases. Moscow: GEOTAR-Media. 2016:289-316 (In Russian).
- Blum RH, Carter SK, Agre K. A clinical review of bleomycin – a new antineoplastic agent. Cancer. 1973;31(4):903-914.
- Hubbard SP, Chabner BA, Canellos GP, Young RC, DeVita Jr. VT. High dose intravenous bleomycin in the treatment of advanced lymphomas. Eur J Cancer. 1975;11(9):623-626.
- Ngeow J, Tan IB, Kanesvaran R, Tan HC, Tao M, Quek R, Lim ST. Prognostic impact of bleomycin-induced pneumonitis on the outcome of Hodgkin’s lymphoma. Ann Hematol. 2011;90(1):67-72.
- Stamatoullas A, Brice P, Bouabdallah R, Mareschal S, Camus V, Rahal I, Franchi P, Lanic H, Tilly H. Outcome of patients older than 60 years with classical Hodgkin lymphoma treated with front line ABVD chemotherapy: frequent pulmonary events suggest limiting the use of bleomycin in the elderly. Br J Haematol. 2015;170(2):179-184.
- Nishino M, Ramaiya NH, Awad MM, Sholl LM, Maattala JA, Taibi M, Hatabu H, Ott PA, Armand PF, Hodi FS. PD-1 inhibitor-related pneumonitis in advanced cancer patients: radiographic patterns and clinical course. Clin Cancer Res. 2016;22(24):6051-6060.
- El Boghdadly Z, Oran B, Rondon JG, Champlin R, Kontoiyannis DP. Pretransplant chest computed tomography screening in asymptomatic patients with leukemia and myelodysplastic syndrome. Bone Marrow Transplant. 2017;52(3):476-479.
- Sorror ML. How I assess comorbidities before hematopoietic cell transplantation. Blood. 2013;121(15):2854-2863.
- Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, Maziarz RT, Antin JH, Soiffer RJ, Weisdorf DJ, Rizzo D, Horowitz MM, Saber W. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123(23):3664-3671.
- Shouval R, Labopin M, Bondi O, Mishan Shamay H, Shimoni A, Ciceri F, Esteve Reiner J, Giebel S, Gorin NC, Schmid C, Polge E, Aljurf M, Kroger N, Craddock CF, Bacigalupo A, Cornelissen JJ, Baron F, Under R, Nagler A, Mohty M. Prediction of allogeneic hematopoietic stem-cell transplantation mortality 100 days after transplantation using a machine learning algorithm: a European Group for Blood and Marrow Transplantation Acute Leukemia Working Party Retrospective Data Mining Study. J Clin Oncol. 2015;33(28):3144-3151.
- Coffey DG, Pollyea DA, Myint H, Smith C, Gutman JA. Adjusting DLCO for Hb and its effects on the Hematopoietic Cell Transplantation-specific Comorbidity Index. Bone Marrow Transplant. 2013;48(9):1253-1256.
Егор А. Кулагин 1, Алиса Г. Волкова 2, Илья Ю. Николаев 2, Олег В. Голощапов 2, Анна Г. Смирнова 2, Татьяна А. Рудакова 2, Елена И. Дарская 2, Елена В. Морозова 2, Наталья Б. Михайлова 2, Юлия Д. Рабик 3, Виктория Г. Тимчик 3, Татьяна И. Щемелинина 3, Руфь Д. Скворцова 3, Татьяна С. Разумовская 3, Сергей Н. Бондаренко 2, Иван С. Моисеев 2, Валерий Н. Марченко 1, Василий И. Трофимов 1, Борис В. Афанасьев 2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22618" ["VALUE"]=> array(2) { ["TEXT"]=> string(955) "<p><sup>1</sup> Кафедра госпитальной терапии с курсом аллергологии и иммунологии имени академика М.В. Черноруцкого, Санкт-Петербург, Россия<br> <sup>2</sup> НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Санкт-Петербург, Россия<br> <sup>3</sup> Отделение функциональной диагностики №2 Научно-клинического исследовательского центра, ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова» Минздрава России, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(895) "1 Кафедра госпитальной терапии с курсом аллергологии и иммунологии имени академика М.В. Черноруцкого, Санкт-Петербург, Россия
2 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Санкт-Петербург, Россия
3 Отделение функциональной диагностики №2 Научно-клинического исследовательского центра,
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова» Минздрава России, Санкт-Петербург, Россия
Высокая эффективность аллогенной трансплантации гемопоэтических стволовых клеток (алло- ТГСК) при широком спектре злокачественных и незлокачественных заболеваний системы крови ограничивается риском тяжелых осложнений и летального исхода без признаков рецидива или прогрессирования основного заболевания (безрецидивная летальность). Среди ключевых факторов безрецидивной летальности рассматривается коморбидность до момента алло-ТГСК. Целью настоящего исследования было охарактеризовать потенциальные предтрансплантационные факторы легочной коморбидности и интегральные показатели функции внешнего дыхания (ФВД) и оценить их прогностическое значение для исходов алло-ТГСК у взрослых пациентов.
Пациенты и методы
Исследование включало 355 больных, в том числе 149 (42%) в проспективной фазе исследования. Сформированная когорта включала пациентов с острыми лейкозами (60%), миелопролифератив-
ными заболеваниями (10%), миелодиспластическим синдромом (5%), лимфомами (17%) и тяжелой апластической анемией (8%). Медиана возраста на момент алло-ТГСК составила 33 года (18-66). Анализировались все потенциальные предтрансплантационные факторы легочной компрометации. Степень тяжести легочной коморбидности оценивалась на основании параметров ФВД – объема форсированного выдоха за первую секунду (ОФВ1) и диффузионной способности лёгких для оксида углерода (CO) (DLco) в соответствии с критериями индекса коморбидности Hematopoietic cell transplantation specific comorbidity index (HCT-CI). Прогностическое значение степени легочной коморбидности исследовано в отношении кумулятивной частоты перевода на искусственную вентиляцию легких (ИВЛ) и безрецидивной летальности.
Результаты
Среди наиболее частых факторов легочной компрометации до алло-ТГСК идентифицированы курение (32%), анамнез хронической обструктивной болезни легких (ХОБЛ) и бронхиальной астмы (БА) (5%), инфекции легких (45%), потенциально пульмонотоксичная химиотерапия (79%), аутологичная ТГСК (8%), ингибиторы иммунных контрольных точек (5%), лучевая терапия на область средостения (6%) и др. Критериальное снижение ОФВ1 от должного имело место у 90 (25%) больных, включая 14%, 9% и 2% легкой, средней и тяжелой степени соответственно. Нарушение DLco было выявлено у 69% обследованных пациентов, включая 29%, 28% и 12% легкой, средней и тяжелой степени соответственно. Кумулятивная частота перевода на ИВЛ в течение 100 дней после алло-ТГСК составила 7,2%, 10,9%, 16,7% и 22,1% у пациентов с легочной коморбидностью 0, 1, 2, 3 степени соответственно. Степень легочной коморбидности была независимым фактором риска безрецидивной летальности (отношение рисков 1,39, ДИ 95%, 1.03-1.89, p=0.033) и ассоциировалась со снижением общей выживаемости.
Выводы
Взрослые пациенты имеют широкий спектр факторов легочной коморбидности до алло-ТГСК. Легочная коморбидность по HCT-CI является фактором риска перевода на ИВЛ в течение первых 100 дней после алло-ТГСК и безрецидивной летальности.
Ключевые слова
Аллогенная трансплантация гемопоэтических стволовых клеток, взрослые, коморбидная патология легких, функция внешнего дыхания, клинический прогноз.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22596" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-26-37" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-26-37" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22716" ["VALUE"]=> array(2) { ["TEXT"]=> string(878) "<p>Egor A. Kulagin <sup>1</sup>, Alisa G. Volkova <sup>2</sup>, Ilya Yu. Nikolaev <sup>2</sup>, Oleg V. Goloshchapov <sup>2</sup>, Anna G. Smirnova <sup>2</sup>, Tatiana A. Rudakova <sup>2</sup>, Elena I. Darskaya <sup>2</sup>, Elena V. Morozova <sup>2</sup>, Nataliya B. Mikhaylova <sup>2</sup>, Julia D. Rabik <sup>3</sup>, Victoria G. Timchik <sup>3</sup>, Tatiana I. Shchemelinina <sup>3</sup>, Ruf D. Skvortsova <sup>3</sup>, Tatiana S. Razumovskaya <sup>3</sup>, Sergey N. Bondarenko <sup>2</sup>, Ivan S. Moiseev <sup>2</sup>, Valeriy N. Marchenko <sup>1</sup>, Vasiliy I. Trofimov <sup>1</sup>, Boris V. Afanasyev <sup>2</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(638) "Egor A. Kulagin 1, Alisa G. Volkova 2, Ilya Yu. Nikolaev 2, Oleg V. Goloshchapov 2, Anna G. Smirnova 2, Tatiana A. Rudakova 2, Elena I. Darskaya 2, Elena V. Morozova 2, Nataliya B. Mikhaylova 2, Julia D. Rabik 3, Victoria G. Timchik 3, Tatiana I. Shchemelinina 3, Ruf D. Skvortsova 3, Tatiana S. Razumovskaya 3, Sergey N. Bondarenko 2, Ivan S. Moiseev 2, Valeriy N. Marchenko 1, Vasiliy I. Trofimov 1, Boris V. Afanasyev 2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22717" ["VALUE"]=> array(2) { ["TEXT"]=> string(544) "<p><sup>1</sup> M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br> <sup>2</sup> Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br> <sup>3</sup> Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(484) "1 M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
3 Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
High efficacy of allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a wide range of malignant and non-malignant hematopoietic disorders system is limited to the risk of serious complications and non-relapse mortality (NRM). Pre-existing comorbidities before allo-HSCT are among key factors for NRM.
The purpose of this study was to characterize the potential pre-transplant factors of pulmonary comorbidity and integral indicators of pulmonary function tests (PFT) and to evaluate their prognostic value for the allo-HSCT outcomes in adult patients.
Patients and methods
The study included 355 patients, among them 149 (42%) in the prospective phase of the study. The cohort included patients with acute leukemia (60%), myeloproliferative diseases (10%), myelodysplastic syndrome (5%), lymphomas (17%), and severe aplastic anemia (8%). The median age at the time of allo-HSCT was 33 years old (18 to 66). We analyzed all the factors that could affect lung function before allo-HSCT. The severity of pulmonary comorbidity was assessed on the basis of forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco), in accordance with the criteria of the Hematopoietic Cell Transplantation Specific Comorbidity Index (HCT-CI). The prognostic value of pulmonary comorbidity was investigated with respect to the cumulative incidence of mechanical ventilation (MV) and NRM rates.
Results
Tobacco smoking (32%), history of chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) (5%), previous pulmonary infections (45%), potentially pulmonary toxic chemotherapy (79%), previous auto-HSCT (8%), usage of immune checkpoint inhibitors (5%), mediastinal radiation therapy (6%) were the most common pulmonary compromising factors before allo-HSCT. According to the HCT-CI criteria, 90 patients (25%) had low FEV1 values, with 14%, 9% and 2% of mild, moderate and severe grade respectively. DLco disorders were diagnosed in 69% of the patients examined, including 29%, 28%, and 12% of mild, moderate, and severe grade respectively. Cumulative incidence of MV within 100 days after allo-HSCT was 7.2%, 10.9%, 16.7%, and 22.1% in patients with pulmonary comorbidity of 0, 1, 2, 3 degrees, respectively. The degree of pulmonary comorbidity was an independent risk factor for NRM (hazard ratio 1.39; CI 95%; 1.03-1.89; p=0.033), being associated with a decrease in overall survival (OS).
Conclusions
Adult patients have a wide range of pulmonary comorbidity factors before allo-HSCT. HCT-CI pulmonary comorbidity is an independent risk factor for MV during the first 100 days after allo-HSCT and NRM.
Keywords
Allogeneic hematopoietic stem cell transplantation, adults, pulmonary comorbidity, pulmonary functional tests, clinical prognosis.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22597" ["VALUE"]=> string(166) "Clinical features and prognostic value of functional disorders and pulmonary comorbidity in adult patients prior to allogeneic hematopoietic stem cell transplantation" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(166) "Clinical features and prognostic value of functional disorders and pulmonary comorbidity in adult patients prior to allogeneic hematopoietic stem cell transplantation" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22620" ["VALUE"]=> string(4) "1649" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1649" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22719" ["VALUE"]=> string(4) "1650" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1650" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(12) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22716" ["VALUE"]=> array(2) { ["TEXT"]=> string(878) "<p>Egor A. Kulagin <sup>1</sup>, Alisa G. Volkova <sup>2</sup>, Ilya Yu. Nikolaev <sup>2</sup>, Oleg V. Goloshchapov <sup>2</sup>, Anna G. Smirnova <sup>2</sup>, Tatiana A. Rudakova <sup>2</sup>, Elena I. Darskaya <sup>2</sup>, Elena V. Morozova <sup>2</sup>, Nataliya B. Mikhaylova <sup>2</sup>, Julia D. Rabik <sup>3</sup>, Victoria G. Timchik <sup>3</sup>, Tatiana I. Shchemelinina <sup>3</sup>, Ruf D. Skvortsova <sup>3</sup>, Tatiana S. Razumovskaya <sup>3</sup>, Sergey N. Bondarenko <sup>2</sup>, Ivan S. Moiseev <sup>2</sup>, Valeriy N. Marchenko <sup>1</sup>, Vasiliy I. Trofimov <sup>1</sup>, Boris V. Afanasyev <sup>2</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(638) "Egor A. Kulagin 1, Alisa G. Volkova 2, Ilya Yu. Nikolaev 2, Oleg V. Goloshchapov 2, Anna G. Smirnova 2, Tatiana A. Rudakova 2, Elena I. Darskaya 2, Elena V. Morozova 2, Nataliya B. Mikhaylova 2, Julia D. Rabik 3, Victoria G. Timchik 3, Tatiana I. Shchemelinina 3, Ruf D. Skvortsova 3, Tatiana S. Razumovskaya 3, Sergey N. Bondarenko 2, Ivan S. Moiseev 2, Valeriy N. Marchenko 1, Vasiliy I. Trofimov 1, Boris V. Afanasyev 2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(638) "Egor A. Kulagin 1, Alisa G. Volkova 2, Ilya Yu. Nikolaev 2, Oleg V. Goloshchapov 2, Anna G. Smirnova 2, Tatiana A. Rudakova 2, Elena I. Darskaya 2, Elena V. Morozova 2, Nataliya B. Mikhaylova 2, Julia D. Rabik 3, Victoria G. Timchik 3, Tatiana I. Shchemelinina 3, Ruf D. Skvortsova 3, Tatiana S. Razumovskaya 3, Sergey N. Bondarenko 2, Ivan S. Moiseev 2, Valeriy N. Marchenko 1, Vasiliy I. Trofimov 1, Boris V. Afanasyev 2
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22718" ["VALUE"]=> array(2) { ["TEXT"]=> string(3239) "<p style="text-align: justify;">High efficacy of allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a wide range of malignant and non-malignant hematopoietic disorders system is limited to the risk of serious complications and non-relapse mortality (NRM). Pre-existing comorbidities before allo-HSCT are among key factors for NRM.</p> <p style="text-align: justify;">The purpose of this study was to characterize the potential pre-transplant factors of pulmonary comorbidity and integral indicators of pulmonary function tests (PFT) and to evaluate their prognostic value for the allo-HSCT outcomes in adult patients.</p> <h3>Patients and methods</h3> <p style="text-align: justify;">The study included 355 patients, among them 149 (42%) in the prospective phase of the study. The cohort included patients with acute leukemia (60%), myeloproliferative diseases (10%), myelodysplastic syndrome (5%), lymphomas (17%), and severe aplastic anemia (8%). The median age at the time of allo-HSCT was 33 years old (18 to 66). We analyzed all the factors that could affect lung function before allo-HSCT. The severity of pulmonary comorbidity was assessed on the basis of forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco), in accordance with the criteria of the Hematopoietic Cell Transplantation Specific Comorbidity Index (HCT-CI). The prognostic value of pulmonary comorbidity was investigated with respect to the cumulative incidence of mechanical ventilation (MV) and NRM rates.</p> <h3>Results</h3> <p style="text-align: justify;">Tobacco smoking (32%), history of chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) (5%), previous pulmonary infections (45%), potentially pulmonary toxic chemotherapy (79%), previous auto-HSCT (8%), usage of immune checkpoint inhibitors (5%), mediastinal radiation therapy (6%) were the most common pulmonary compromising factors before allo-HSCT. According to the HCT-CI criteria, 90 patients (25%) had low FEV1 values, with 14%, 9% and 2% of mild, moderate and severe grade respectively. DLco disorders were diagnosed in 69% of the patients examined, including 29%, 28%, and 12% of mild, moderate, and severe grade respectively. Cumulative incidence of MV within 100 days after allo-HSCT was 7.2%, 10.9%, 16.7%, and 22.1% in patients with pulmonary comorbidity of 0, 1, 2, 3 degrees, respectively. The degree of pulmonary comorbidity was an independent risk factor for NRM (hazard ratio 1.39; CI 95%; 1.03-1.89; p=0.033), being associated with a decrease in overall survival (OS).</p> <h3>Conclusions</h3> <p style="text-align: justify;">Adult patients have a wide range of pulmonary comorbidity factors before allo-HSCT. HCT-CI pulmonary comorbidity is an independent risk factor for MV during the first 100 days after allo-HSCT and NRM. </p> <h2>Keywords</h2> <p style="text-align: justify;">Allogeneic hematopoietic stem cell transplantation, adults, pulmonary comorbidity, pulmonary functional tests, clinical prognosis. </p> " ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3059) "High efficacy of allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a wide range of malignant and non-malignant hematopoietic disorders system is limited to the risk of serious complications and non-relapse mortality (NRM). Pre-existing comorbidities before allo-HSCT are among key factors for NRM.
The purpose of this study was to characterize the potential pre-transplant factors of pulmonary comorbidity and integral indicators of pulmonary function tests (PFT) and to evaluate their prognostic value for the allo-HSCT outcomes in adult patients.
Patients and methods
The study included 355 patients, among them 149 (42%) in the prospective phase of the study. The cohort included patients with acute leukemia (60%), myeloproliferative diseases (10%), myelodysplastic syndrome (5%), lymphomas (17%), and severe aplastic anemia (8%). The median age at the time of allo-HSCT was 33 years old (18 to 66). We analyzed all the factors that could affect lung function before allo-HSCT. The severity of pulmonary comorbidity was assessed on the basis of forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco), in accordance with the criteria of the Hematopoietic Cell Transplantation Specific Comorbidity Index (HCT-CI). The prognostic value of pulmonary comorbidity was investigated with respect to the cumulative incidence of mechanical ventilation (MV) and NRM rates.
Results
Tobacco smoking (32%), history of chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) (5%), previous pulmonary infections (45%), potentially pulmonary toxic chemotherapy (79%), previous auto-HSCT (8%), usage of immune checkpoint inhibitors (5%), mediastinal radiation therapy (6%) were the most common pulmonary compromising factors before allo-HSCT. According to the HCT-CI criteria, 90 patients (25%) had low FEV1 values, with 14%, 9% and 2% of mild, moderate and severe grade respectively. DLco disorders were diagnosed in 69% of the patients examined, including 29%, 28%, and 12% of mild, moderate, and severe grade respectively. Cumulative incidence of MV within 100 days after allo-HSCT was 7.2%, 10.9%, 16.7%, and 22.1% in patients with pulmonary comorbidity of 0, 1, 2, 3 degrees, respectively. The degree of pulmonary comorbidity was an independent risk factor for NRM (hazard ratio 1.39; CI 95%; 1.03-1.89; p=0.033), being associated with a decrease in overall survival (OS).
Conclusions
Adult patients have a wide range of pulmonary comorbidity factors before allo-HSCT. HCT-CI pulmonary comorbidity is an independent risk factor for MV during the first 100 days after allo-HSCT and NRM.
Keywords
Allogeneic hematopoietic stem cell transplantation, adults, pulmonary comorbidity, pulmonary functional tests, clinical prognosis.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(3059) "High efficacy of allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a wide range of malignant and non-malignant hematopoietic disorders system is limited to the risk of serious complications and non-relapse mortality (NRM). Pre-existing comorbidities before allo-HSCT are among key factors for NRM.
The purpose of this study was to characterize the potential pre-transplant factors of pulmonary comorbidity and integral indicators of pulmonary function tests (PFT) and to evaluate their prognostic value for the allo-HSCT outcomes in adult patients.
Patients and methods
The study included 355 patients, among them 149 (42%) in the prospective phase of the study. The cohort included patients with acute leukemia (60%), myeloproliferative diseases (10%), myelodysplastic syndrome (5%), lymphomas (17%), and severe aplastic anemia (8%). The median age at the time of allo-HSCT was 33 years old (18 to 66). We analyzed all the factors that could affect lung function before allo-HSCT. The severity of pulmonary comorbidity was assessed on the basis of forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco), in accordance with the criteria of the Hematopoietic Cell Transplantation Specific Comorbidity Index (HCT-CI). The prognostic value of pulmonary comorbidity was investigated with respect to the cumulative incidence of mechanical ventilation (MV) and NRM rates.
Results
Tobacco smoking (32%), history of chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) (5%), previous pulmonary infections (45%), potentially pulmonary toxic chemotherapy (79%), previous auto-HSCT (8%), usage of immune checkpoint inhibitors (5%), mediastinal radiation therapy (6%) were the most common pulmonary compromising factors before allo-HSCT. According to the HCT-CI criteria, 90 patients (25%) had low FEV1 values, with 14%, 9% and 2% of mild, moderate and severe grade respectively. DLco disorders were diagnosed in 69% of the patients examined, including 29%, 28%, and 12% of mild, moderate, and severe grade respectively. Cumulative incidence of MV within 100 days after allo-HSCT was 7.2%, 10.9%, 16.7%, and 22.1% in patients with pulmonary comorbidity of 0, 1, 2, 3 degrees, respectively. The degree of pulmonary comorbidity was an independent risk factor for NRM (hazard ratio 1.39; CI 95%; 1.03-1.89; p=0.033), being associated with a decrease in overall survival (OS).
Conclusions
Adult patients have a wide range of pulmonary comorbidity factors before allo-HSCT. HCT-CI pulmonary comorbidity is an independent risk factor for MV during the first 100 days after allo-HSCT and NRM.
Keywords
Allogeneic hematopoietic stem cell transplantation, adults, pulmonary comorbidity, pulmonary functional tests, clinical prognosis.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22596" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-26-37" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-26-37" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-26-37" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22597" ["VALUE"]=> string(166) "Clinical features and prognostic value of functional disorders and pulmonary comorbidity in adult patients prior to allogeneic hematopoietic stem cell transplantation" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(166) "Clinical features and prognostic value of functional disorders and pulmonary comorbidity in adult patients prior to allogeneic hematopoietic stem cell transplantation" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(166) "Clinical features and prognostic value of functional disorders and pulmonary comorbidity in adult patients prior to allogeneic hematopoietic stem cell transplantation" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22717" ["VALUE"]=> array(2) { ["TEXT"]=> string(544) "<p><sup>1</sup> M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br> <sup>2</sup> Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br> <sup>3</sup> Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(484) "1 M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
3 Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
1 M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
3 Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
Егор А. Кулагин 1, Алиса Г. Волкова 2, Илья Ю. Николаев 2, Олег В. Голощапов 2, Анна Г. Смирнова 2, Татьяна А. Рудакова 2, Елена И. Дарская 2, Елена В. Морозова 2, Наталья Б. Михайлова 2, Юлия Д. Рабик 3, Виктория Г. Тимчик 3, Татьяна И. Щемелинина 3, Руфь Д. Скворцова 3, Татьяна С. Разумовская 3, Сергей Н. Бондаренко 2, Иван С. Моисеев 2, Валерий Н. Марченко 1, Василий И. Трофимов 1, Борис В. Афанасьев 2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(903) "Егор А. Кулагин 1, Алиса Г. Волкова 2, Илья Ю. Николаев 2, Олег В. Голощапов 2, Анна Г. Смирнова 2, Татьяна А. Рудакова 2, Елена И. Дарская 2, Елена В. Морозова 2, Наталья Б. Михайлова 2, Юлия Д. Рабик 3, Виктория Г. Тимчик 3, Татьяна И. Щемелинина 3, Руфь Д. Скворцова 3, Татьяна С. Разумовская 3, Сергей Н. Бондаренко 2, Иван С. Моисеев 2, Валерий Н. Марченко 1, Василий И. Трофимов 1, Борис В. Афанасьев 2
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22574" ["VALUE"]=> string(22) "07/30/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "07/30/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "07/30/2019 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22575" ["VALUE"]=> string(22) "08/09/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "08/09/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "08/09/2019 12:00:00 am" } ["CONTACT"]=> array(38) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22576" ["VALUE"]=> string(4) "1664" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1664" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(60) "Egor A. Kulagin " ["LINK_ELEMENT_VALUE"]=> bool(false) } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22619" ["VALUE"]=> array(2) { ["TEXT"]=> string(5923) "<p style="text-align: justify;">Высокая эффективность аллогенной трансплантации гемопоэтических стволовых клеток (алло- ТГСК) при широком спектре злокачественных и незлокачественных заболеваний системы крови ограничивается риском тяжелых осложнений и летального исхода без признаков рецидива или прогрессирования основного заболевания (безрецидивная летальность). Среди ключевых факторов безрецидивной летальности рассматривается коморбидность до момента алло-ТГСК. Целью настоящего исследования было охарактеризовать потенциальные предтрансплантационные факторы легочной коморбидности и интегральные показатели функции внешнего дыхания (ФВД) и оценить их прогностическое значение для исходов алло-ТГСК у взрослых пациентов.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">Исследование включало 355 больных, в том числе 149 (42%) в проспективной фазе исследования. Сформированная когорта включала пациентов с острыми лейкозами (60%), миелопролифератив-<br>ными заболеваниями (10%), миелодиспластическим синдромом (5%), лимфомами (17%) и тяжелой апластической анемией (8%). Медиана возраста на момент алло-ТГСК составила 33 года (18-66). Анализировались все потенциальные предтрансплантационные факторы легочной компрометации. Степень тяжести легочной коморбидности оценивалась на основании параметров ФВД – объема форсированного выдоха за первую секунду (ОФВ1) и диффузионной способности лёгких для оксида углерода (CO) (DLco) в соответствии с критериями индекса коморбидности Hematopoietic cell transplantation specific comorbidity index (HCT-CI). Прогностическое значение степени легочной коморбидности исследовано в отношении кумулятивной частоты перевода на искусственную вентиляцию легких (ИВЛ) и безрецидивной летальности.</p> <h3>Результаты</h3> <p style="text-align: justify;">Среди наиболее частых факторов легочной компрометации до алло-ТГСК идентифицированы курение (32%), анамнез хронической обструктивной болезни легких (ХОБЛ) и бронхиальной астмы (БА) (5%), инфекции легких (45%), потенциально пульмонотоксичная химиотерапия (79%), аутологичная ТГСК (8%), ингибиторы иммунных контрольных точек (5%), лучевая терапия на область средостения (6%) и др. Критериальное снижение ОФВ1 от должного имело место у 90 (25%) больных, включая 14%, 9% и 2% легкой, средней и тяжелой степени соответственно. Нарушение DLco было выявлено у 69% обследованных пациентов, включая 29%, 28% и 12% легкой, средней и тяжелой степени соответственно. Кумулятивная частота перевода на ИВЛ в течение 100 дней после алло-ТГСК составила 7,2%, 10,9%, 16,7% и 22,1% у пациентов с легочной коморбидностью 0, 1, 2, 3 степени соответственно. Степень легочной коморбидности была независимым фактором риска безрецидивной летальности (отношение рисков 1,39, ДИ 95%, 1.03-1.89, p=0.033) и ассоциировалась со снижением общей выживаемости. </p> <h3>Выводы</h3> <p style="text-align: justify;">Взрослые пациенты имеют широкий спектр факторов легочной коморбидности до алло-ТГСК. Легочная коморбидность по HCT-CI является фактором риска перевода на ИВЛ в течение первых 100 дней после алло-ТГСК и безрецидивной летальности. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Аллогенная трансплантация гемопоэтических стволовых клеток, взрослые, коморбидная патология легких, функция внешнего дыхания, клинический прогноз. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(5759) "Высокая эффективность аллогенной трансплантации гемопоэтических стволовых клеток (алло- ТГСК) при широком спектре злокачественных и незлокачественных заболеваний системы крови ограничивается риском тяжелых осложнений и летального исхода без признаков рецидива или прогрессирования основного заболевания (безрецидивная летальность). Среди ключевых факторов безрецидивной летальности рассматривается коморбидность до момента алло-ТГСК. Целью настоящего исследования было охарактеризовать потенциальные предтрансплантационные факторы легочной коморбидности и интегральные показатели функции внешнего дыхания (ФВД) и оценить их прогностическое значение для исходов алло-ТГСК у взрослых пациентов.
Пациенты и методы
Исследование включало 355 больных, в том числе 149 (42%) в проспективной фазе исследования. Сформированная когорта включала пациентов с острыми лейкозами (60%), миелопролифератив-
ными заболеваниями (10%), миелодиспластическим синдромом (5%), лимфомами (17%) и тяжелой апластической анемией (8%). Медиана возраста на момент алло-ТГСК составила 33 года (18-66). Анализировались все потенциальные предтрансплантационные факторы легочной компрометации. Степень тяжести легочной коморбидности оценивалась на основании параметров ФВД – объема форсированного выдоха за первую секунду (ОФВ1) и диффузионной способности лёгких для оксида углерода (CO) (DLco) в соответствии с критериями индекса коморбидности Hematopoietic cell transplantation specific comorbidity index (HCT-CI). Прогностическое значение степени легочной коморбидности исследовано в отношении кумулятивной частоты перевода на искусственную вентиляцию легких (ИВЛ) и безрецидивной летальности.
Результаты
Среди наиболее частых факторов легочной компрометации до алло-ТГСК идентифицированы курение (32%), анамнез хронической обструктивной болезни легких (ХОБЛ) и бронхиальной астмы (БА) (5%), инфекции легких (45%), потенциально пульмонотоксичная химиотерапия (79%), аутологичная ТГСК (8%), ингибиторы иммунных контрольных точек (5%), лучевая терапия на область средостения (6%) и др. Критериальное снижение ОФВ1 от должного имело место у 90 (25%) больных, включая 14%, 9% и 2% легкой, средней и тяжелой степени соответственно. Нарушение DLco было выявлено у 69% обследованных пациентов, включая 29%, 28% и 12% легкой, средней и тяжелой степени соответственно. Кумулятивная частота перевода на ИВЛ в течение 100 дней после алло-ТГСК составила 7,2%, 10,9%, 16,7% и 22,1% у пациентов с легочной коморбидностью 0, 1, 2, 3 степени соответственно. Степень легочной коморбидности была независимым фактором риска безрецидивной летальности (отношение рисков 1,39, ДИ 95%, 1.03-1.89, p=0.033) и ассоциировалась со снижением общей выживаемости.
Выводы
Взрослые пациенты имеют широкий спектр факторов легочной коморбидности до алло-ТГСК. Легочная коморбидность по HCT-CI является фактором риска перевода на ИВЛ в течение первых 100 дней после алло-ТГСК и безрецидивной летальности.
Ключевые слова
Аллогенная трансплантация гемопоэтических стволовых клеток, взрослые, коморбидная патология легких, функция внешнего дыхания, клинический прогноз.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(5759) "Высокая эффективность аллогенной трансплантации гемопоэтических стволовых клеток (алло- ТГСК) при широком спектре злокачественных и незлокачественных заболеваний системы крови ограничивается риском тяжелых осложнений и летального исхода без признаков рецидива или прогрессирования основного заболевания (безрецидивная летальность). Среди ключевых факторов безрецидивной летальности рассматривается коморбидность до момента алло-ТГСК. Целью настоящего исследования было охарактеризовать потенциальные предтрансплантационные факторы легочной коморбидности и интегральные показатели функции внешнего дыхания (ФВД) и оценить их прогностическое значение для исходов алло-ТГСК у взрослых пациентов.
Пациенты и методы
Исследование включало 355 больных, в том числе 149 (42%) в проспективной фазе исследования. Сформированная когорта включала пациентов с острыми лейкозами (60%), миелопролифератив-
ными заболеваниями (10%), миелодиспластическим синдромом (5%), лимфомами (17%) и тяжелой апластической анемией (8%). Медиана возраста на момент алло-ТГСК составила 33 года (18-66). Анализировались все потенциальные предтрансплантационные факторы легочной компрометации. Степень тяжести легочной коморбидности оценивалась на основании параметров ФВД – объема форсированного выдоха за первую секунду (ОФВ1) и диффузионной способности лёгких для оксида углерода (CO) (DLco) в соответствии с критериями индекса коморбидности Hematopoietic cell transplantation specific comorbidity index (HCT-CI). Прогностическое значение степени легочной коморбидности исследовано в отношении кумулятивной частоты перевода на искусственную вентиляцию легких (ИВЛ) и безрецидивной летальности.
Результаты
Среди наиболее частых факторов легочной компрометации до алло-ТГСК идентифицированы курение (32%), анамнез хронической обструктивной болезни легких (ХОБЛ) и бронхиальной астмы (БА) (5%), инфекции легких (45%), потенциально пульмонотоксичная химиотерапия (79%), аутологичная ТГСК (8%), ингибиторы иммунных контрольных точек (5%), лучевая терапия на область средостения (6%) и др. Критериальное снижение ОФВ1 от должного имело место у 90 (25%) больных, включая 14%, 9% и 2% легкой, средней и тяжелой степени соответственно. Нарушение DLco было выявлено у 69% обследованных пациентов, включая 29%, 28% и 12% легкой, средней и тяжелой степени соответственно. Кумулятивная частота перевода на ИВЛ в течение 100 дней после алло-ТГСК составила 7,2%, 10,9%, 16,7% и 22,1% у пациентов с легочной коморбидностью 0, 1, 2, 3 степени соответственно. Степень легочной коморбидности была независимым фактором риска безрецидивной летальности (отношение рисков 1,39, ДИ 95%, 1.03-1.89, p=0.033) и ассоциировалась со снижением общей выживаемости.
Выводы
Взрослые пациенты имеют широкий спектр факторов легочной коморбидности до алло-ТГСК. Легочная коморбидность по HCT-CI является фактором риска перевода на ИВЛ в течение первых 100 дней после алло-ТГСК и безрецидивной летальности.
Ключевые слова
Аллогенная трансплантация гемопоэтических стволовых клеток, взрослые, коморбидная патология легких, функция внешнего дыхания, клинический прогноз.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22618" ["VALUE"]=> array(2) { ["TEXT"]=> string(955) "<p><sup>1</sup> Кафедра госпитальной терапии с курсом аллергологии и иммунологии имени академика М.В. Черноруцкого, Санкт-Петербург, Россия<br> <sup>2</sup> НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Санкт-Петербург, Россия<br> <sup>3</sup> Отделение функциональной диагностики №2 Научно-клинического исследовательского центра, ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова» Минздрава России, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(895) "1 Кафедра госпитальной терапии с курсом аллергологии и иммунологии имени академика М.В. Черноруцкого, Санкт-Петербург, Россия
2 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Санкт-Петербург, Россия
3 Отделение функциональной диагностики №2 Научно-клинического исследовательского центра,
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова» Минздрава России, Санкт-Петербург, Россия
1 Кафедра госпитальной терапии с курсом аллергологии и иммунологии имени академика М.В. Черноруцкого, Санкт-Петербург, Россия
2 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Санкт-Петербург, Россия
3 Отделение функциональной диагностики №2 Научно-клинического исследовательского центра,
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова» Минздрава России, Санкт-Петербург, Россия
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is one of the most rapidly developing fields of medicine [1, 2, 3, 4]. Improvement of allo-HSCT technology allowed focusing on the new challenges. One of those issues is poor graft function (PGF). The incidence of PGF depends on many factors, e.g., diagnosis of the underlying disease, type of allo-HSCT, ABO-compatibility, viral reactivation, and varies between 5% and 20%, according to the most publications [5-8]. However, given the multifactorial nature of PGF, as well as frequent inability to perform etiological therapy, the treatment options are limited and poor standardized [9, 10].
Thrombopoietin is one of the main physiological regulators of platelet production and was initially considered as a linear growth factor for megakaryocytes. However, a number of studies have shown that Mpl expression is detected in 70% of hematopoietic stem cells. Thus, thrombopoietin alone or in combination with other cytokines stimulates the proliferation of early hematopoietic precursors [11, 12]. These data allowed the use of TPO-RA for the treatment of both idiopathic thrombocytopenic purpura and aplastic anemia with promising results [13-15]. The safety of using TPO-RA for malignant diseases has been questioned, however, it was analyzed in a large cohort study which showed TPO-RA therapy did not affect relapse of acute myeloid leukemia [16-18]. Recently, a number of studies have been conducted in order to expand the obtained experience to the setting of posttransplant cytopenias. TPO-RA has shown a positive effect in posttransplant thrombocytopenia, and there are some data suggesting functional improvement of other hematopoietic lineages.
Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias, including PGF, following allo-HSCT. In this report, we present data on the efficacy of TPO-RA in a large single-center adult cohort with PGF.
Patients and methods
We have performed clinical analysis of thirty-one adult patients at the median age of 22 (18-56) years old who received TPO-RA for treatment of cytopenia after allo-HSCT in the R. Gorbacheva Memorial Research Institute of Children Oncology, Hematology and Transplantation at the First St. Petersburg State I. Pavlov Medical University.
The inclusion criteria were as follows: 1) thrombocytopenia <20×109/l with or without cytopenias in other hematopoietic lines; 2) complete of stable mixed donor chimerism ≥90%; 3) no signs of relapse of underlying disease, or hematopoietic graft rejection. The spectrum of disorders in which allo-HSCT was indicated is shown in Table 1.
Table 1. Characteristics of the patients

Conditioning regimen considered to be myeloablative (MAC) (n=11.38%) at the dosage of oral busulfan ≥10 mg/kg. Dose of busulfan in reduced intensity regimes (RIC) was 10 mg/kg (n=18, 62%). Depending on the severity of cytopenia, three groups were selected by the following criteria: 1) mild PGF: ANC 1.0-1.5×109/l; platelets 50-100×109/l; hemoglobin >100 g/l; 2) moderate PGF: ANC 0.5-1.0×109/l; platelets 20-50×109/l; hemoglobin 70-100 g/l, 3) severe PGF: ANC <0.5×109/l; platelets <20×109/l; hemoglobin <70 g/l.
The response to TPO-RA therapy was assessed according to the hemogram dynamics: complete response: ANC ≥1.0×109/l, platelets ≥50×109/l, hemoglobin ≥80g/l; partial response: ANC ≥0.5×109/l, platelets ≥20×109/l, hemoglobin ≥70 g/l; no response: ANC <0.5×109/l, platelets <20×109/l, hemoglobin <70 g/l. Clinical outcomes of PGF were considered as: 1) any response to therapy, 3) recurrence of a malignant disease, 3) death.
Statistical analysis
Descriptive tables were analyzed for patient-related factors, donor and transplantation. Fisher's exact test and Pearson's Chi-square were used to compare binary data. The cumulative response rate was calculated taking into account competing risks (death, relapse). Overall survival (OS) was estimated using the Kaplan-Meier method over the time from administration of TPO agonists to the date of the last contact, or the date of death. The log-rank test was used to evaluate statistical differences between curves. Statistical analysis was performed using SPSS Statistics v.17 software, EZR free statistical environment, version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
This data analysis included 31 patients treated with TPO-RA for PGF after the first or second allo-HSCT. The myeloid engraftment was documented in all cases at the median of 21 (11-48) days. Thrombocytopenia was the indication for the therapy in 7 cases, 10 and 13 patients received TPO-RA for bi- and trilineage cytopenias, respectively. Characteristics of patients and transplants are shown in Table 1.
Malignant diseases prevailed in the diagnosis landscape: 87% versus 13%, with a significant proportion in the group fell on acute leukemia (55%) and myeloproliferative diseases (26%). The majority of patients (n=17, 55%) were transplanted from unrelated HLA-matched donors. However, the number of allo-HSCT from haploidentical donors was also significant in this cohort (n=9, 29%). Bone marrow (BM) and peripheral blood stem cells (PBSC) were used as a source of graft in 41% and 48% of cases, respectively, whereas a combination of BM and PBSC was applied in 11% cases.
Majority of the patients were transplanted after RIC: 65% versus 35% treated with MAC regimens. GVHD prophylaxis depended on the type of donor and source of the graft. GVHD prophylaxis for all cases of haploidentical HSCTs except of one (n=8, 26%) consisted of posttransplant cyclophosphamide (ptCy) in combination with cyclosporine A, or tacrolimus and/or other immunosuppressants (mycophenolate mofetil or sirolimus). For HLA-matched HSCTs, ptCy, ATG in combination with CsA and methotrexate, and a combination of tacrolimus and mycophenolate mofetil was used in 2 cases, 1 case, and 1 case, respectively. Of the 17 unrelated HLA-matched HSCTs, ATG and ptCy were used in 7 and 10 cases, respectively. Thus, GVHD prophylaxis with ptCy was predominant in the analyzed group (61%, n=19). Allo-HSCT with a major AB0-incompatibility took place in 25% (n=7) cases. Most patients (81%, n=25) suffered viral reactivation (mainly cytomegalovirus) and received ganciclovir or valganciclovir at the doses of 5-10 mg/kg/day, or 450-900 mg/day, respectively. A total of 61% (n=19) of the patients had signs of acute infection at the time of starting TPO-RA therapy. The proportion of cases of acute GVHD grade III-IV was also significant (42%).
The median time from allo-HSCT to PGF was 54 days (18 to 664), with prevalence of early PGF (n=20, 65%), compared to late PGF (n=11, 35%). Severe PGF was the most frequent indication for therapy (n=24, 77%) vs posttransplant thrombocytopenia (n=7, 23%).
The median duration of PGF was 59 days (5-426). The median time from the diagnosis of PGF to the start of therapy with TPO-RA was 15 days (0-119). The median duration of the treatment was 3 (1-48) weeks. The median cumulative doses of romiplostim and eltrombopag were 15 (5-70) mg and 2100 (700-50400) mg, respectively.
TPO-RA drugs were well tolerated, with no detectable toxicity of grade 3-4. One case of hepatotoxicity grade 2 was documented with eltrombopag but didn’t require withdrawal of the drug.
TPO-RA were used in combination with other therapies in 26% of cases: rituximab in 5 cases, rituximab and infusion of donor lymphocytes in 3 cases, and a booster dose of CD34+ cells from the same donor was applied in one case.
A total of 16 (52 %) patients developed response to the TPO-RA. Complete response was documented in 4 cases (13 %), while 12 patients (39 %) showed partial response. The median of increase in ANC in responders was 1.7×109/l (0.1-5.6), in platelet count – 20×109/l (2-205). The median cumulative dose of romiplostim in responders was 30 mg/kg (3.5-73), for eltrombopag it was 4900 mg (2100-50400). The median time of response for romiplostim and eltrombopag was 63 days (5-181) and 103 days (52-426), respectively. Combination therapy had no benefits in the response rate compared to monotherapy with TPO-RA. Overall response was similar for both medications. Our analysis showed no influence of infections (including viral), or acute GVHD grade 3-4 on the cumulative response to the TPO-RA therapy.

Figure 1. One-year overall survival (OS) curves for responders to TPO-RA drugs, and non-responding patients. Abscissa, time from start of the therapy, days; ordinate OS rates, % of total
Twelve of 16 responders were alive: 7 patients with time of response under median values and 5 patients with time to response exceeding median levels.
A total of 18 patients died. Infectious complications were the main cause of death in these cases (n=11), wherein 8 cases were classified as non-responders, and 3 patients showed longer time to response which exceeded median values. The disease relapse caused death in 4 cases, while aGVHD was associated with lethal outcome in 3 cases.
One-year OS from the start of therapy with TPO-RA was 60% (95% CI, 40-76). It was significantly different for responders and non-responders: 78% (95% CI, 47-93) versus 33% (95% CI, 12-56) (p=0.004), as seen from Fig. 1.
Discussion
Allogeneic hematopoietic stem cell transplantation is an effective method for treatment of a wide range of malignant and non-malignant diseases of the blood system. With improving the HSCT technology, most transplanted patients achieve engraftment, but the so-called “poor graft function”, i.e., posttransplant cytopenia of various origin with preservation of donor chimerism still remains a challenge. Poor graft function is one of factors significantly worsening the outcome of allo-HSCT [5].
The impairment of hematopoietic stem cell (HSC) compartments after HSCT has been demonstrated by reduced numbers of hematopoietic progenitors under the in vitro culture conditions [19]. The graft functioning might be influenced by the underlying disease, donor and recipient HLA compatibility, the dose of transplanted CD34+ cells, as well as by accompanying complications (GVHD, infections, including viral activation). However, most of the cases remain idiopathic [20, 21, 22]. Most likely, a combination of these factors creates an immune-active environment that hampers the normal development and functioning of transplanted HSCs [23, 24, 25]. Moreover, several post-HSCT conditions (e.g., myelotoxic drugs, inflammatory events, and infections) provide well-established mechanisms impairing hematopoiesis.
TPO-RA drugs, in the context of PGF therapy, may present a promising option, especially, concerning eltrombopag. There are several mechanisms by which eltrombopag may provide effect in the bone marrow failure syndromes. Eltrombopag works as a trigger for HSCs and promotes active proliferation of HSCs after HSCT. Also eltrombopag has an immunomodulatory effect on the T-regulatory cell function [26]. Furthermore, abolition of inhibitory effect produced by interferon-γ upon HSCs may be another potential mechanism of eltrombopag action which has been recently explained. Eltrombopag, by its binding directly to c-MPL, activates its intracellular signal transduction pathway, irrespectively of interferon-γ presence [27].
Since it is impossible to separate the only etiological factor, the choice of a single approach to the therapy of PGF is complicated. However, given the data on the efficacy of TPO agonists in various bone marrow failure syndromes and other diseases associated with cytopenia, and the safety of their use in malignant diseases, as well as its ability to overcome the immune mechanisms of suppressing hematopoiesis, TPO-RA seem to be good candidates for management of PGF. Recently, the several groups published the experience of TPO-RA administration in post-transplant setting [28, 29, 30]. Nevertheless, the precise analysis of efficiency of this therapy is complicated, due to small number of patients and different inclusion criteria in these studies.
We analyzed the results of the use of TPO-RA in our BMT center. The special feature of our cohort was the predominance of patients with severe trilineage cytopenia, as well as high proportion of patients with severe acute GVHD. Our experience showed the safety of TPO-RA: there was only one case of hepatotoxicity of grade 1, which did not require discontinuation of the drug. Neither the drug used, nor the duration of therapy, nor the cumulative dose of each agent didn’t influence overall response in our study. However, there are reports that the cumulative dose for romiplostim plays a role for the overall response to therapy [31].
In our study, there was no statistically significant correlations between the overall response rates to TPO-RA, and clinical complications associated with PGF (sepsis, aGVHD, viral infections), thus being in accordance with results from other centers. However, there is some evidence that a better response could be obtained in the absence of active GVHD [32].
Facing a problem of prolonged cytopenia in the posttransplant period, only booster CD34-cell infusions are considered more or less standardized therapy. TPO-RA used as monotherapy, or in combination with other methods, seem to be quite effective for PGF after allo-HSCT, regardless of its etiology.
Conclusion
TPO-RA showed promising efficacy and low toxicity in adult patients with PGF after allo-HSCT. Considering multifactorial origin of PGF, TPO-RA might be a reasonable approach that could be applied early and irrespectively of PGF cause. However, the optimal dose and duration of the administration, as well as the criteria for discontinuation of these drugs remain uncertain. Multicenter prospective studies are needed to resolve these problems.
Conflict of interest
The authors report no conflicts of interest.
References
- Duarte RF, Labopin M, Bader Р, Basak GW, Bonini Ch, Chabannon Ch, Corbacioglu S, Dreger P, Dufour C, Andrew R. Gennery AR, Kuball J, Lankester AC, Lanza F, Montoto S, Nagler A, Peffault de Latour R, Snowden JA, Styczynski J, Yakoub-Agha I, Kröger N, Mohty M,for the European Society for Blood and Marrow Transplantation (EBMT). Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant. 2019 https://doi.org/10.1038/s41409-019-0516-2.
- Majhail NS, Farnia SH, Carpenter PA, Champlin RE, Crawford S, Marks DI, Omel JL, Orchard PJ, Palmer J, Saber W, Savani BN, Veys PA, Bredeson ChN, Giralt SA, LeMaistre ChF. Indications for autologous and allogeneic hematopoietic cell transplantation: Guidelines from the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2015; 21(11): 1863–1869.
- Savchenko VG, Liubimova LS, Parovichnikova EN, Mendeleeva LP, Mamotiuk KS, Demidova IA, Gribanova EO, Gal'tseva IV, Pokrovskaia OS, Kuz'mina LA, Zhelnova EI, Kliasova GA, Glasko EN, Kaplanskaia IB, Poreshina LP, et al. Transplantations of allogenic and autologous hemopoietic stem cells in acute leukemia (results of 20-year experience). Terapevticheskiy arkhiv. 2007;79 (7):30-35. (In Russian).
- Afanasyev BV, Zubarovskaya LS, Moiseev IS. Allogeneic hematopoietic stem cell transplantation in children: now, problems and prospects. Russian Journal of Children Hematology and Oncology. 2015;2(2):28-42. (In Russian).
- Rudakova TA, Kulagin AD, Klimova OU, et al. Severe "poor graft function" after allogeneic hematopoietic stem cell transplantation in adult patients: incidence, risk Factors, and outcomes. Clinical Oncohematology. 2019;12(3):309-318 (In Russian).
- Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, Ringden O. Graft failure in the modern era of allogeneic hematopoietic SCT. Bone Marrow Transplant. 2013;48: 537-543.
- Alchalby H, Yunus DR, Zabelina T, Ayuk F, Kröger N. Incidence and risk factors of poor graft function after allogeneic stem cell transplantation for myelofibrosis. Bone Marrow Transplant. 2016;51(9):1223-1227.
- Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, Pozzi S, Varaldo R, Lamparelli T, Bregante S, Van Lint MT, diGrazia C, Bacigalupo A. CD34+ selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20:1440–1443.
- Gale RP. Early and late graft-failure after transplants. Bone Marrow Transplant. 2016;51:182-183.
- Valcárcel D, Sureda A. Graft failure. The EBMT Handbook (2019). doi.org/10.1007/978-3-030-02278-5_41.
- Solar GP, Kerr WG, Zeigler FC, Hess D, Donahue Ch, de Sauvage FJ, Eaton DL. Role of c-mpl in Early Hematopoiesis. Blood. 1998; 92(1):4-10.
- Ninos JM, Jefferies LC, Cogle ChR, Kerr WG. The thrombopoietin receptor, c-Mpl, is a selective surface marker for human hematopoietic stem cells. J Transl Med. 2006;4:9. doi: 10.1186/1479-5876-4-9.
- Bussel JB, Cheng G, Saleh MN, Psaila B, Kovaleva L, Meddeb B, Kloczko J, Hassani H, Mayer B, Stone NL, Arning M, Provan D, Jenkins JM. Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura. N Engl J Med. 2007; 29;357(22):2237-2247.
- Cheng G, Saleh MN, Marcher C, Vasey S, Mayer B, Aivado M, Arning M, Stone NL, Bussel JB. Eltrombopag for management of chronic immune thrombocytopenia (RAISE): a 6-month, randomised, phase 3 study. Lancet. 2011; 29; 377(9763):393-402.
- Winkler T, Fan X, Cooper J, Desmond R, Young DJ, Townsley DM. Eltrombopag for refractory severe aplastic anemia: dosing, duration, long term outcomes and clonal evolution. Blood, 2019.
- Ecsedi M, Lengline É, Knol-Bout C, Bosman P, Eikema DJ, Afanasyev B, Maschan A, Dreger P, Halkes CJM, Drexler B, Cortelezzi A, Drénou B, Patriarca A, Bruno B, Onofrillo D, Lanino E, Pulanic D, Serventi-Seiwerth R, Garnier A, Ljungman P, Bonifazi F, Giammarco S, Tournilhac O, Pioltelli P, Rovó A, Risitano AM, de Latour RP, Dufour C, Passweg J. Use of eltrombopag in aplastic anemia in Europe. Ann Hematol. 2019; 98(6):1341-1350.
- Mittelman M, Platzbecker U, Afanasyev B, Grosicki S, Wong RSM, Anagnostopoulos A, Brenner B, Denzlinger C, Rossi G, Nagler A, Garcia-Delgado R, Portella MSO, Zhu Z, Selleslag D. Eltrombopag for advanced myelodysplastic syndromes or acute myeloid leukaemia and severe thrombocytopenia (ASPIRE): a randomised, placebo-controlled, phase 2 trial. Lancet Haematol. 2018;5(1):e34-e43. DOI: 10.1016/S2352-3026(17)30228-4.
- Oliva EN, Alati C, Santini V, Poloni A, Molteni A, Niscola P, Salvi F, Sanpaolo G, Balleari E, Germing U, Fenaux P, Stamatoullas A, Palumbo GA, Salutari P, Impera S et al. Eltrombopag versus placebo for low-risk myelodysplastic syndromes with thrombocytopenia (EQoL-MDS): phase 1 results of a single-blind, randomised, controlled, phase 2 superiority trial. Lancet Haematol. 2017;4:e127-e136. DOI: 10.1016/S2352-3026(17)30012-1.
- Kong Y, Wang YT, Hu Y, Han W, Chang YJ, Zhang XH, Jiang ZF, Huang XJ. The bone marrow microenvironment is similarly impaired in allogeneic hematopoietic stem cell transplantation patients with early and late poor graft function. Bone Marrow Transplant. 2016;51:249-255.
- Rondón G, Saliba RM, Khouri I, Giralt S, Chan K, Jabbour E, McMannis J, Champlin R, Shpall E. Long-term follow up of patients who experienced graft failure post allogeneic progenitor cell transplantation. Results of a single institution analysis. Biol Blood Marrow Transplant. 2008; 14(8): 859–866.
- Kröger N, Holler E, Kobbe G, Bornhäuser M, Schwerdtfeger R, Baurmann H, Nagler A, Bethge W, Stelljes M, Uharek L, Wandt H, Burchert A, Corradini P, Schubert J, Kaufmann M, Dreger P, Wulf GG, Einsele H, Zabelina T, Kvasnicka HM, Thiele J, Brand R, Zander AR, Niederwieser D, de Witte TM. Allogeneic stem cell transplantation after reduced-intensity conditioning in patients with myelofibrosis: a prospective, multicenter study of the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation Blood. 2009;114(26):5264-5270.
- Dominietto A, Raiola AM, van Lint MT, Lamparelli T, Gualandi F, Berisso G, Bregante S, Frassoni F, Casarino L, Verdiani S and Bacigalupo A. Factors influencing haematological recovery after allogeneic haemopoietic stem cell transplants: graft-versus-host disease, donor type, cytomegalovirus infections and cell dose. Br J Haematol. 2001;112:219-227.
- Yu J-M, Emmons RV, Hanazono Y, Sellers S, Young NS, Dunbar CE. Expression of interferon-γ by stromal cells inhibits murine long-term repopulating hematopoietic stem cell activity. Exp Hematol. 1999;27(5):895-903.
- Kong Y, Wang Yu-Tong , Cao Xie-Na , Song Yang , Chen Yu-Hong , Sun Yu-Qian , Wang Yu , Zhang Xiao-Hui , Xu Lan-Ping, Huang Xiao-Jun. Aberrant T cell responses in the bone marrow microenvironment of patients with poor graft function after allogeneic hematopoietic stem cell transplantation. J Transl Med. 2017;15:57. doi: 10.1186/s12967-017-1159-y.
- Rudakova TA, Eismont YuA, Moiseev IS, Zubarovskaya LS, Kulagin AD, Afanasyev BV. Role of polyomavirus in emerging secondary hypofunction of marrow graft following allogeneic bone marrow transplantation in adults. Cellular Therapy and Transplantation. 2016;5(3):79–82. DOI: 10.18620/ctt-1866-8836-2016-5-3-79-82.
- Bao W, Bussel JB, Heck S, He W, Karpoff M, Boulad N, Yazdanbakhsh K. Improved regulatory T-cell activity in patients with chronic immune thrombocytopenia treated with thrombopoietic agents. Blood. 2010;116:4639–4645.
- Alvarado LJ, Andreoni A, Huntsman HD, Cheng H, Knutson JR, Larochelle A. Heterodimerization of TPO and IFNγ impairs human hematopoietic stem/progenitor cell signaling and survival in chronic inflammation. Blood. 2017;130:4.
- Lisukov IA, Uspenskaya OS, Kulagin AD, Bondarenko SN, Rudakova TA, Slesarchuk O.A., Afanasyev BV. Romiplostim in thrombocytopenia treatment after allogeneic bone marrow transplantation. Oncohematology. 2012;7(1):29–34. (In Russian).
- Marotta S, Marano L, Ricci P, Cacace F, Frieri C, Simeone L, Trastulli F, Vitiello S, Cardano F, Pane F, Risitano AM. Eltrombopag for post-transplant cytopenias due to poor graft function. Bone Marrow Transplant. 2019;54(8):1346-1353.
- Tang C, Chen F, Kong D, Ma Q, Dai H, Yin J, Li Zh, Chen Ji, Zhu X, Mao X, Wu D, Tang X. Successful treatment of secondary poor graft function post allogeneic hematopoietic stem cell transplantation with Eltrombopag. J Hematol Oncol. 2018 ;11:103 https://doi.org/10.1186/s13045-018-0649-6.
- Liga M. Romiplostim for the treatment of thrombocytopenia after allogeneic stem cell transplantation. The 45th Annual Meeting of EBMT (Physicians, Poster Session). Bone Marrow Transplantation. 2019;54:144–619, P143.
- Aguirre L. Eltrombopag (EPAG) induces a high percentage of responses in patients with post allo-HSCT poor graft function (PGF) and no active GVHD. The 45th Annual Meeting of EBMT (Physicians, Poster Session). Bone Marrow Transplantation. 2019;54:144–619, P133.
Introduction
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is one of the most rapidly developing fields of medicine [1, 2, 3, 4]. Improvement of allo-HSCT technology allowed focusing on the new challenges. One of those issues is poor graft function (PGF). The incidence of PGF depends on many factors, e.g., diagnosis of the underlying disease, type of allo-HSCT, ABO-compatibility, viral reactivation, and varies between 5% and 20%, according to the most publications [5-8]. However, given the multifactorial nature of PGF, as well as frequent inability to perform etiological therapy, the treatment options are limited and poor standardized [9, 10].
Thrombopoietin is one of the main physiological regulators of platelet production and was initially considered as a linear growth factor for megakaryocytes. However, a number of studies have shown that Mpl expression is detected in 70% of hematopoietic stem cells. Thus, thrombopoietin alone or in combination with other cytokines stimulates the proliferation of early hematopoietic precursors [11, 12]. These data allowed the use of TPO-RA for the treatment of both idiopathic thrombocytopenic purpura and aplastic anemia with promising results [13-15]. The safety of using TPO-RA for malignant diseases has been questioned, however, it was analyzed in a large cohort study which showed TPO-RA therapy did not affect relapse of acute myeloid leukemia [16-18]. Recently, a number of studies have been conducted in order to expand the obtained experience to the setting of posttransplant cytopenias. TPO-RA has shown a positive effect in posttransplant thrombocytopenia, and there are some data suggesting functional improvement of other hematopoietic lineages.
Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias, including PGF, following allo-HSCT. In this report, we present data on the efficacy of TPO-RA in a large single-center adult cohort with PGF.
Patients and methods
We have performed clinical analysis of thirty-one adult patients at the median age of 22 (18-56) years old who received TPO-RA for treatment of cytopenia after allo-HSCT in the R. Gorbacheva Memorial Research Institute of Children Oncology, Hematology and Transplantation at the First St. Petersburg State I. Pavlov Medical University.
The inclusion criteria were as follows: 1) thrombocytopenia <20×109/l with or without cytopenias in other hematopoietic lines; 2) complete of stable mixed donor chimerism ≥90%; 3) no signs of relapse of underlying disease, or hematopoietic graft rejection. The spectrum of disorders in which allo-HSCT was indicated is shown in Table 1.
Table 1. Characteristics of the patients

Conditioning regimen considered to be myeloablative (MAC) (n=11.38%) at the dosage of oral busulfan ≥10 mg/kg. Dose of busulfan in reduced intensity regimes (RIC) was 10 mg/kg (n=18, 62%). Depending on the severity of cytopenia, three groups were selected by the following criteria: 1) mild PGF: ANC 1.0-1.5×109/l; platelets 50-100×109/l; hemoglobin >100 g/l; 2) moderate PGF: ANC 0.5-1.0×109/l; platelets 20-50×109/l; hemoglobin 70-100 g/l, 3) severe PGF: ANC <0.5×109/l; platelets <20×109/l; hemoglobin <70 g/l.
The response to TPO-RA therapy was assessed according to the hemogram dynamics: complete response: ANC ≥1.0×109/l, platelets ≥50×109/l, hemoglobin ≥80g/l; partial response: ANC ≥0.5×109/l, platelets ≥20×109/l, hemoglobin ≥70 g/l; no response: ANC <0.5×109/l, platelets <20×109/l, hemoglobin <70 g/l. Clinical outcomes of PGF were considered as: 1) any response to therapy, 3) recurrence of a malignant disease, 3) death.
Statistical analysis
Descriptive tables were analyzed for patient-related factors, donor and transplantation. Fisher's exact test and Pearson's Chi-square were used to compare binary data. The cumulative response rate was calculated taking into account competing risks (death, relapse). Overall survival (OS) was estimated using the Kaplan-Meier method over the time from administration of TPO agonists to the date of the last contact, or the date of death. The log-rank test was used to evaluate statistical differences between curves. Statistical analysis was performed using SPSS Statistics v.17 software, EZR free statistical environment, version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
This data analysis included 31 patients treated with TPO-RA for PGF after the first or second allo-HSCT. The myeloid engraftment was documented in all cases at the median of 21 (11-48) days. Thrombocytopenia was the indication for the therapy in 7 cases, 10 and 13 patients received TPO-RA for bi- and trilineage cytopenias, respectively. Characteristics of patients and transplants are shown in Table 1.
Malignant diseases prevailed in the diagnosis landscape: 87% versus 13%, with a significant proportion in the group fell on acute leukemia (55%) and myeloproliferative diseases (26%). The majority of patients (n=17, 55%) were transplanted from unrelated HLA-matched donors. However, the number of allo-HSCT from haploidentical donors was also significant in this cohort (n=9, 29%). Bone marrow (BM) and peripheral blood stem cells (PBSC) were used as a source of graft in 41% and 48% of cases, respectively, whereas a combination of BM and PBSC was applied in 11% cases.
Majority of the patients were transplanted after RIC: 65% versus 35% treated with MAC regimens. GVHD prophylaxis depended on the type of donor and source of the graft. GVHD prophylaxis for all cases of haploidentical HSCTs except of one (n=8, 26%) consisted of posttransplant cyclophosphamide (ptCy) in combination with cyclosporine A, or tacrolimus and/or other immunosuppressants (mycophenolate mofetil or sirolimus). For HLA-matched HSCTs, ptCy, ATG in combination with CsA and methotrexate, and a combination of tacrolimus and mycophenolate mofetil was used in 2 cases, 1 case, and 1 case, respectively. Of the 17 unrelated HLA-matched HSCTs, ATG and ptCy were used in 7 and 10 cases, respectively. Thus, GVHD prophylaxis with ptCy was predominant in the analyzed group (61%, n=19). Allo-HSCT with a major AB0-incompatibility took place in 25% (n=7) cases. Most patients (81%, n=25) suffered viral reactivation (mainly cytomegalovirus) and received ganciclovir or valganciclovir at the doses of 5-10 mg/kg/day, or 450-900 mg/day, respectively. A total of 61% (n=19) of the patients had signs of acute infection at the time of starting TPO-RA therapy. The proportion of cases of acute GVHD grade III-IV was also significant (42%).
The median time from allo-HSCT to PGF was 54 days (18 to 664), with prevalence of early PGF (n=20, 65%), compared to late PGF (n=11, 35%). Severe PGF was the most frequent indication for therapy (n=24, 77%) vs posttransplant thrombocytopenia (n=7, 23%).
The median duration of PGF was 59 days (5-426). The median time from the diagnosis of PGF to the start of therapy with TPO-RA was 15 days (0-119). The median duration of the treatment was 3 (1-48) weeks. The median cumulative doses of romiplostim and eltrombopag were 15 (5-70) mg and 2100 (700-50400) mg, respectively.
TPO-RA drugs were well tolerated, with no detectable toxicity of grade 3-4. One case of hepatotoxicity grade 2 was documented with eltrombopag but didn’t require withdrawal of the drug.
TPO-RA were used in combination with other therapies in 26% of cases: rituximab in 5 cases, rituximab and infusion of donor lymphocytes in 3 cases, and a booster dose of CD34+ cells from the same donor was applied in one case.
A total of 16 (52 %) patients developed response to the TPO-RA. Complete response was documented in 4 cases (13 %), while 12 patients (39 %) showed partial response. The median of increase in ANC in responders was 1.7×109/l (0.1-5.6), in platelet count – 20×109/l (2-205). The median cumulative dose of romiplostim in responders was 30 mg/kg (3.5-73), for eltrombopag it was 4900 mg (2100-50400). The median time of response for romiplostim and eltrombopag was 63 days (5-181) and 103 days (52-426), respectively. Combination therapy had no benefits in the response rate compared to monotherapy with TPO-RA. Overall response was similar for both medications. Our analysis showed no influence of infections (including viral), or acute GVHD grade 3-4 on the cumulative response to the TPO-RA therapy.

Figure 1. One-year overall survival (OS) curves for responders to TPO-RA drugs, and non-responding patients. Abscissa, time from start of the therapy, days; ordinate OS rates, % of total
Twelve of 16 responders were alive: 7 patients with time of response under median values and 5 patients with time to response exceeding median levels.
A total of 18 patients died. Infectious complications were the main cause of death in these cases (n=11), wherein 8 cases were classified as non-responders, and 3 patients showed longer time to response which exceeded median values. The disease relapse caused death in 4 cases, while aGVHD was associated with lethal outcome in 3 cases.
One-year OS from the start of therapy with TPO-RA was 60% (95% CI, 40-76). It was significantly different for responders and non-responders: 78% (95% CI, 47-93) versus 33% (95% CI, 12-56) (p=0.004), as seen from Fig. 1.
Discussion
Allogeneic hematopoietic stem cell transplantation is an effective method for treatment of a wide range of malignant and non-malignant diseases of the blood system. With improving the HSCT technology, most transplanted patients achieve engraftment, but the so-called “poor graft function”, i.e., posttransplant cytopenia of various origin with preservation of donor chimerism still remains a challenge. Poor graft function is one of factors significantly worsening the outcome of allo-HSCT [5].
The impairment of hematopoietic stem cell (HSC) compartments after HSCT has been demonstrated by reduced numbers of hematopoietic progenitors under the in vitro culture conditions [19]. The graft functioning might be influenced by the underlying disease, donor and recipient HLA compatibility, the dose of transplanted CD34+ cells, as well as by accompanying complications (GVHD, infections, including viral activation). However, most of the cases remain idiopathic [20, 21, 22]. Most likely, a combination of these factors creates an immune-active environment that hampers the normal development and functioning of transplanted HSCs [23, 24, 25]. Moreover, several post-HSCT conditions (e.g., myelotoxic drugs, inflammatory events, and infections) provide well-established mechanisms impairing hematopoiesis.
TPO-RA drugs, in the context of PGF therapy, may present a promising option, especially, concerning eltrombopag. There are several mechanisms by which eltrombopag may provide effect in the bone marrow failure syndromes. Eltrombopag works as a trigger for HSCs and promotes active proliferation of HSCs after HSCT. Also eltrombopag has an immunomodulatory effect on the T-regulatory cell function [26]. Furthermore, abolition of inhibitory effect produced by interferon-γ upon HSCs may be another potential mechanism of eltrombopag action which has been recently explained. Eltrombopag, by its binding directly to c-MPL, activates its intracellular signal transduction pathway, irrespectively of interferon-γ presence [27].
Since it is impossible to separate the only etiological factor, the choice of a single approach to the therapy of PGF is complicated. However, given the data on the efficacy of TPO agonists in various bone marrow failure syndromes and other diseases associated with cytopenia, and the safety of their use in malignant diseases, as well as its ability to overcome the immune mechanisms of suppressing hematopoiesis, TPO-RA seem to be good candidates for management of PGF. Recently, the several groups published the experience of TPO-RA administration in post-transplant setting [28, 29, 30]. Nevertheless, the precise analysis of efficiency of this therapy is complicated, due to small number of patients and different inclusion criteria in these studies.
We analyzed the results of the use of TPO-RA in our BMT center. The special feature of our cohort was the predominance of patients with severe trilineage cytopenia, as well as high proportion of patients with severe acute GVHD. Our experience showed the safety of TPO-RA: there was only one case of hepatotoxicity of grade 1, which did not require discontinuation of the drug. Neither the drug used, nor the duration of therapy, nor the cumulative dose of each agent didn’t influence overall response in our study. However, there are reports that the cumulative dose for romiplostim plays a role for the overall response to therapy [31].
In our study, there was no statistically significant correlations between the overall response rates to TPO-RA, and clinical complications associated with PGF (sepsis, aGVHD, viral infections), thus being in accordance with results from other centers. However, there is some evidence that a better response could be obtained in the absence of active GVHD [32].
Facing a problem of prolonged cytopenia in the posttransplant period, only booster CD34-cell infusions are considered more or less standardized therapy. TPO-RA used as monotherapy, or in combination with other methods, seem to be quite effective for PGF after allo-HSCT, regardless of its etiology.
Conclusion
TPO-RA showed promising efficacy and low toxicity in adult patients with PGF after allo-HSCT. Considering multifactorial origin of PGF, TPO-RA might be a reasonable approach that could be applied early and irrespectively of PGF cause. However, the optimal dose and duration of the administration, as well as the criteria for discontinuation of these drugs remain uncertain. Multicenter prospective studies are needed to resolve these problems.
Conflict of interest
The authors report no conflicts of interest.
References
- Duarte RF, Labopin M, Bader Р, Basak GW, Bonini Ch, Chabannon Ch, Corbacioglu S, Dreger P, Dufour C, Andrew R. Gennery AR, Kuball J, Lankester AC, Lanza F, Montoto S, Nagler A, Peffault de Latour R, Snowden JA, Styczynski J, Yakoub-Agha I, Kröger N, Mohty M,for the European Society for Blood and Marrow Transplantation (EBMT). Indications for haematopoietic stem cell transplantation for haematological diseases, solid tumours and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant. 2019 https://doi.org/10.1038/s41409-019-0516-2.
- Majhail NS, Farnia SH, Carpenter PA, Champlin RE, Crawford S, Marks DI, Omel JL, Orchard PJ, Palmer J, Saber W, Savani BN, Veys PA, Bredeson ChN, Giralt SA, LeMaistre ChF. Indications for autologous and allogeneic hematopoietic cell transplantation: Guidelines from the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2015; 21(11): 1863–1869.
- Savchenko VG, Liubimova LS, Parovichnikova EN, Mendeleeva LP, Mamotiuk KS, Demidova IA, Gribanova EO, Gal'tseva IV, Pokrovskaia OS, Kuz'mina LA, Zhelnova EI, Kliasova GA, Glasko EN, Kaplanskaia IB, Poreshina LP, et al. Transplantations of allogenic and autologous hemopoietic stem cells in acute leukemia (results of 20-year experience). Terapevticheskiy arkhiv. 2007;79 (7):30-35. (In Russian).
- Afanasyev BV, Zubarovskaya LS, Moiseev IS. Allogeneic hematopoietic stem cell transplantation in children: now, problems and prospects. Russian Journal of Children Hematology and Oncology. 2015;2(2):28-42. (In Russian).
- Rudakova TA, Kulagin AD, Klimova OU, et al. Severe "poor graft function" after allogeneic hematopoietic stem cell transplantation in adult patients: incidence, risk Factors, and outcomes. Clinical Oncohematology. 2019;12(3):309-318 (In Russian).
- Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, Ringden O. Graft failure in the modern era of allogeneic hematopoietic SCT. Bone Marrow Transplant. 2013;48: 537-543.
- Alchalby H, Yunus DR, Zabelina T, Ayuk F, Kröger N. Incidence and risk factors of poor graft function after allogeneic stem cell transplantation for myelofibrosis. Bone Marrow Transplant. 2016;51(9):1223-1227.
- Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, Pozzi S, Varaldo R, Lamparelli T, Bregante S, Van Lint MT, diGrazia C, Bacigalupo A. CD34+ selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20:1440–1443.
- Gale RP. Early and late graft-failure after transplants. Bone Marrow Transplant. 2016;51:182-183.
- Valcárcel D, Sureda A. Graft failure. The EBMT Handbook (2019). doi.org/10.1007/978-3-030-02278-5_41.
- Solar GP, Kerr WG, Zeigler FC, Hess D, Donahue Ch, de Sauvage FJ, Eaton DL. Role of c-mpl in Early Hematopoiesis. Blood. 1998; 92(1):4-10.
- Ninos JM, Jefferies LC, Cogle ChR, Kerr WG. The thrombopoietin receptor, c-Mpl, is a selective surface marker for human hematopoietic stem cells. J Transl Med. 2006;4:9. doi: 10.1186/1479-5876-4-9.
- Bussel JB, Cheng G, Saleh MN, Psaila B, Kovaleva L, Meddeb B, Kloczko J, Hassani H, Mayer B, Stone NL, Arning M, Provan D, Jenkins JM. Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura. N Engl J Med. 2007; 29;357(22):2237-2247.
- Cheng G, Saleh MN, Marcher C, Vasey S, Mayer B, Aivado M, Arning M, Stone NL, Bussel JB. Eltrombopag for management of chronic immune thrombocytopenia (RAISE): a 6-month, randomised, phase 3 study. Lancet. 2011; 29; 377(9763):393-402.
- Winkler T, Fan X, Cooper J, Desmond R, Young DJ, Townsley DM. Eltrombopag for refractory severe aplastic anemia: dosing, duration, long term outcomes and clonal evolution. Blood, 2019.
- Ecsedi M, Lengline É, Knol-Bout C, Bosman P, Eikema DJ, Afanasyev B, Maschan A, Dreger P, Halkes CJM, Drexler B, Cortelezzi A, Drénou B, Patriarca A, Bruno B, Onofrillo D, Lanino E, Pulanic D, Serventi-Seiwerth R, Garnier A, Ljungman P, Bonifazi F, Giammarco S, Tournilhac O, Pioltelli P, Rovó A, Risitano AM, de Latour RP, Dufour C, Passweg J. Use of eltrombopag in aplastic anemia in Europe. Ann Hematol. 2019; 98(6):1341-1350.
- Mittelman M, Platzbecker U, Afanasyev B, Grosicki S, Wong RSM, Anagnostopoulos A, Brenner B, Denzlinger C, Rossi G, Nagler A, Garcia-Delgado R, Portella MSO, Zhu Z, Selleslag D. Eltrombopag for advanced myelodysplastic syndromes or acute myeloid leukaemia and severe thrombocytopenia (ASPIRE): a randomised, placebo-controlled, phase 2 trial. Lancet Haematol. 2018;5(1):e34-e43. DOI: 10.1016/S2352-3026(17)30228-4.
- Oliva EN, Alati C, Santini V, Poloni A, Molteni A, Niscola P, Salvi F, Sanpaolo G, Balleari E, Germing U, Fenaux P, Stamatoullas A, Palumbo GA, Salutari P, Impera S et al. Eltrombopag versus placebo for low-risk myelodysplastic syndromes with thrombocytopenia (EQoL-MDS): phase 1 results of a single-blind, randomised, controlled, phase 2 superiority trial. Lancet Haematol. 2017;4:e127-e136. DOI: 10.1016/S2352-3026(17)30012-1.
- Kong Y, Wang YT, Hu Y, Han W, Chang YJ, Zhang XH, Jiang ZF, Huang XJ. The bone marrow microenvironment is similarly impaired in allogeneic hematopoietic stem cell transplantation patients with early and late poor graft function. Bone Marrow Transplant. 2016;51:249-255.
- Rondón G, Saliba RM, Khouri I, Giralt S, Chan K, Jabbour E, McMannis J, Champlin R, Shpall E. Long-term follow up of patients who experienced graft failure post allogeneic progenitor cell transplantation. Results of a single institution analysis. Biol Blood Marrow Transplant. 2008; 14(8): 859–866.
- Kröger N, Holler E, Kobbe G, Bornhäuser M, Schwerdtfeger R, Baurmann H, Nagler A, Bethge W, Stelljes M, Uharek L, Wandt H, Burchert A, Corradini P, Schubert J, Kaufmann M, Dreger P, Wulf GG, Einsele H, Zabelina T, Kvasnicka HM, Thiele J, Brand R, Zander AR, Niederwieser D, de Witte TM. Allogeneic stem cell transplantation after reduced-intensity conditioning in patients with myelofibrosis: a prospective, multicenter study of the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation Blood. 2009;114(26):5264-5270.
- Dominietto A, Raiola AM, van Lint MT, Lamparelli T, Gualandi F, Berisso G, Bregante S, Frassoni F, Casarino L, Verdiani S and Bacigalupo A. Factors influencing haematological recovery after allogeneic haemopoietic stem cell transplants: graft-versus-host disease, donor type, cytomegalovirus infections and cell dose. Br J Haematol. 2001;112:219-227.
- Yu J-M, Emmons RV, Hanazono Y, Sellers S, Young NS, Dunbar CE. Expression of interferon-γ by stromal cells inhibits murine long-term repopulating hematopoietic stem cell activity. Exp Hematol. 1999;27(5):895-903.
- Kong Y, Wang Yu-Tong , Cao Xie-Na , Song Yang , Chen Yu-Hong , Sun Yu-Qian , Wang Yu , Zhang Xiao-Hui , Xu Lan-Ping, Huang Xiao-Jun. Aberrant T cell responses in the bone marrow microenvironment of patients with poor graft function after allogeneic hematopoietic stem cell transplantation. J Transl Med. 2017;15:57. doi: 10.1186/s12967-017-1159-y.
- Rudakova TA, Eismont YuA, Moiseev IS, Zubarovskaya LS, Kulagin AD, Afanasyev BV. Role of polyomavirus in emerging secondary hypofunction of marrow graft following allogeneic bone marrow transplantation in adults. Cellular Therapy and Transplantation. 2016;5(3):79–82. DOI: 10.18620/ctt-1866-8836-2016-5-3-79-82.
- Bao W, Bussel JB, Heck S, He W, Karpoff M, Boulad N, Yazdanbakhsh K. Improved regulatory T-cell activity in patients with chronic immune thrombocytopenia treated with thrombopoietic agents. Blood. 2010;116:4639–4645.
- Alvarado LJ, Andreoni A, Huntsman HD, Cheng H, Knutson JR, Larochelle A. Heterodimerization of TPO and IFNγ impairs human hematopoietic stem/progenitor cell signaling and survival in chronic inflammation. Blood. 2017;130:4.
- Lisukov IA, Uspenskaya OS, Kulagin AD, Bondarenko SN, Rudakova TA, Slesarchuk O.A., Afanasyev BV. Romiplostim in thrombocytopenia treatment after allogeneic bone marrow transplantation. Oncohematology. 2012;7(1):29–34. (In Russian).
- Marotta S, Marano L, Ricci P, Cacace F, Frieri C, Simeone L, Trastulli F, Vitiello S, Cardano F, Pane F, Risitano AM. Eltrombopag for post-transplant cytopenias due to poor graft function. Bone Marrow Transplant. 2019;54(8):1346-1353.
- Tang C, Chen F, Kong D, Ma Q, Dai H, Yin J, Li Zh, Chen Ji, Zhu X, Mao X, Wu D, Tang X. Successful treatment of secondary poor graft function post allogeneic hematopoietic stem cell transplantation with Eltrombopag. J Hematol Oncol. 2018 ;11:103 https://doi.org/10.1186/s13045-018-0649-6.
- Liga M. Romiplostim for the treatment of thrombocytopenia after allogeneic stem cell transplantation. The 45th Annual Meeting of EBMT (Physicians, Poster Session). Bone Marrow Transplantation. 2019;54:144–619, P143.
- Aguirre L. Eltrombopag (EPAG) induces a high percentage of responses in patients with post allo-HSCT poor graft function (PGF) and no active GVHD. The 45th Annual Meeting of EBMT (Physicians, Poster Session). Bone Marrow Transplantation. 2019;54:144–619, P133.
Татьяна А. Рудакова, Александр Д. Кулагин, Иван С. Моисеев, Татьяна А. Быкова, Сергей Н. Бондаренко, Мария В. Барабанщикова, Анастасия В. Бейнарович, Анна А. Осипова, Варвара Н. Овечкина, Александр Л. Алянский, Елена И. Дарская, Елена В. Морозова, Борис В. Афанасьев
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22295" ["VALUE"]=> array(2) { ["TEXT"]=> string(367) "<p>НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой Первого Санкт-Петербургского государственного медицинского университета им. И. П. Павлова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(355) "НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой Первого Санкт-Петербургского государственного медицинского университета им. И. П. Павлова, Санкт-Петербург, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_RU"]=> array(36) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22296" ["VALUE"]=> array(2) { ["TEXT"]=> string(6044) "<p style="text-align: justify;">Посттрансплантационные цитопении в структуре гипофункции трансплантата являются жизнеугрожающим осложнением аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК). Общепринятые терапевтические опции для лечения ограничены повторными инфузиями гемопоэтических стволовых клеток. Однако миметики тромбопоэтина (ТПО), показавшие свою эффективность при идиопатической апластической анемией и тромбоцитопении (ромиплостим, элтромбопаг), могут рассматриваться в качестве возможной альтернативной стратегии терапии гипофункции трансплантата после алло-ТГСК. В данной работе представлен опыт использования агонистов рецептора тромбопоэтина для лечения посттрансплантационных цитопений, в том числе критериальной тяжелой гипофункции трансплантата после алло-ТГСК в нашем центре.</p> <p style="text-align: justify;">В общей сложности 31 пациент (15 мужчин, 16 женщин) со средним возрастом 22 года (18-57) получили терапию агонистами рецептора ТПО (АР-ТПО) для посттрансплантационной тромбоцитопении <20×10<sup>9</sup>/л (n=7) и ГФТ (n=24). Для терапии использовался ромиплостим (n=17) со средней дозой 5 мкг/кг в неделю (3-5) или элтромбопаг (n=14) со средней дозой 50 мг/день (50-150). Критериями тяжелой гипофункции трансплантата (тГФТ) были: цитопения в двух или более миелоидных линиях (тромбоциты <20×10<sup>9</sup>/л, абсолютное число нейтрофилов (АЧН) <0,5×10<sup>9</sup>/л, гемоглобин <70 г/л в любое время после документированного приживления, полный или стабильный смешанный донорский химеризм >90% без признаков рецидива основного заболевания. Общий ответ включал полный ответ (ПО) (тромбоциты ≥100×10<sup>9</sup>/л, АЧН ≥1,5×109/л, гемоглобин ≥100 г/л) и частичный ответ (ЧО) (тромбоциты >20×10<sup>9</sup>/л, АЧН ≥0,5×10<sup>9</sup>/л, гемоглобин >70 г/л). Медиана времени от постановки диагноза тГФТ до начала терапии АР-ТПО составила 14 дней (0-119), медиана продолжительности терапии АР-ТПО составила 3 недели (1-43). Переносимость АР-ТПО была удовлетворительной, без признаков токсичности II-IV степени. В общей сложности в 8 случаях (28%) АР-ТПО использовались в комбинации с ритуксимабом (n=4), ритуксимабом и инфузиями донорских лимфоцитов (ИДЛ) (n=3), а также с инфузиями CD34-клеток (n=1). Всего 14 (48%) пациентов достигли ответа (ПО: n=4, 14%; ЧО: n=10, 34%). Комбинированная терапия не показала преимущества в скорости ответа по сравнению с АР-ТПО в монорежиме. Медиана прироста АЧН у ответивших на терапию составила 3,4×10<sup>9</sup>/л (0,8-6,0), тромбоцитов – 48×10<sup>9</sup>/л (21-205). В общей сложности 15 пациентов (3 ответивших, 12 не ответивших на терапию) умерли от инфекции (n=10), рецидива (n=2) и острой реакции «трансплантат-против-хозяина» (оРТПХ) III-IV степени (n=3). Однолетняя общая выживаемость (ОВ) от начала терапии составила 60% (95% ДИ, 40-76), при этом наблюдалась существенная разница между ответившими и неответившими на АР-ТПО: 79% (95% ДИ, 47-93) против 39% (95% ДИ, 14-63) (р=0,01). Наше исследование показало многообещающую эффективность и удовлетворительную безопасность АР-ТПО у пациентов с тГФТ после алло-ТГСК. Необходимо проведение многоцентровых проспективных исследований для установления оптимальной дозы и продолжительности приема, а также критериев отмены этих препаратов. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Алло-ТГСК, гипофункция трансплантата, агонисты рецепторов тромбопоэтина.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(5849) "Посттрансплантационные цитопении в структуре гипофункции трансплантата являются жизнеугрожающим осложнением аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК). Общепринятые терапевтические опции для лечения ограничены повторными инфузиями гемопоэтических стволовых клеток. Однако миметики тромбопоэтина (ТПО), показавшие свою эффективность при идиопатической апластической анемией и тромбоцитопении (ромиплостим, элтромбопаг), могут рассматриваться в качестве возможной альтернативной стратегии терапии гипофункции трансплантата после алло-ТГСК. В данной работе представлен опыт использования агонистов рецептора тромбопоэтина для лечения посттрансплантационных цитопений, в том числе критериальной тяжелой гипофункции трансплантата после алло-ТГСК в нашем центре.
В общей сложности 31 пациент (15 мужчин, 16 женщин) со средним возрастом 22 года (18-57) получили терапию агонистами рецептора ТПО (АР-ТПО) для посттрансплантационной тромбоцитопении <20×109/л (n=7) и ГФТ (n=24). Для терапии использовался ромиплостим (n=17) со средней дозой 5 мкг/кг в неделю (3-5) или элтромбопаг (n=14) со средней дозой 50 мг/день (50-150). Критериями тяжелой гипофункции трансплантата (тГФТ) были: цитопения в двух или более миелоидных линиях (тромбоциты <20×109/л, абсолютное число нейтрофилов (АЧН) <0,5×109/л, гемоглобин <70 г/л в любое время после документированного приживления, полный или стабильный смешанный донорский химеризм >90% без признаков рецидива основного заболевания. Общий ответ включал полный ответ (ПО) (тромбоциты ≥100×109/л, АЧН ≥1,5×109/л, гемоглобин ≥100 г/л) и частичный ответ (ЧО) (тромбоциты >20×109/л, АЧН ≥0,5×109/л, гемоглобин >70 г/л). Медиана времени от постановки диагноза тГФТ до начала терапии АР-ТПО составила 14 дней (0-119), медиана продолжительности терапии АР-ТПО составила 3 недели (1-43). Переносимость АР-ТПО была удовлетворительной, без признаков токсичности II-IV степени. В общей сложности в 8 случаях (28%) АР-ТПО использовались в комбинации с ритуксимабом (n=4), ритуксимабом и инфузиями донорских лимфоцитов (ИДЛ) (n=3), а также с инфузиями CD34-клеток (n=1). Всего 14 (48%) пациентов достигли ответа (ПО: n=4, 14%; ЧО: n=10, 34%). Комбинированная терапия не показала преимущества в скорости ответа по сравнению с АР-ТПО в монорежиме. Медиана прироста АЧН у ответивших на терапию составила 3,4×109/л (0,8-6,0), тромбоцитов – 48×109/л (21-205). В общей сложности 15 пациентов (3 ответивших, 12 не ответивших на терапию) умерли от инфекции (n=10), рецидива (n=2) и острой реакции «трансплантат-против-хозяина» (оРТПХ) III-IV степени (n=3). Однолетняя общая выживаемость (ОВ) от начала терапии составила 60% (95% ДИ, 40-76), при этом наблюдалась существенная разница между ответившими и неответившими на АР-ТПО: 79% (95% ДИ, 47-93) против 39% (95% ДИ, 14-63) (р=0,01). Наше исследование показало многообещающую эффективность и удовлетворительную безопасность АР-ТПО у пациентов с тГФТ после алло-ТГСК. Необходимо проведение многоцентровых проспективных исследований для установления оптимальной дозы и продолжительности приема, а также критериев отмены этих препаратов.
Ключевые слова
Алло-ТГСК, гипофункция трансплантата, агонисты рецепторов тромбопоэтина.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22297" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-38-44" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-38-44" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22313" ["VALUE"]=> array(2) { ["TEXT"]=> string(290) "<p>Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(278) "Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22314" ["VALUE"]=> array(2) { ["TEXT"]=> string(254) "<p>Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(242) "Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22331" ["VALUE"]=> array(2) { ["TEXT"]=> string(3345) "<p style="text-align: justify;">Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT. </p> <p style="text-align: justify;">A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×10<sup>9</sup>/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×10<sup>9</sup>/l, absolute neutrophil count (ANC) <0.5×10<sup>9</sup>/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×10<sup>9</sup>/l, ANC ≥1.5×10<sup>9</sup>/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×10<sup>9</sup>/l, ANC ≥0.5×10<sup>9</sup>/l, hemoglobin >70 g/l). Median time from diagnosis of sPGF to the start of TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×10<sup>9</sup>/l (0.8-6.0), platelets – 48×10<sup>9</sup>/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) <i>vs</i> 39% (95% CI, 14-63) (p=0.01). </p> <p style="text-align: justify;">Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.</p> <h2>Keywords</h2> <p style="text-align: justify;">Allo-HSCT, poor graft function, thrombopoietin receptor agonists.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3104) "Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT.
A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×109/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×109/l, absolute neutrophil count (ANC) <0.5×109/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×109/l, ANC ≥1.5×109/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×109/l, ANC ≥0.5×109/l, hemoglobin >70 g/l). Median time from diagnosis of sPGF to the start of TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×109/l (0.8-6.0), platelets – 48×109/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) vs 39% (95% CI, 14-63) (p=0.01).
Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.
Keywords
Allo-HSCT, poor graft function, thrombopoietin receptor agonists.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22298" ["VALUE"]=> string(136) "Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(136) "Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22299" ["VALUE"]=> string(4) "1645" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1645" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22315" ["VALUE"]=> string(4) "1646" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1646" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(12) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22313" ["VALUE"]=> array(2) { ["TEXT"]=> string(290) "<p>Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(278) "Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(278) "Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22331" ["VALUE"]=> array(2) { ["TEXT"]=> string(3345) "<p style="text-align: justify;">Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT. </p> <p style="text-align: justify;">A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×10<sup>9</sup>/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×10<sup>9</sup>/l, absolute neutrophil count (ANC) <0.5×10<sup>9</sup>/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×10<sup>9</sup>/l, ANC ≥1.5×10<sup>9</sup>/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×10<sup>9</sup>/l, ANC ≥0.5×10<sup>9</sup>/l, hemoglobin >70 g/l). Median time from diagnosis of sPGF to the start of TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×10<sup>9</sup>/l (0.8-6.0), platelets – 48×10<sup>9</sup>/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) <i>vs</i> 39% (95% CI, 14-63) (p=0.01). </p> <p style="text-align: justify;">Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.</p> <h2>Keywords</h2> <p style="text-align: justify;">Allo-HSCT, poor graft function, thrombopoietin receptor agonists.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3104) "Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT.
A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×109/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×109/l, absolute neutrophil count (ANC) <0.5×109/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×109/l, ANC ≥1.5×109/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×109/l, ANC ≥0.5×109/l, hemoglobin >70 g/l). Median time from diagnosis of sPGF to the start of TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×109/l (0.8-6.0), platelets – 48×109/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) vs 39% (95% CI, 14-63) (p=0.01).
Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.
Keywords
Allo-HSCT, poor graft function, thrombopoietin receptor agonists.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(3104) "Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT.
A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×109/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×109/l, absolute neutrophil count (ANC) <0.5×109/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×109/l, ANC ≥1.5×109/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×109/l, ANC ≥0.5×109/l, hemoglobin >70 g/l). Median time from diagnosis of sPGF to the start of TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×109/l (0.8-6.0), platelets – 48×109/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) vs 39% (95% CI, 14-63) (p=0.01).
Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.
Keywords
Allo-HSCT, poor graft function, thrombopoietin receptor agonists.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22297" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-38-44" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-38-44" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-38-44" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22298" ["VALUE"]=> string(136) "Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(136) "Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(136) "Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22314" ["VALUE"]=> array(2) { ["TEXT"]=> string(254) "<p>Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(242) "Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(242) "Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
" } ["AUTHORS"]=> array(38) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> array(13) { [0]=> string(5) "22470" [1]=> string(5) "22471" [2]=> string(5) "22472" [3]=> string(5) "22473" [4]=> string(5) "22474" [5]=> string(5) "22475" [6]=> string(5) "22476" [7]=> string(5) "22477" [8]=> string(5) "22478" [9]=> string(5) "22479" [10]=> string(5) "22480" [11]=> string(5) "22481" [12]=> string(5) "22482" } ["VALUE"]=> array(13) { [0]=> string(4) "1630" [1]=> string(3) "503" [2]=> string(2) "60" [3]=> string(4) "1642" [4]=> string(4) "1631" [5]=> string(3) "146" [6]=> string(4) "1629" [7]=> string(4) "1643" [8]=> string(3) "303" [9]=> string(3) "498" [10]=> string(3) "285" [11]=> string(3) "147" [12]=> string(2) "34" } ["DESCRIPTION"]=> array(13) { [0]=> string(0) "" [1]=> string(0) "" [2]=> string(0) "" [3]=> string(0) "" [4]=> string(0) "" [5]=> string(0) "" [6]=> string(0) "" [7]=> string(0) "" [8]=> string(0) "" [9]=> string(0) "" [10]=> string(0) "" [11]=> string(0) "" [12]=> string(0) "" } ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(13) { [0]=> string(4) "1630" [1]=> string(3) "503" [2]=> string(2) "60" [3]=> string(4) "1642" [4]=> string(4) "1631" [5]=> string(3) "146" [6]=> string(4) "1629" [7]=> string(4) "1643" [8]=> string(3) "303" [9]=> string(3) "498" [10]=> string(3) "285" [11]=> string(3) "147" [12]=> string(2) "34" } ["~DESCRIPTION"]=> array(13) { [0]=> string(0) "" [1]=> string(0) "" [2]=> string(0) "" [3]=> string(0) "" [4]=> string(0) "" [5]=> string(0) "" [6]=> string(0) "" [7]=> string(0) "" [8]=> string(0) "" [9]=> string(0) "" [10]=> string(0) "" [11]=> string(0) "" [12]=> string(0) "" } ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> array(13) { [0]=> string(63) "Tatiana A. Rudakova" [1]=> string(63) "Alexander D. Kulagin" [2]=> string(57) "Ivan S. Moiseev" [3]=> string(61) "Tatiana A. Bykova" [4]=> string(64) "Sergey N. Bondarenko" [5]=> string(66) "Maria V. Barabanshikova" [6]=> string(68) "Anastasia V. Beynarovich" [7]=> string(59) "Anna A. Osipova" [8]=> string(63) "Varvara N. Ovechkina" [9]=> string(65) "Alexander L. Alyanskiy" [10]=> string(60) "Elena I. Darskaya" [11]=> string(60) "Elena V. Morozova" [12]=> string(60) "Boris V. Afanasyev" } ["LINK_ELEMENT_VALUE"]=> bool(false) } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22294" ["VALUE"]=> array(2) { ["TEXT"]=> string(489) "<p>Татьяна А. Рудакова, Александр Д. Кулагин, Иван С. Моисеев, Татьяна А. Быкова, Сергей Н. Бондаренко, Мария В. Барабанщикова, Анастасия В. Бейнарович, Анна А. Осипова, Варвара Н. Овечкина, Александр Л. Алянский, Елена И. Дарская, Елена В. Морозова, Борис В. Афанасьев</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(477) "Татьяна А. Рудакова, Александр Д. Кулагин, Иван С. Моисеев, Татьяна А. Быкова, Сергей Н. Бондаренко, Мария В. Барабанщикова, Анастасия В. Бейнарович, Анна А. Осипова, Варвара Н. Овечкина, Александр Л. Алянский, Елена И. Дарская, Елена В. Морозова, Борис В. Афанасьев
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(477) "Татьяна А. Рудакова, Александр Д. Кулагин, Иван С. Моисеев, Татьяна А. Быкова, Сергей Н. Бондаренко, Мария В. Барабанщикова, Анастасия В. Бейнарович, Анна А. Осипова, Варвара Н. Овечкина, Александр Л. Алянский, Елена И. Дарская, Елена В. Морозова, Борис В. Афанасьев
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22278" ["VALUE"]=> string(22) "07/31/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "07/31/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "07/31/2019 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22279" ["VALUE"]=> string(22) "08/09/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "08/09/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "08/09/2019 12:00:00 am" } ["CONTACT"]=> array(38) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22280" ["VALUE"]=> string(4) "1630" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1630" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(63) "Tatiana A. Rudakova" ["LINK_ELEMENT_VALUE"]=> bool(false) } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22296" ["VALUE"]=> array(2) { ["TEXT"]=> string(6044) "<p style="text-align: justify;">Посттрансплантационные цитопении в структуре гипофункции трансплантата являются жизнеугрожающим осложнением аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК). Общепринятые терапевтические опции для лечения ограничены повторными инфузиями гемопоэтических стволовых клеток. Однако миметики тромбопоэтина (ТПО), показавшие свою эффективность при идиопатической апластической анемией и тромбоцитопении (ромиплостим, элтромбопаг), могут рассматриваться в качестве возможной альтернативной стратегии терапии гипофункции трансплантата после алло-ТГСК. В данной работе представлен опыт использования агонистов рецептора тромбопоэтина для лечения посттрансплантационных цитопений, в том числе критериальной тяжелой гипофункции трансплантата после алло-ТГСК в нашем центре.</p> <p style="text-align: justify;">В общей сложности 31 пациент (15 мужчин, 16 женщин) со средним возрастом 22 года (18-57) получили терапию агонистами рецептора ТПО (АР-ТПО) для посттрансплантационной тромбоцитопении <20×10<sup>9</sup>/л (n=7) и ГФТ (n=24). Для терапии использовался ромиплостим (n=17) со средней дозой 5 мкг/кг в неделю (3-5) или элтромбопаг (n=14) со средней дозой 50 мг/день (50-150). Критериями тяжелой гипофункции трансплантата (тГФТ) были: цитопения в двух или более миелоидных линиях (тромбоциты <20×10<sup>9</sup>/л, абсолютное число нейтрофилов (АЧН) <0,5×10<sup>9</sup>/л, гемоглобин <70 г/л в любое время после документированного приживления, полный или стабильный смешанный донорский химеризм >90% без признаков рецидива основного заболевания. Общий ответ включал полный ответ (ПО) (тромбоциты ≥100×10<sup>9</sup>/л, АЧН ≥1,5×109/л, гемоглобин ≥100 г/л) и частичный ответ (ЧО) (тромбоциты >20×10<sup>9</sup>/л, АЧН ≥0,5×10<sup>9</sup>/л, гемоглобин >70 г/л). Медиана времени от постановки диагноза тГФТ до начала терапии АР-ТПО составила 14 дней (0-119), медиана продолжительности терапии АР-ТПО составила 3 недели (1-43). Переносимость АР-ТПО была удовлетворительной, без признаков токсичности II-IV степени. В общей сложности в 8 случаях (28%) АР-ТПО использовались в комбинации с ритуксимабом (n=4), ритуксимабом и инфузиями донорских лимфоцитов (ИДЛ) (n=3), а также с инфузиями CD34-клеток (n=1). Всего 14 (48%) пациентов достигли ответа (ПО: n=4, 14%; ЧО: n=10, 34%). Комбинированная терапия не показала преимущества в скорости ответа по сравнению с АР-ТПО в монорежиме. Медиана прироста АЧН у ответивших на терапию составила 3,4×10<sup>9</sup>/л (0,8-6,0), тромбоцитов – 48×10<sup>9</sup>/л (21-205). В общей сложности 15 пациентов (3 ответивших, 12 не ответивших на терапию) умерли от инфекции (n=10), рецидива (n=2) и острой реакции «трансплантат-против-хозяина» (оРТПХ) III-IV степени (n=3). Однолетняя общая выживаемость (ОВ) от начала терапии составила 60% (95% ДИ, 40-76), при этом наблюдалась существенная разница между ответившими и неответившими на АР-ТПО: 79% (95% ДИ, 47-93) против 39% (95% ДИ, 14-63) (р=0,01). Наше исследование показало многообещающую эффективность и удовлетворительную безопасность АР-ТПО у пациентов с тГФТ после алло-ТГСК. Необходимо проведение многоцентровых проспективных исследований для установления оптимальной дозы и продолжительности приема, а также критериев отмены этих препаратов. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Алло-ТГСК, гипофункция трансплантата, агонисты рецепторов тромбопоэтина.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(5849) "Посттрансплантационные цитопении в структуре гипофункции трансплантата являются жизнеугрожающим осложнением аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК). Общепринятые терапевтические опции для лечения ограничены повторными инфузиями гемопоэтических стволовых клеток. Однако миметики тромбопоэтина (ТПО), показавшие свою эффективность при идиопатической апластической анемией и тромбоцитопении (ромиплостим, элтромбопаг), могут рассматриваться в качестве возможной альтернативной стратегии терапии гипофункции трансплантата после алло-ТГСК. В данной работе представлен опыт использования агонистов рецептора тромбопоэтина для лечения посттрансплантационных цитопений, в том числе критериальной тяжелой гипофункции трансплантата после алло-ТГСК в нашем центре.
В общей сложности 31 пациент (15 мужчин, 16 женщин) со средним возрастом 22 года (18-57) получили терапию агонистами рецептора ТПО (АР-ТПО) для посттрансплантационной тромбоцитопении <20×109/л (n=7) и ГФТ (n=24). Для терапии использовался ромиплостим (n=17) со средней дозой 5 мкг/кг в неделю (3-5) или элтромбопаг (n=14) со средней дозой 50 мг/день (50-150). Критериями тяжелой гипофункции трансплантата (тГФТ) были: цитопения в двух или более миелоидных линиях (тромбоциты <20×109/л, абсолютное число нейтрофилов (АЧН) <0,5×109/л, гемоглобин <70 г/л в любое время после документированного приживления, полный или стабильный смешанный донорский химеризм >90% без признаков рецидива основного заболевания. Общий ответ включал полный ответ (ПО) (тромбоциты ≥100×109/л, АЧН ≥1,5×109/л, гемоглобин ≥100 г/л) и частичный ответ (ЧО) (тромбоциты >20×109/л, АЧН ≥0,5×109/л, гемоглобин >70 г/л). Медиана времени от постановки диагноза тГФТ до начала терапии АР-ТПО составила 14 дней (0-119), медиана продолжительности терапии АР-ТПО составила 3 недели (1-43). Переносимость АР-ТПО была удовлетворительной, без признаков токсичности II-IV степени. В общей сложности в 8 случаях (28%) АР-ТПО использовались в комбинации с ритуксимабом (n=4), ритуксимабом и инфузиями донорских лимфоцитов (ИДЛ) (n=3), а также с инфузиями CD34-клеток (n=1). Всего 14 (48%) пациентов достигли ответа (ПО: n=4, 14%; ЧО: n=10, 34%). Комбинированная терапия не показала преимущества в скорости ответа по сравнению с АР-ТПО в монорежиме. Медиана прироста АЧН у ответивших на терапию составила 3,4×109/л (0,8-6,0), тромбоцитов – 48×109/л (21-205). В общей сложности 15 пациентов (3 ответивших, 12 не ответивших на терапию) умерли от инфекции (n=10), рецидива (n=2) и острой реакции «трансплантат-против-хозяина» (оРТПХ) III-IV степени (n=3). Однолетняя общая выживаемость (ОВ) от начала терапии составила 60% (95% ДИ, 40-76), при этом наблюдалась существенная разница между ответившими и неответившими на АР-ТПО: 79% (95% ДИ, 47-93) против 39% (95% ДИ, 14-63) (р=0,01). Наше исследование показало многообещающую эффективность и удовлетворительную безопасность АР-ТПО у пациентов с тГФТ после алло-ТГСК. Необходимо проведение многоцентровых проспективных исследований для установления оптимальной дозы и продолжительности приема, а также критериев отмены этих препаратов.
Ключевые слова
Алло-ТГСК, гипофункция трансплантата, агонисты рецепторов тромбопоэтина.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(5849) "Посттрансплантационные цитопении в структуре гипофункции трансплантата являются жизнеугрожающим осложнением аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК). Общепринятые терапевтические опции для лечения ограничены повторными инфузиями гемопоэтических стволовых клеток. Однако миметики тромбопоэтина (ТПО), показавшие свою эффективность при идиопатической апластической анемией и тромбоцитопении (ромиплостим, элтромбопаг), могут рассматриваться в качестве возможной альтернативной стратегии терапии гипофункции трансплантата после алло-ТГСК. В данной работе представлен опыт использования агонистов рецептора тромбопоэтина для лечения посттрансплантационных цитопений, в том числе критериальной тяжелой гипофункции трансплантата после алло-ТГСК в нашем центре.
В общей сложности 31 пациент (15 мужчин, 16 женщин) со средним возрастом 22 года (18-57) получили терапию агонистами рецептора ТПО (АР-ТПО) для посттрансплантационной тромбоцитопении <20×109/л (n=7) и ГФТ (n=24). Для терапии использовался ромиплостим (n=17) со средней дозой 5 мкг/кг в неделю (3-5) или элтромбопаг (n=14) со средней дозой 50 мг/день (50-150). Критериями тяжелой гипофункции трансплантата (тГФТ) были: цитопения в двух или более миелоидных линиях (тромбоциты <20×109/л, абсолютное число нейтрофилов (АЧН) <0,5×109/л, гемоглобин <70 г/л в любое время после документированного приживления, полный или стабильный смешанный донорский химеризм >90% без признаков рецидива основного заболевания. Общий ответ включал полный ответ (ПО) (тромбоциты ≥100×109/л, АЧН ≥1,5×109/л, гемоглобин ≥100 г/л) и частичный ответ (ЧО) (тромбоциты >20×109/л, АЧН ≥0,5×109/л, гемоглобин >70 г/л). Медиана времени от постановки диагноза тГФТ до начала терапии АР-ТПО составила 14 дней (0-119), медиана продолжительности терапии АР-ТПО составила 3 недели (1-43). Переносимость АР-ТПО была удовлетворительной, без признаков токсичности II-IV степени. В общей сложности в 8 случаях (28%) АР-ТПО использовались в комбинации с ритуксимабом (n=4), ритуксимабом и инфузиями донорских лимфоцитов (ИДЛ) (n=3), а также с инфузиями CD34-клеток (n=1). Всего 14 (48%) пациентов достигли ответа (ПО: n=4, 14%; ЧО: n=10, 34%). Комбинированная терапия не показала преимущества в скорости ответа по сравнению с АР-ТПО в монорежиме. Медиана прироста АЧН у ответивших на терапию составила 3,4×109/л (0,8-6,0), тромбоцитов – 48×109/л (21-205). В общей сложности 15 пациентов (3 ответивших, 12 не ответивших на терапию) умерли от инфекции (n=10), рецидива (n=2) и острой реакции «трансплантат-против-хозяина» (оРТПХ) III-IV степени (n=3). Однолетняя общая выживаемость (ОВ) от начала терапии составила 60% (95% ДИ, 40-76), при этом наблюдалась существенная разница между ответившими и неответившими на АР-ТПО: 79% (95% ДИ, 47-93) против 39% (95% ДИ, 14-63) (р=0,01). Наше исследование показало многообещающую эффективность и удовлетворительную безопасность АР-ТПО у пациентов с тГФТ после алло-ТГСК. Необходимо проведение многоцентровых проспективных исследований для установления оптимальной дозы и продолжительности приема, а также критериев отмены этих препаратов.
Ключевые слова
Алло-ТГСК, гипофункция трансплантата, агонисты рецепторов тромбопоэтина.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22295" ["VALUE"]=> array(2) { ["TEXT"]=> string(367) "<p>НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой Первого Санкт-Петербургского государственного медицинского университета им. И. П. Павлова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(355) "НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой Первого Санкт-Петербургского государственного медицинского университета им. И. П. Павлова, Санкт-Петербург, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(355) "НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой Первого Санкт-Петербургского государственного медицинского университета им. И. П. Павлова, Санкт-Петербург, Россия
" } } } [3]=> array(49) { ["IBLOCK_SECTION_ID"]=> string(3) "126" ["~IBLOCK_SECTION_ID"]=> string(3) "126" ["ID"]=> string(4) "1662" ["~ID"]=> string(4) "1662" ["IBLOCK_ID"]=> string(1) "2" ["~IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(273) "Клиническое значение феномена гиперэкспрессии гена BAALC при прогнозировании посттрансплантационных рецидивов у больных острым миелоидным лейкозом" ["~NAME"]=> string(273) "Клиническое значение феномена гиперэкспрессии гена BAALC при прогнозировании посттрансплантационных рецидивов у больных острым миелоидным лейкозом" ["ACTIVE_FROM"]=> NULL ["~ACTIVE_FROM"]=> NULL ["TIMESTAMP_X"]=> string(22) "09/29/2019 03:49:46 pm" ["~TIMESTAMP_X"]=> string(22) "09/29/2019 03:49:46 pm" ["DETAIL_PAGE_URL"]=> string(154) "/en/archive/tom-8-nomer-2/klinicheskie-issledovaniya/klinicheskoe-znachenie-fenomena-giperekspressii-gena-baalc-pri-prognozirovanii-posttransplantatsionn/" ["~DETAIL_PAGE_URL"]=> string(154) "/en/archive/tom-8-nomer-2/klinicheskie-issledovaniya/klinicheskoe-znachenie-fenomena-giperekspressii-gena-baalc-pri-prognozirovanii-posttransplantatsionn/" ["LIST_PAGE_URL"]=> string(12) "/en/archive/" ["~LIST_PAGE_URL"]=> string(12) "/en/archive/" ["DETAIL_TEXT"]=> string(41735) "Introduction
The Brain And Acute Leukemia Cytoplasmic (BAALC) gene becomes a new molecular star on the horizon of leukemia research. Its protein was initially discovered in the cytoplasm of central nervous system neuroderm cells [1]. Later on, a sufficient role of BAALC gene overexpression as a prognostic marker and pathogenetic factor of acute myeloid leukemia (AML) proved to be more obvious [2-4]. Initially, the BAALC overexpression was revealed in the patients with chromosome 8 trisomy, wherein BAALC gene maps. More recently, this abnormality has been demonstrated in 50-60% of AML patients with different morphological and cytogenetic variants [5-8]. Thus, BAALC gene overexpression proved to be rather specific for AML patients with t(8;21) translocation [5]. Meanwhile, the incidence of such phenomenon was also high in M0 and M1 AML FAB-variants [6]. On the contrary, it was observed extremely rare in AML M3 [7].
The BAALC gene expression has been recently shown to be closely associated with leukemic CD34+ but not CD34- precursor cell population which may initiate a relapse of acute leukemia that was shown in experiments with precursor cell enrichment [9-11]. Great contribution of early leukemic precursors, particularly CD34+/CD38- cells, to BAALC expression was demonstrated in other works [12], as documented by growing number of studies in the field [4, 13-18]. It is essential that the above-mentioned precursor cells with CD34+/CD38- phenotype may be responsible to regulate size of blast cell population, which, in turn, is able to express WT1 gene mRNA. Therefore, the latter gene is considered to be a basic molecular marker for AML relapses [19]. Since both these markers are functionally associated with changing levels of leukemic cells in AML patients treated by allogeneic hematopoietic stem cell transplantation (allo-HSCT), the parallel study of their expression seems to be quite important both in clinical and tumor biology aspects [5, 20].
One of such studies [5] included a cohort of 45 adult patients with core-binding-factor-positive AML, of which 28 cases had a standard t(8;21) translocation, and 17 patients harbored the inv(16) aberration. This work revealed that the patients with elevated BAALC gene expression level at diagnosis had shorter overall survival (OS) and relapse-free survival (RFS) (p=0.031, and p=0.011, respectively) along with significantly increased cumulative incidence of relapse (CIR) post-transplant (p=0.002). In this setting, the decrease of BAALC gene expression level following induction chemotherapy had no impact on results of allo-HSCT or auto-HSCT in one-third of this group.
This study has shown for the first time that the elevated BAALC and WT1 gene expression levels over post-transplant period in the patients with core-binding-factor-positive AML may be associated with unfavorable clinical prognosis. It should be noticed here, that all the associations between BAALC and WT1 gene expression and basic clinical parameters were obtained in the cohorts with intermediate or favorable cytogenetic AML variants. At the same time, such associations are not confirmed in more heterogeneous groups of patients, including both favorable and dismal AML variants [21]. When explaining these differences in clinical and laboratory characteristics among two patient groups, we consider an important role of particular chromosomal aberrations to be responsible for the transformation of leukemic cell precursors from the sleeping condition to more active state.
The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of WT1 and BAALC molecular markers expressed by appropriate cell types.
Patients and methods
Our study presents the data on WT1 and BAALC gene expression levels measured in parallel, during serial assays of bone marrow samples taken from sixty-one patients with initial diagnosis of AML. All the patients were treated with allo-HSCT at R. Gorbacheva Memorial Research Institute of Children Oncology, Hematology and Transplantation (St. Petersburg) from 2010 to 2016 years. The study group included 27 females and 34 males at the age of 3 to 66 years (median age 23.5 years old). Twelve patients were classified into the group with evident cytological remission (<4% in the bone marrow) at the time of HSCT, however, showing WT1 overexpression in the marrow samples [22]. Among the remaining 49 patients with different AML FAB-variants, serial BAALC and WT1 expression changes have been evaluated individually, being combined with blast cell counts in the same bone marrow aspirates.
Total mRNA extraction from fresh bone marrow samples, its reverse transcription and quantitative estimation of the BAALC gene expression level were performed as previously described [23]. Basic control time points for bone marrow sampling were as follows: at diagnosis (e.g., D-80), just before allo-HSCT, prior to the conditioning (D0) and after allo-HSCT, i.e. on D+30, D+60, D+90, D+150 and later post-transplant. The bone marrow sampling was obligatory in cases of PTR occurrence. A median follow-up time after HSCT was 7 months (range from 0.6 to 52.5). The analysis of BAALC gene expression included a total of 93 samples tested at clinical (cytologically proven) relapse, and 299 specimens were taken during clinical remission. In parallel, the WT1 gene expression levels and blast cell counts were determined in each sample at the same time points. A basal BAALC expression level of 31% to the reference gene was chosen as a common cut-off value to study clinical significance of BAALC gene overexpression before and after HSCT, in order to perform molecular monitoring of leukemic precursors and interaction of blast cell populations. This value was higher than the maximal BAALC gene expression in those patients with pre-transplant cytological remission who did not show any clinical signs of the disease progression. The copy numbers (CN) of WT1 transcripts was determined by the same quantitative real-time PCR method, according to recommendations of European LeukemiaNet group [24]. The basal WT1 expression level of 250 copies per 104 copies of ABL1 reference gene was applied to designate low and high WT1 expressors.
Statistical analysis
Descriptive statistics methods for data with asymmetric distribution were used, with evaluation of the sample ranges and median values. Two-year relapse-free survival (RFS) and cumulative incidence of relapse (CIR) were calculated using Kaplan-Meier method, and the log-rank test was used to compare differences between survival curves. RFS and CIR were measured from D0 until the date of death, regardless of cause, or until terms of documented relapse, or last contact date. P <0.05 was considered a statistically significant difference level. SPSS software version 22.0 (IBM corporation, Armonk, NY, USA) was used for statistical analysis.
Results
Initially, we estimated clinical significance of the BAALC gene overexpression in AML patients with a false cytological remission at the moment of transplantation. A term of "misleading" cytological remission was used to refer to clinical state with elevated WT1 expression level (higher than 250 copies per 104 copies of reference gene ABL1) combined with normal marrow blast counts (less than 5%). Among 12 such cases, nine patients (75%) did not express BAALC at the levels above the chosen cut-off of 31%, whereas increased BAALC expression was detected in three other patients. Despite limited number of tested AML cases, the RFS and CIR in the latter group appeared to be significantly worse, compared to those with low BAALC expression (р=0.019 и p=0.002, respectively), as seen from Fig. 1.

Figure 1. The difference between RFS (A) and CIR (B) depending on the BAALC gene expression level at the moment of allo-HSCT in the group of patients transplanted in a "misleading" cytological remission
Hence, one may conclude that the patients with combined WT1 and BAALC overexpression could be classified into prognostically unfavorable group, associated with high risk of early post-transplant relapse. This regulatory function seems to be retained in nine patients studied at the moment of transplantation. However, it could be lost in three other patients, in whom a combined WT1 and BAALC overexpression took place.
The BAALC and WT1 expression levels for the previously discussed AML patients [23] were assessed in the context of our recent findings. As shown in Fig. 2, the highest BAALC expression levels were observed in relapsing patients with AML classified as M1 and M2 FAB-variants, with intermediate values in M0, M4 and M5 FAB-variants of AML. The lowest BAALC expression was detected in AML M3 and M7 cases.

Figure 2. Distribution of individual values and median levels of BAALC gene expression in relapsing patients with different AML FAB-variants
In addition, we have studied the BAALC gene expression levels in patients with different cytogenetic AML variants. According to our data, the highest BAALC gene expression levels among cases with favorable cytogenetic changes were observed in the patients with t(8;21) (N=21), and in subgroups with unfavorable karyotype, i.e., aberrations in chromosomes 5 and 7 (N=23), as well as complex karyotype (N=8), and other severe abnormalities (≤2) (N=11, data not shown). In cases of relapse, no statistically significant differences of BAALC gene expression levels were noted between these subgroups.
The patient cohort with higher BAALC gene expression (>31% in relapse) consisted of 30 out of 50 cases (60%), including eight patients with both M1 and M2 FAB- variants of AML. A combined BAALC and WT1 overexpression was observed in 28 cases of 30 (93.3%). The data on two patients with M1 and M2 FAB-variants of AML are shown below (Fig. 3, 4).

Figure 3. Monitoring of BAALC and WT1 mRNA expression levels measured by QR-PCR, and bone marrow blast numbers in a patient with AML M1 (№4)
Note: The values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and during 1 to 3 PTRs were 1.3; 0.15; 1.25; 1.54 for BAALC gene, and 1.05; 0.03; 0.05 and 0.03 for the WT1 gene, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).

Figure 4. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in young patient with AML M2 (№12) measured by QR-PCR of BAALC and WT1 mRNA expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in two PTRs were 0.04; 1.5; 0.47 for gene BAALC and 0.07; 0.24; 0.27 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
As seen from Fig. 2 and Table 2, the BAALC gene expression levels in PTR were higher in patients with AML M1 and M2, and sufficiently lower in AML M4. In order to discuss in details some special interactions between leukemic cell precursors and blast cell populations, determined by means of QR-PCR, we have demonstrated here complete clinical and laboratory characteristics from a larger group of patients with different cytological and cytogenetic AML variants according to FAB criteria. Our study cohort consisted of 22 patients (11 cases for each AML M1 and M2- variants). Twenty one of them had a fully characterized cell karyotype. Simultaneous overexpression of both BAALC and WT1 genes at PTR was detected in four and three AML M1 and M2 cases, respectively (Table 2). As based on these data, the presence of a combined gene overexpression in the patients at post-transplant period is considered an index of unfavorable prognosis.
Table 2. BAALC and WT1 gene expression levels at diagnosis, before allo-HSCT (D0) and at PTRs after hematopoietic stem cell transplantation in the patients with different AML FAB-variants


As seen from Table 2, simultaneous overexpression of BAALC and WT1 genes at relapse at any stage of the disease (at diagnosis, D0 pre-transplant, or PTR) occurred in 28/55 (56%) patients. It was observed in eight patients with AML M1 (72.7%), 8 patients with AML M2 (72.7%), as well as in 1 (33.3%), 8 (50%), 2 (40%) patients with AML M0, M4, and M5, respectively.
To illustrate this concept, several clinical cases of each AML M1, M2 and M4 FAB-variants are represented below (Fig. 3 to 5). The relative ratios of leukemic cell precursors or blast cell burdens were monitored as BAALC and WT1 gene expression levels, respectively, as shown for a patient with AML M1 (Table 2, Fig. 3). In this case No.4, a simultaneous BAALC and WT1 overexpression took place at diagnosis, and at 2nd and 3rd PTRs that occured despite second HSCT and high-dose chemotherapy which was unsuccessful.
In this case, cytogenetic characteristics of leukemic cells were different for the 1st and 2nd relapses. At the first PTR, complex karyotype changes included loss of chromosome X, deletion of 11q and additional chromosome 21 revealed in 15% of tested cells, whereas additional unbalanced translocations t(X;17), t(1;3), and t(1;17) were detected in the second PTR.
In another AML case No. 12 (M2 variant) with t(8;21) translocation (Fig. 4), a simultaneous measurement of BAALC and WT1 gene expression levels revealed overexpression of the WT1 gene at diagnosis, with bone marrow blast burden of up to 28%. Further on, a combined overexpression of both molecular markers was associated with 1st and 2nd relapses, thus being prognostically unfavorable. One may suggest that the disease progression and fatal outcome occurred due to resistance of tumor cells to therapy.
Similar clinical situation was observed in the next patient with AML M4 (No. 31), who received allotransplant at the age of five years. In spite of t(8;21) translocation found at diagnosis, thus classifying the patient into favorable group, an additional deletion 7q – del(7)(q32q36) before transplant allowed, however, to evaluate this case as unfavorable one. The combined BAALC and WT1 overexpression at diagnosis, as well as in first PTR, was accompanied by increased expression level of a specific RUNX1/RUNX1T1 fusion transcript (Fig. 5). Of notice, the blast burden in the bone marrow sample at relapse (D+223) was not too high, wherein hypothetic inhibition of leukemic precursor cells from side of the blast population was minimal, thus explaining higher BAALC gene expression levels observed.

Figure 5. Molecular monitoring of interactions between leukemic cell precursors and blast cells in the patient with AML M4 (№31) measured by QR-PCR of BAALC, WT1 and RUNX1/RUNX1T1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.95; 0.35 for gene BAALC and 0.1; 0.04 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Another clinical case (No. 29) concerns a female patient 21 years old with AML M4 FAB variant (Fig. 6). The first concomitant overexpression of BAALC and WT1 genes has been observed pre-transplant, associated with complex structural chromosomal changes, i.e., monosomy 7, t(2;3) translocation, as well as 3q inversion. All these abnormalities seemed to correlate with a failure to achieve full cytological and molecular remissions. It has been combined with overexpression of both BAALC and WT1 genes during the entire posttransplant period. From this point of view, it is not surprising that the first PTR occurred early on D+80 after transplantation. Prognostically unfavorable simultaneous WT1 and BAALC overexpression, as well as the same clonal changes of karyotype were detected again at that time. The second clinical relapse was detected on the day D+232 posttransplant, when overexpression of the both genes was expressed even more, and a new additional chromosomal abnormality (monosomy 5) was detected on day D+251.

Figure 6. Molecular monitoring of the interaction between leukemic cell precursors and blast cells burdens in patient with AML M4 (№29) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in two PTRs were 1.07; 3.9; 4 for gene BAALC and 0.09; 0.12; 2.6 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Another molecular profile has been revealed during serial measurement of BAALC and WT1 gene expression levels in a 55-year old female patient (Case No. 40, Table 2) with the same AML M4 FAB-variant, but with normal karyotype (Fig. 7). As shown here, the elevated WT1 gene expression level took place not only in pre-transplant relapse, but in early PTR as well, which seems to be a result of transplantation without subsequent cytological remission. At the same time, the BAALC gene overexpression was not observed at neither of relapses. Instead of successful treatment of the first PTR at D+65 after allo-HSCT, the patient developed a new cytological relapse accompanied by the WT1 gene overexpression, and the lethal outcome was detected at D+101 after allo-HSCT.

Figure 7. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in patient with AML M4 (№40) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.035; 0.0006 for gene BAALC and 1.17; 0.1 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
As regards special AML forms, characterized by the absence of BAALC overexpression we observed in 4 (8%) of 50 such cases in our cohort (three among them had AML M3 and one, M7 FAB-variant). Data of the serial parallel measurement of BAALC and WT1 gene expression levels in one of them are represented at Figure 8. Elevated BAALC gene expression level over the cut-off level in a 17-year-old female patient (№ 47) was not observed both at relapse before allo-HSCT, or in posttransplant relapse. At the same time, a significant WT1 gene overexpression took place in both relapses.

Figure 8. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in a 17-years old female patient with AML M3 (№47) measured by QR-PCR of BAALC, WT1 and PML-RARα gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.035; 0.0006 for gene BAALC and 1.17; 0.1 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
In general, the results shown in Fig. 8 may be explained by more differentiated state of promyelocytes providing clinical development of acute promyelocytic leukemia, compared to CD34+/CD38- cell precursors of leukemic hematopoiesis. By this reason, they are unable to express BAALC gene. On the other hand, some, still unknown, immature leukemic cells in M3 FAB- variant AML must have a direct cause higher WT1 gene expression levels which should be studied at regular basis.
It is reasonable to present here some data on parallel measurement of BAALC and WT1 gene expression level in bone marrow samples from a 3-year-old female patient (№49) with AML M7 (Fig. 9). The BAALC gene expression level was under the cut-off value during the entire follow-up period. At the same time, WT1 gene overexpression closely associated with increasing blast burden in bone marrow, was detected during relapse before HSCT, as well as at the posttransplant relapse with pronounced blastosis in bone marrow (>60%).

Figure 9. Molecular monitoring of the interaction between leukemic cell precursors and blast cells in a 3-years old female patient with AML M7 (№49) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.0025; 0.0003 for gene BAALC and 0.03; 0.69 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Finally, we would like to demonstrate here some special biological features of blast elements in AML patients, who did not exhibit WT1 gene overexpression. E.g., we present the graphs of molecular monitoring by WT1 and BAALC expression levels in two patients (No. 24 and 26) with M0 AML (Fig. 10) and M4 AML (Fig. 11). The first case presents a 25-year old patient (№24), who had reciprocal translocation t(3;10)(p21;p11) (without EVI1 gene overexpression), and interstitial deletion of chromosome 11 long arm (without MLL gene rearrangements, as shown by FISH technique). According to this graph, the BAALC gene expression level over the cut-off value was detected at relapse before transplantation, as well as at PTR, whereas WT1 gene expression level changes were <250 copies per 104 copies of ABL1 gene during entire period of study. The lethal outcome of the disease on the D+133 after transplantation has been associated with progression.

Figure 10. Molecular monitoring of the interaction between leukemic cell precursors and blast cells in a patient with AML M0 (№24) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 1.24; 0.82 for gene BAALC and 0.0003; 0.0005 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
The data from another clinical case are demonstrated in the Figure 11. They relate to a 6-years old patient, who had permanently relapsing disease course and has undergone haploidentical hematopoietic stem cell transplantation in cytological relapse for this reason. In this case, a distinct increase in BAALC expression level has been observed upon relapse before HSCT, as well as at the first PTR on the day D+246. The WT1 expression level at relapse before transplantation and at first PTR was did not exceed the cut-off level. It is equally important that, according to cytogenetic data, this patient has undergone a clonal evolution over the period between diagnosis and first PTR karyotyping associated with its transformation from normal to complex one, including rearrangements of both chromosomes 5, as well as X, 2, 6, 9 and 19. For the first post-transplant relapse, the patient has been treated by polychemotherapy in combination with donor lymphocyte infusion and 5-azacytidin. Such supportive therapy allowed morphological remission for a sufficient period of time. However, the disease progression was detected again on the day D+734 posttransplant, as evidenced by a combined cytological relapse with myelomonocytic blast cells. Their immune profile was as follows: CD34+/CD33+/CD117+/CD13+/CD38+/CD14+ associated with complex clonal rearrangements of chromosomes 2, 5 and 19. It should be noted, that, at the second PTR, this patient had both BAALC and WT1 genes overexpression, what may be explained by hypothetical changes of negative regulation of leukemic precursors by the blast cell burden. Finally, lethal outcome has occurred in this case on the day D+779 post-transplant.

Figure 11. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in a 6 years old patient with AML M4 (№26) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in the first and second PTRs were 9.8; 71.2; 18.6 for gene BAALC and 0.02; 0.03; 0.21 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Discussion
The data presented here show an opportunity for simultaneous BAALC and WT1 gene overexpression in a group of AML patients with increased levels of WT1 and normalized up to 4% number of blasts in bone marrow samples. Therefore, it could be considered a strong indicator of poor prognosis in these cases. On the other hand, the levels of BAALC and WT1 levels expression determined by means of PCR may reflect, in a quantitative manner, the relative sizes of precursor and blast cell burden. Of note, hypothetical correlation between these tumor compartments has not elucidated yet, and may be not obligatory for all AML cases. The study has shown that the absence of BAALC overexpression at transplantation was associated with lower CIR in 9 of 12 patients (75%) with abovementioned intermediate clinical status. On the contrary, the 3 other patients with elevated BAALC expression before transplant revealed earlier PTR development associated with shorter 2-year OS and EFS, as compared with the main group of patients. Hence, an assumption was made that simultaneous overexpression of BAALC and WT1 may be a useful indicator of dismal post-transplant AML course. Keeping this in mind, we showed a double overexpression phenomenon to be present in four patients with M1 (N=2), M2 (n=1) and M4 (n=1) AML variants associated with poor prognosis. Further on, our data showed the levels of BAALC expression to be similarly high in patients with immature and mature M1 and M2 FAB-variants, respectively. On the other hand, the lowest BAALC expression levels were noticed in patients with M3 and M7 AML FAB- variants. Today, the absence of BAALC gene expression in patients with acute promyelocytic leukemia may be explained by its origin from more “mature” cell populations than the standard CD34+CD38– precursors producing BAALC [25]. The same situation seems exist in the M7 FAB variants of AML, which also needs a similar additional study.
In our opinion, the results of BAALC gene expression measurement in patients with M2 and M4 FAB-variants are interesting in several regards. Firstly, high expression of BAALC and WT1 genes were synchronous in most cases. At the same time, the numbers of blast elements in their bone marrow aspirates increased to lower degree than expected. The simplest explanation for this discordance between findings in AML variants and cell maturity may be that these blast elements can differentiate only partially and, therefore, transform into more mature cellular populations. However, due to decreased size of blast population preserved in this kind of AML, some hypothetical regulating mechanisms can be activated for additional recruitment of new portions of CD34+CD38- precursors into leukemic hematopoiesis. Due to mentioned transition of blast elements to the more mature hematopoietic compartments, as well as their hypothetical regulator mechanism between blast burden and leukemic precursor compartment, the revealed similarity in gene BAALC overexpression for M2 and M4 FAB- variants of AML, and those in M1 and M0 FAB variants may be explained in these terms.
In conclusion, it should be like to notice, that clinical significance of our findings, concerning simultaneous overexpression of BAALC and WT1 genes in adults and children with AML treated with allo-HSCT, and/or donor lymphocyte infusions was presented for the first time and could be effectively used for clinical diagnostics and prediction of relapses in AML patients. The combined WT1 and BAALC overexpression was studied in relatively small group of patients, thus requiring further confirmation in larger groups of patients with different FAB variants of AML.
Conflict of interest
No conflict of interests is declared.
References
- Tanner S, Austin J, Leone G, Rush L, Plass C, Heinonen K, Mrózek K, Still H, Knuutila S, Kolitz J, Archer K, Caligiuri M, Bloomfield C, de la Chapelle A. BAALC, the human member of a novel mammalian neuroectoderm gene lineage, is implicated in hematopoiesis and acute leukemia. Proc Natl Acad Sci USA. 2001;98(24):13901-13906.
- Santamaría C, Chillón M, García-Sanz R, Pérez C, Caballero M, Mateos M, Ramos F, de Coca A, Alonso J, Giraldo P, Bernal T, Queizán J, Rodríguez J, Puig N, Balanzategui A, Sarasquete M, Alcoceba M, Díaz-Mediavilla J, San Miguel J, González M. BAALC is an important predictor of refractoriness to chemotherapy and poor survival in intermediate-risk acute myeloid leukemia (AML). Ann Hematol. 2010;89:453-458.
- Weber S, Haferlach T, Alpermann T, Perglerová K, Schnittger S, Haferlach C, Kern W. Feasibility of BAALC gene expression for detection of minimal residual disease and risk stratification in normal karyotype acute myeloid leukemia. Br J Haematol. 2016;175(5):904-916.
- Jentzsch M, Bill M, Grimm J, Schulz J, Goldmann K, Beinicke S, Häntschel J, Pönish W, Franke G-N, Vicinic V, Behre G, Lange T, Niederwiesser D, Schwind S. High BAALC copy numbers in peripheral blood prior to allogeneic transplantation predict early relapse in acute myeloid leukemia. Oncotarget. 2017;8(50):87994-97954.
- Yoon J, Kim H, Shin S, Yahng S, Lee S, Cho S, Eom K, Kim Y, Lee S, Min C, Cho S, Kim D, Lee J, Min W, Park C, Lim J. BAALC and WT1 expressions from diagnosis to hematopoietic stem cell transplantation: consecutive monitoring in adult patients with core-binding–factor-positive AML. Europ J Haematol. 2013;91:112-127.
- Xiao S, Shen J, Huang J, Fu H. Prognostic significance of the BAALC gene expression in adult patients with acute myeloid leukemia: A meta-analysis. Mol Clin Oncol. 2015;3(4):880-888.
- Hecht A, Doll S, Altmann H, Nowak D, Lengfelder E, Röllig C, Ehninger G, Spiekermann K, Hiddemann W, Weiß C, Hofmann W, Nolte F, Platzbecker U. Validation of a molecular risk score for prognosis of patients with acute promyelocytic leukemia treated with all-trans retinoic acid and chemotherapy-containing regimens. Clin Lymphoma Myeloma Leuk. 2017; 17(12):889-896.e5.
- Staffas A, Kanduri M, Hovland R, Rosenquist R, Ommen HB, Abrahamsson J, Forestier E, Jahnukainen K, Jónsson ÓG, Zeller B, Palle J, Lönnerholm G, Hasle H, Palmqvist L, Ehrencrona H; Nordic Society of Pediatric Hematology and Oncology (NOPHO). Presence of FLT3-ITD and high BAALC expression are independent prognostic markers in childhood acute myeloid leukemia. Blood. 2011 Nov 24;118(22):5905-13.
- Najima Y, Ohashi K, Kawamura M, Onozuka Y, Yamaguchi T, Akiyama H, et al. Molecular monitoring of BAALC expression in patients with CD34-positive acute leukemia. Int J Hematol. 2010;91:636–645.
- Damiani D, Tiribelli M, Franzoni A, Michelutti A, Fabbro D, Cavallin M, Toffoletti E, Simeone E, Fanin R, Damante G. BAALC overexpression retains its negative prognostic role across all cytogenetic risk groups in acute myeloid leukemia patients. Am J Hematol. 2013;88(10):848-852.
- Pogosova-Agadjanyan E, Moseley A, Othus M, Appelbaum F, Chauncey T, Chen I, Erba H, Godwin J, Fang M, Kopecky K, List A, Pogosov G, Radich J, Willman C, Wood B, Meshinchi S, Stirewalt D. Impact of specimen heterogeneity on biomarkers in repository samples from patients with acute myeloid leukemia: A SWOG report. Biopreserv Biobank. 2018;16(1):42-52.
- Morita K, Masamoto Y, Kataoka K, Koya J, Kagoya Y, Yashiroda H, Sato T, Murata S, Kurokawa M. BAALC potentiates oncogenic ERK pathway through interactions with MEKK1 and KLF4. Leukemia. 2015;29(11):2248-2456.
- Costello R, Mallet F, Gaugler B, Sainty D, Arnoulet C, Gastaut J, Olive D. Human acute myeloid leukemia CD34+/CD38- progenitor cells have decreased sensitivity to chemotherapy and Fas-induced apoptosis? Reduced immunogenicity, and impaired dendritic cell transformation capacities. Cancer Res. 2000;60:4403-4411.
- Gerber J, Smith B, Ngwang B, Zhang H, Vala M, Morsberger L, Galkin S, Collector M, Perkins B, Levis M, et al. A clinically relevant population of leukemic CD34+CD38- cells in acute myeloid leukemia. Blood. 2012;119(15):3571-3577.
- Gerber J, Zeidner J, Morse S, Blackford A, Perkins B, Yanagisawa B, Zhang H, Morsberger L, Karp J, Ning Y, Cocke C, Rosner G, Smith D, Jones R. Association of acute myeloid leukemia’s most immature phenotype with risk groups and outcomes. Haematologica. 2016;101950;607-615.
- Jentzsch M, Bill M, Nicolet D, Leiblein S, Schubert K, Pless M, Bergmann U, Wildenberger K, Schuhmann L, Cross M, et al. Prognostic impact of the CD34+/CD38- cell burden in patients with acute myeloid leukemia receiviung allogeneic stem cell transplantation. Am J Hematol. 2017;92(4):388-396.
- Plesa A, Dumontet C, Mattei E, Tagoug I, Hayette S, Sujobert P, Tigaud I, Pages M, Chelghome Y, Baracco F, et al. High frequqncy of CD34+CD38-/low immature leukemia cells is correlated with unfavorable prognosis in acute leukemia. World J Stem Cells. 2017;9(12):227-234.
- Thomas D, Majeti R. Biology and relevance of human acute myeloid leukemia stem cells. Blood. 2017;129(12):1577–1585.
- Mamaev N, Gudozhnikova Y, Gindina T, Barkhatov I, Shakirova A, Katerina V, Gubina M, Nikolaeva E, Semenova E, Paina O, Darskaya E, Pirogova O, Porunova V, Moiseev I, Mikhailova I, Ayubova B, Kravtsova V, Bondarenko S, Zubarovskaya L, Afanasyev B. Efficacy of Chemotherapy in Acute Leukemia Patients Resistant to Previous Standard Treatment According to the Series Measurement of WT1 Gene Expression. Clinical Oncohematology. 2018;11(1):78-88 (In Russian).
- Minetto P, Guolo F, Clavio M, de Astis E, Colombo N, Grasso R, Fugazza G, Sessarego M, Lemoli R, Gobbi M, Miglino M. Combined assessment of WT1 and BAALC gene expression at diagnosis may improve leukemia-free survival prediction in patients with myelodysplastic syndromes. Leukemia Res. 2015;39:866-873.
- Haferlach C, Kern W, Schindela S, Kohlmann A, Alpermann T, Schnittger S, Haferlach T. Gene expression of BAALC, CDKN1B, ERG, and MN1 adds independent prognostic information to cytogenetics and molecular mutations in adult acute myeloid leukemia. Genes Chromosomes Cancer. 2012;51(3):257-265.
- Gudozhnikova Y, Mamaev N, Barkhatov I, Katerina V, Gindina T, Shakirova A, Bondarenko S, Slesarchuk O, Darskaya E, Paina O, Zubarovskaya L, Afanasyev B. Results of Molecular Monitoring in Post-transplant Period by Means of Series Investigation of WT1 Gene Expression in Patients with Acute Myeloid Leukemia. Clinical Oncohematology. 2018;11(3):241-251 (In Russian).
- Shakirova A, Barkhatov I, Churkina A, Moiseev I, Gindina T, Bondarenko S, Afanasyev B. Prognostic significance of BAALC overexpression in patients with AML during the post-transplant period. Cell Ther Transplant. 2018;7(2):54-63.
- Cilloni D, Renneville A, Hermitte F, Hills R, Daly S, Jovanovic J, Gottardi E, Fava M, Schnittger S, Weiss T, Izzo B, Nomdedeu J, van der Heijden A, van der Reijden B, Jansen J, van der Velden V, Ommen H, Preudhomme C, Saglio G, Grimwade D. Real-time quantitative polymerase chain reaction detection of minimal residual disease by standardized WT1 assay to enhance risk stratification in acute myeloid leukemia: a European LeukemiaNet study. J Clin Oncol. 2009;27(31):5195-5201.
- Reinisch A, Thomas D, Corces MR, et al. A humanized bone marrow ossicle xenotransplantation model enables improved engraftment of healthy and leukemic human hematopoietic cells. Nat Med. 2016;22(7):812-821.
Introduction
The Brain And Acute Leukemia Cytoplasmic (BAALC) gene becomes a new molecular star on the horizon of leukemia research. Its protein was initially discovered in the cytoplasm of central nervous system neuroderm cells [1]. Later on, a sufficient role of BAALC gene overexpression as a prognostic marker and pathogenetic factor of acute myeloid leukemia (AML) proved to be more obvious [2-4]. Initially, the BAALC overexpression was revealed in the patients with chromosome 8 trisomy, wherein BAALC gene maps. More recently, this abnormality has been demonstrated in 50-60% of AML patients with different morphological and cytogenetic variants [5-8]. Thus, BAALC gene overexpression proved to be rather specific for AML patients with t(8;21) translocation [5]. Meanwhile, the incidence of such phenomenon was also high in M0 and M1 AML FAB-variants [6]. On the contrary, it was observed extremely rare in AML M3 [7].
The BAALC gene expression has been recently shown to be closely associated with leukemic CD34+ but not CD34- precursor cell population which may initiate a relapse of acute leukemia that was shown in experiments with precursor cell enrichment [9-11]. Great contribution of early leukemic precursors, particularly CD34+/CD38- cells, to BAALC expression was demonstrated in other works [12], as documented by growing number of studies in the field [4, 13-18]. It is essential that the above-mentioned precursor cells with CD34+/CD38- phenotype may be responsible to regulate size of blast cell population, which, in turn, is able to express WT1 gene mRNA. Therefore, the latter gene is considered to be a basic molecular marker for AML relapses [19]. Since both these markers are functionally associated with changing levels of leukemic cells in AML patients treated by allogeneic hematopoietic stem cell transplantation (allo-HSCT), the parallel study of their expression seems to be quite important both in clinical and tumor biology aspects [5, 20].
One of such studies [5] included a cohort of 45 adult patients with core-binding-factor-positive AML, of which 28 cases had a standard t(8;21) translocation, and 17 patients harbored the inv(16) aberration. This work revealed that the patients with elevated BAALC gene expression level at diagnosis had shorter overall survival (OS) and relapse-free survival (RFS) (p=0.031, and p=0.011, respectively) along with significantly increased cumulative incidence of relapse (CIR) post-transplant (p=0.002). In this setting, the decrease of BAALC gene expression level following induction chemotherapy had no impact on results of allo-HSCT or auto-HSCT in one-third of this group.
This study has shown for the first time that the elevated BAALC and WT1 gene expression levels over post-transplant period in the patients with core-binding-factor-positive AML may be associated with unfavorable clinical prognosis. It should be noticed here, that all the associations between BAALC and WT1 gene expression and basic clinical parameters were obtained in the cohorts with intermediate or favorable cytogenetic AML variants. At the same time, such associations are not confirmed in more heterogeneous groups of patients, including both favorable and dismal AML variants [21]. When explaining these differences in clinical and laboratory characteristics among two patient groups, we consider an important role of particular chromosomal aberrations to be responsible for the transformation of leukemic cell precursors from the sleeping condition to more active state.
The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of WT1 and BAALC molecular markers expressed by appropriate cell types.
Patients and methods
Our study presents the data on WT1 and BAALC gene expression levels measured in parallel, during serial assays of bone marrow samples taken from sixty-one patients with initial diagnosis of AML. All the patients were treated with allo-HSCT at R. Gorbacheva Memorial Research Institute of Children Oncology, Hematology and Transplantation (St. Petersburg) from 2010 to 2016 years. The study group included 27 females and 34 males at the age of 3 to 66 years (median age 23.5 years old). Twelve patients were classified into the group with evident cytological remission (<4% in the bone marrow) at the time of HSCT, however, showing WT1 overexpression in the marrow samples [22]. Among the remaining 49 patients with different AML FAB-variants, serial BAALC and WT1 expression changes have been evaluated individually, being combined with blast cell counts in the same bone marrow aspirates.
Total mRNA extraction from fresh bone marrow samples, its reverse transcription and quantitative estimation of the BAALC gene expression level were performed as previously described [23]. Basic control time points for bone marrow sampling were as follows: at diagnosis (e.g., D-80), just before allo-HSCT, prior to the conditioning (D0) and after allo-HSCT, i.e. on D+30, D+60, D+90, D+150 and later post-transplant. The bone marrow sampling was obligatory in cases of PTR occurrence. A median follow-up time after HSCT was 7 months (range from 0.6 to 52.5). The analysis of BAALC gene expression included a total of 93 samples tested at clinical (cytologically proven) relapse, and 299 specimens were taken during clinical remission. In parallel, the WT1 gene expression levels and blast cell counts were determined in each sample at the same time points. A basal BAALC expression level of 31% to the reference gene was chosen as a common cut-off value to study clinical significance of BAALC gene overexpression before and after HSCT, in order to perform molecular monitoring of leukemic precursors and interaction of blast cell populations. This value was higher than the maximal BAALC gene expression in those patients with pre-transplant cytological remission who did not show any clinical signs of the disease progression. The copy numbers (CN) of WT1 transcripts was determined by the same quantitative real-time PCR method, according to recommendations of European LeukemiaNet group [24]. The basal WT1 expression level of 250 copies per 104 copies of ABL1 reference gene was applied to designate low and high WT1 expressors.
Statistical analysis
Descriptive statistics methods for data with asymmetric distribution were used, with evaluation of the sample ranges and median values. Two-year relapse-free survival (RFS) and cumulative incidence of relapse (CIR) were calculated using Kaplan-Meier method, and the log-rank test was used to compare differences between survival curves. RFS and CIR were measured from D0 until the date of death, regardless of cause, or until terms of documented relapse, or last contact date. P <0.05 was considered a statistically significant difference level. SPSS software version 22.0 (IBM corporation, Armonk, NY, USA) was used for statistical analysis.
Results
Initially, we estimated clinical significance of the BAALC gene overexpression in AML patients with a false cytological remission at the moment of transplantation. A term of "misleading" cytological remission was used to refer to clinical state with elevated WT1 expression level (higher than 250 copies per 104 copies of reference gene ABL1) combined with normal marrow blast counts (less than 5%). Among 12 such cases, nine patients (75%) did not express BAALC at the levels above the chosen cut-off of 31%, whereas increased BAALC expression was detected in three other patients. Despite limited number of tested AML cases, the RFS and CIR in the latter group appeared to be significantly worse, compared to those with low BAALC expression (р=0.019 и p=0.002, respectively), as seen from Fig. 1.

Figure 1. The difference between RFS (A) and CIR (B) depending on the BAALC gene expression level at the moment of allo-HSCT in the group of patients transplanted in a "misleading" cytological remission
Hence, one may conclude that the patients with combined WT1 and BAALC overexpression could be classified into prognostically unfavorable group, associated with high risk of early post-transplant relapse. This regulatory function seems to be retained in nine patients studied at the moment of transplantation. However, it could be lost in three other patients, in whom a combined WT1 and BAALC overexpression took place.
The BAALC and WT1 expression levels for the previously discussed AML patients [23] were assessed in the context of our recent findings. As shown in Fig. 2, the highest BAALC expression levels were observed in relapsing patients with AML classified as M1 and M2 FAB-variants, with intermediate values in M0, M4 and M5 FAB-variants of AML. The lowest BAALC expression was detected in AML M3 and M7 cases.

Figure 2. Distribution of individual values and median levels of BAALC gene expression in relapsing patients with different AML FAB-variants
In addition, we have studied the BAALC gene expression levels in patients with different cytogenetic AML variants. According to our data, the highest BAALC gene expression levels among cases with favorable cytogenetic changes were observed in the patients with t(8;21) (N=21), and in subgroups with unfavorable karyotype, i.e., aberrations in chromosomes 5 and 7 (N=23), as well as complex karyotype (N=8), and other severe abnormalities (≤2) (N=11, data not shown). In cases of relapse, no statistically significant differences of BAALC gene expression levels were noted between these subgroups.
The patient cohort with higher BAALC gene expression (>31% in relapse) consisted of 30 out of 50 cases (60%), including eight patients with both M1 and M2 FAB- variants of AML. A combined BAALC and WT1 overexpression was observed in 28 cases of 30 (93.3%). The data on two patients with M1 and M2 FAB-variants of AML are shown below (Fig. 3, 4).

Figure 3. Monitoring of BAALC and WT1 mRNA expression levels measured by QR-PCR, and bone marrow blast numbers in a patient with AML M1 (№4)
Note: The values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and during 1 to 3 PTRs were 1.3; 0.15; 1.25; 1.54 for BAALC gene, and 1.05; 0.03; 0.05 and 0.03 for the WT1 gene, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).

Figure 4. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in young patient with AML M2 (№12) measured by QR-PCR of BAALC and WT1 mRNA expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in two PTRs were 0.04; 1.5; 0.47 for gene BAALC and 0.07; 0.24; 0.27 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
As seen from Fig. 2 and Table 2, the BAALC gene expression levels in PTR were higher in patients with AML M1 and M2, and sufficiently lower in AML M4. In order to discuss in details some special interactions between leukemic cell precursors and blast cell populations, determined by means of QR-PCR, we have demonstrated here complete clinical and laboratory characteristics from a larger group of patients with different cytological and cytogenetic AML variants according to FAB criteria. Our study cohort consisted of 22 patients (11 cases for each AML M1 and M2- variants). Twenty one of them had a fully characterized cell karyotype. Simultaneous overexpression of both BAALC and WT1 genes at PTR was detected in four and three AML M1 and M2 cases, respectively (Table 2). As based on these data, the presence of a combined gene overexpression in the patients at post-transplant period is considered an index of unfavorable prognosis.
Table 2. BAALC and WT1 gene expression levels at diagnosis, before allo-HSCT (D0) and at PTRs after hematopoietic stem cell transplantation in the patients with different AML FAB-variants


As seen from Table 2, simultaneous overexpression of BAALC and WT1 genes at relapse at any stage of the disease (at diagnosis, D0 pre-transplant, or PTR) occurred in 28/55 (56%) patients. It was observed in eight patients with AML M1 (72.7%), 8 patients with AML M2 (72.7%), as well as in 1 (33.3%), 8 (50%), 2 (40%) patients with AML M0, M4, and M5, respectively.
To illustrate this concept, several clinical cases of each AML M1, M2 and M4 FAB-variants are represented below (Fig. 3 to 5). The relative ratios of leukemic cell precursors or blast cell burdens were monitored as BAALC and WT1 gene expression levels, respectively, as shown for a patient with AML M1 (Table 2, Fig. 3). In this case No.4, a simultaneous BAALC and WT1 overexpression took place at diagnosis, and at 2nd and 3rd PTRs that occured despite second HSCT and high-dose chemotherapy which was unsuccessful.
In this case, cytogenetic characteristics of leukemic cells were different for the 1st and 2nd relapses. At the first PTR, complex karyotype changes included loss of chromosome X, deletion of 11q and additional chromosome 21 revealed in 15% of tested cells, whereas additional unbalanced translocations t(X;17), t(1;3), and t(1;17) were detected in the second PTR.
In another AML case No. 12 (M2 variant) with t(8;21) translocation (Fig. 4), a simultaneous measurement of BAALC and WT1 gene expression levels revealed overexpression of the WT1 gene at diagnosis, with bone marrow blast burden of up to 28%. Further on, a combined overexpression of both molecular markers was associated with 1st and 2nd relapses, thus being prognostically unfavorable. One may suggest that the disease progression and fatal outcome occurred due to resistance of tumor cells to therapy.
Similar clinical situation was observed in the next patient with AML M4 (No. 31), who received allotransplant at the age of five years. In spite of t(8;21) translocation found at diagnosis, thus classifying the patient into favorable group, an additional deletion 7q – del(7)(q32q36) before transplant allowed, however, to evaluate this case as unfavorable one. The combined BAALC and WT1 overexpression at diagnosis, as well as in first PTR, was accompanied by increased expression level of a specific RUNX1/RUNX1T1 fusion transcript (Fig. 5). Of notice, the blast burden in the bone marrow sample at relapse (D+223) was not too high, wherein hypothetic inhibition of leukemic precursor cells from side of the blast population was minimal, thus explaining higher BAALC gene expression levels observed.

Figure 5. Molecular monitoring of interactions between leukemic cell precursors and blast cells in the patient with AML M4 (№31) measured by QR-PCR of BAALC, WT1 and RUNX1/RUNX1T1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.95; 0.35 for gene BAALC and 0.1; 0.04 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Another clinical case (No. 29) concerns a female patient 21 years old with AML M4 FAB variant (Fig. 6). The first concomitant overexpression of BAALC and WT1 genes has been observed pre-transplant, associated with complex structural chromosomal changes, i.e., monosomy 7, t(2;3) translocation, as well as 3q inversion. All these abnormalities seemed to correlate with a failure to achieve full cytological and molecular remissions. It has been combined with overexpression of both BAALC and WT1 genes during the entire posttransplant period. From this point of view, it is not surprising that the first PTR occurred early on D+80 after transplantation. Prognostically unfavorable simultaneous WT1 and BAALC overexpression, as well as the same clonal changes of karyotype were detected again at that time. The second clinical relapse was detected on the day D+232 posttransplant, when overexpression of the both genes was expressed even more, and a new additional chromosomal abnormality (monosomy 5) was detected on day D+251.

Figure 6. Molecular monitoring of the interaction between leukemic cell precursors and blast cells burdens in patient with AML M4 (№29) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in two PTRs were 1.07; 3.9; 4 for gene BAALC and 0.09; 0.12; 2.6 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Another molecular profile has been revealed during serial measurement of BAALC and WT1 gene expression levels in a 55-year old female patient (Case No. 40, Table 2) with the same AML M4 FAB-variant, but with normal karyotype (Fig. 7). As shown here, the elevated WT1 gene expression level took place not only in pre-transplant relapse, but in early PTR as well, which seems to be a result of transplantation without subsequent cytological remission. At the same time, the BAALC gene overexpression was not observed at neither of relapses. Instead of successful treatment of the first PTR at D+65 after allo-HSCT, the patient developed a new cytological relapse accompanied by the WT1 gene overexpression, and the lethal outcome was detected at D+101 after allo-HSCT.

Figure 7. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in patient with AML M4 (№40) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.035; 0.0006 for gene BAALC and 1.17; 0.1 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
As regards special AML forms, characterized by the absence of BAALC overexpression we observed in 4 (8%) of 50 such cases in our cohort (three among them had AML M3 and one, M7 FAB-variant). Data of the serial parallel measurement of BAALC and WT1 gene expression levels in one of them are represented at Figure 8. Elevated BAALC gene expression level over the cut-off level in a 17-year-old female patient (№ 47) was not observed both at relapse before allo-HSCT, or in posttransplant relapse. At the same time, a significant WT1 gene overexpression took place in both relapses.

Figure 8. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in a 17-years old female patient with AML M3 (№47) measured by QR-PCR of BAALC, WT1 and PML-RARα gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.035; 0.0006 for gene BAALC and 1.17; 0.1 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
In general, the results shown in Fig. 8 may be explained by more differentiated state of promyelocytes providing clinical development of acute promyelocytic leukemia, compared to CD34+/CD38- cell precursors of leukemic hematopoiesis. By this reason, they are unable to express BAALC gene. On the other hand, some, still unknown, immature leukemic cells in M3 FAB- variant AML must have a direct cause higher WT1 gene expression levels which should be studied at regular basis.
It is reasonable to present here some data on parallel measurement of BAALC and WT1 gene expression level in bone marrow samples from a 3-year-old female patient (№49) with AML M7 (Fig. 9). The BAALC gene expression level was under the cut-off value during the entire follow-up period. At the same time, WT1 gene overexpression closely associated with increasing blast burden in bone marrow, was detected during relapse before HSCT, as well as at the posttransplant relapse with pronounced blastosis in bone marrow (>60%).

Figure 9. Molecular monitoring of the interaction between leukemic cell precursors and blast cells in a 3-years old female patient with AML M7 (№49) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 0.0025; 0.0003 for gene BAALC and 0.03; 0.69 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Finally, we would like to demonstrate here some special biological features of blast elements in AML patients, who did not exhibit WT1 gene overexpression. E.g., we present the graphs of molecular monitoring by WT1 and BAALC expression levels in two patients (No. 24 and 26) with M0 AML (Fig. 10) and M4 AML (Fig. 11). The first case presents a 25-year old patient (№24), who had reciprocal translocation t(3;10)(p21;p11) (without EVI1 gene overexpression), and interstitial deletion of chromosome 11 long arm (without MLL gene rearrangements, as shown by FISH technique). According to this graph, the BAALC gene expression level over the cut-off value was detected at relapse before transplantation, as well as at PTR, whereas WT1 gene expression level changes were <250 copies per 104 copies of ABL1 gene during entire period of study. The lethal outcome of the disease on the D+133 after transplantation has been associated with progression.

Figure 10. Molecular monitoring of the interaction between leukemic cell precursors and blast cells in a patient with AML M0 (№24) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in PTR were 1.24; 0.82 for gene BAALC and 0.0003; 0.0005 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
The data from another clinical case are demonstrated in the Figure 11. They relate to a 6-years old patient, who had permanently relapsing disease course and has undergone haploidentical hematopoietic stem cell transplantation in cytological relapse for this reason. In this case, a distinct increase in BAALC expression level has been observed upon relapse before HSCT, as well as at the first PTR on the day D+246. The WT1 expression level at relapse before transplantation and at first PTR was did not exceed the cut-off level. It is equally important that, according to cytogenetic data, this patient has undergone a clonal evolution over the period between diagnosis and first PTR karyotyping associated with its transformation from normal to complex one, including rearrangements of both chromosomes 5, as well as X, 2, 6, 9 and 19. For the first post-transplant relapse, the patient has been treated by polychemotherapy in combination with donor lymphocyte infusion and 5-azacytidin. Such supportive therapy allowed morphological remission for a sufficient period of time. However, the disease progression was detected again on the day D+734 posttransplant, as evidenced by a combined cytological relapse with myelomonocytic blast cells. Their immune profile was as follows: CD34+/CD33+/CD117+/CD13+/CD38+/CD14+ associated with complex clonal rearrangements of chromosomes 2, 5 and 19. It should be noted, that, at the second PTR, this patient had both BAALC and WT1 genes overexpression, what may be explained by hypothetical changes of negative regulation of leukemic precursors by the blast cell burden. Finally, lethal outcome has occurred in this case on the day D+779 post-transplant.

Figure 11. Molecular monitoring of the interaction between leukemic cell precursor and blast cell masses in a 6 years old patient with AML M4 (№26) measured by QR-PCR of BAALC and WT1 gene expression levels
Note: Values of molecular indexes (CNgene/104ABL1) in relapse before allo-HSCT and in the first and second PTRs were 9.8; 71.2; 18.6 for gene BAALC and 0.02; 0.03; 0.21 for gene WT1, respectively. Abscissa, terms of observation pre- and post-transplant, Ordinate, blast numbers (left axis); gene expression (right axis).
Discussion
The data presented here show an opportunity for simultaneous BAALC and WT1 gene overexpression in a group of AML patients with increased levels of WT1 and normalized up to 4% number of blasts in bone marrow samples. Therefore, it could be considered a strong indicator of poor prognosis in these cases. On the other hand, the levels of BAALC and WT1 levels expression determined by means of PCR may reflect, in a quantitative manner, the relative sizes of precursor and blast cell burden. Of note, hypothetical correlation between these tumor compartments has not elucidated yet, and may be not obligatory for all AML cases. The study has shown that the absence of BAALC overexpression at transplantation was associated with lower CIR in 9 of 12 patients (75%) with abovementioned intermediate clinical status. On the contrary, the 3 other patients with elevated BAALC expression before transplant revealed earlier PTR development associated with shorter 2-year OS and EFS, as compared with the main group of patients. Hence, an assumption was made that simultaneous overexpression of BAALC and WT1 may be a useful indicator of dismal post-transplant AML course. Keeping this in mind, we showed a double overexpression phenomenon to be present in four patients with M1 (N=2), M2 (n=1) and M4 (n=1) AML variants associated with poor prognosis. Further on, our data showed the levels of BAALC expression to be similarly high in patients with immature and mature M1 and M2 FAB-variants, respectively. On the other hand, the lowest BAALC expression levels were noticed in patients with M3 and M7 AML FAB- variants. Today, the absence of BAALC gene expression in patients with acute promyelocytic leukemia may be explained by its origin from more “mature” cell populations than the standard CD34+CD38– precursors producing BAALC [25]. The same situation seems exist in the M7 FAB variants of AML, which also needs a similar additional study.
In our opinion, the results of BAALC gene expression measurement in patients with M2 and M4 FAB-variants are interesting in several regards. Firstly, high expression of BAALC and WT1 genes were synchronous in most cases. At the same time, the numbers of blast elements in their bone marrow aspirates increased to lower degree than expected. The simplest explanation for this discordance between findings in AML variants and cell maturity may be that these blast elements can differentiate only partially and, therefore, transform into more mature cellular populations. However, due to decreased size of blast population preserved in this kind of AML, some hypothetical regulating mechanisms can be activated for additional recruitment of new portions of CD34+CD38- precursors into leukemic hematopoiesis. Due to mentioned transition of blast elements to the more mature hematopoietic compartments, as well as their hypothetical regulator mechanism between blast burden and leukemic precursor compartment, the revealed similarity in gene BAALC overexpression for M2 and M4 FAB- variants of AML, and those in M1 and M0 FAB variants may be explained in these terms.
In conclusion, it should be like to notice, that clinical significance of our findings, concerning simultaneous overexpression of BAALC and WT1 genes in adults and children with AML treated with allo-HSCT, and/or donor lymphocyte infusions was presented for the first time and could be effectively used for clinical diagnostics and prediction of relapses in AML patients. The combined WT1 and BAALC overexpression was studied in relatively small group of patients, thus requiring further confirmation in larger groups of patients with different FAB variants of AML.
Conflict of interest
No conflict of interests is declared.
References
- Tanner S, Austin J, Leone G, Rush L, Plass C, Heinonen K, Mrózek K, Still H, Knuutila S, Kolitz J, Archer K, Caligiuri M, Bloomfield C, de la Chapelle A. BAALC, the human member of a novel mammalian neuroectoderm gene lineage, is implicated in hematopoiesis and acute leukemia. Proc Natl Acad Sci USA. 2001;98(24):13901-13906.
- Santamaría C, Chillón M, García-Sanz R, Pérez C, Caballero M, Mateos M, Ramos F, de Coca A, Alonso J, Giraldo P, Bernal T, Queizán J, Rodríguez J, Puig N, Balanzategui A, Sarasquete M, Alcoceba M, Díaz-Mediavilla J, San Miguel J, González M. BAALC is an important predictor of refractoriness to chemotherapy and poor survival in intermediate-risk acute myeloid leukemia (AML). Ann Hematol. 2010;89:453-458.
- Weber S, Haferlach T, Alpermann T, Perglerová K, Schnittger S, Haferlach C, Kern W. Feasibility of BAALC gene expression for detection of minimal residual disease and risk stratification in normal karyotype acute myeloid leukemia. Br J Haematol. 2016;175(5):904-916.
- Jentzsch M, Bill M, Grimm J, Schulz J, Goldmann K, Beinicke S, Häntschel J, Pönish W, Franke G-N, Vicinic V, Behre G, Lange T, Niederwiesser D, Schwind S. High BAALC copy numbers in peripheral blood prior to allogeneic transplantation predict early relapse in acute myeloid leukemia. Oncotarget. 2017;8(50):87994-97954.
- Yoon J, Kim H, Shin S, Yahng S, Lee S, Cho S, Eom K, Kim Y, Lee S, Min C, Cho S, Kim D, Lee J, Min W, Park C, Lim J. BAALC and WT1 expressions from diagnosis to hematopoietic stem cell transplantation: consecutive monitoring in adult patients with core-binding–factor-positive AML. Europ J Haematol. 2013;91:112-127.
- Xiao S, Shen J, Huang J, Fu H. Prognostic significance of the BAALC gene expression in adult patients with acute myeloid leukemia: A meta-analysis. Mol Clin Oncol. 2015;3(4):880-888.
- Hecht A, Doll S, Altmann H, Nowak D, Lengfelder E, Röllig C, Ehninger G, Spiekermann K, Hiddemann W, Weiß C, Hofmann W, Nolte F, Platzbecker U. Validation of a molecular risk score for prognosis of patients with acute promyelocytic leukemia treated with all-trans retinoic acid and chemotherapy-containing regimens. Clin Lymphoma Myeloma Leuk. 2017; 17(12):889-896.e5.
- Staffas A, Kanduri M, Hovland R, Rosenquist R, Ommen HB, Abrahamsson J, Forestier E, Jahnukainen K, Jónsson ÓG, Zeller B, Palle J, Lönnerholm G, Hasle H, Palmqvist L, Ehrencrona H; Nordic Society of Pediatric Hematology and Oncology (NOPHO). Presence of FLT3-ITD and high BAALC expression are independent prognostic markers in childhood acute myeloid leukemia. Blood. 2011 Nov 24;118(22):5905-13.
- Najima Y, Ohashi K, Kawamura M, Onozuka Y, Yamaguchi T, Akiyama H, et al. Molecular monitoring of BAALC expression in patients with CD34-positive acute leukemia. Int J Hematol. 2010;91:636–645.
- Damiani D, Tiribelli M, Franzoni A, Michelutti A, Fabbro D, Cavallin M, Toffoletti E, Simeone E, Fanin R, Damante G. BAALC overexpression retains its negative prognostic role across all cytogenetic risk groups in acute myeloid leukemia patients. Am J Hematol. 2013;88(10):848-852.
- Pogosova-Agadjanyan E, Moseley A, Othus M, Appelbaum F, Chauncey T, Chen I, Erba H, Godwin J, Fang M, Kopecky K, List A, Pogosov G, Radich J, Willman C, Wood B, Meshinchi S, Stirewalt D. Impact of specimen heterogeneity on biomarkers in repository samples from patients with acute myeloid leukemia: A SWOG report. Biopreserv Biobank. 2018;16(1):42-52.
- Morita K, Masamoto Y, Kataoka K, Koya J, Kagoya Y, Yashiroda H, Sato T, Murata S, Kurokawa M. BAALC potentiates oncogenic ERK pathway through interactions with MEKK1 and KLF4. Leukemia. 2015;29(11):2248-2456.
- Costello R, Mallet F, Gaugler B, Sainty D, Arnoulet C, Gastaut J, Olive D. Human acute myeloid leukemia CD34+/CD38- progenitor cells have decreased sensitivity to chemotherapy and Fas-induced apoptosis? Reduced immunogenicity, and impaired dendritic cell transformation capacities. Cancer Res. 2000;60:4403-4411.
- Gerber J, Smith B, Ngwang B, Zhang H, Vala M, Morsberger L, Galkin S, Collector M, Perkins B, Levis M, et al. A clinically relevant population of leukemic CD34+CD38- cells in acute myeloid leukemia. Blood. 2012;119(15):3571-3577.
- Gerber J, Zeidner J, Morse S, Blackford A, Perkins B, Yanagisawa B, Zhang H, Morsberger L, Karp J, Ning Y, Cocke C, Rosner G, Smith D, Jones R. Association of acute myeloid leukemia’s most immature phenotype with risk groups and outcomes. Haematologica. 2016;101950;607-615.
- Jentzsch M, Bill M, Nicolet D, Leiblein S, Schubert K, Pless M, Bergmann U, Wildenberger K, Schuhmann L, Cross M, et al. Prognostic impact of the CD34+/CD38- cell burden in patients with acute myeloid leukemia receiviung allogeneic stem cell transplantation. Am J Hematol. 2017;92(4):388-396.
- Plesa A, Dumontet C, Mattei E, Tagoug I, Hayette S, Sujobert P, Tigaud I, Pages M, Chelghome Y, Baracco F, et al. High frequqncy of CD34+CD38-/low immature leukemia cells is correlated with unfavorable prognosis in acute leukemia. World J Stem Cells. 2017;9(12):227-234.
- Thomas D, Majeti R. Biology and relevance of human acute myeloid leukemia stem cells. Blood. 2017;129(12):1577–1585.
- Mamaev N, Gudozhnikova Y, Gindina T, Barkhatov I, Shakirova A, Katerina V, Gubina M, Nikolaeva E, Semenova E, Paina O, Darskaya E, Pirogova O, Porunova V, Moiseev I, Mikhailova I, Ayubova B, Kravtsova V, Bondarenko S, Zubarovskaya L, Afanasyev B. Efficacy of Chemotherapy in Acute Leukemia Patients Resistant to Previous Standard Treatment According to the Series Measurement of WT1 Gene Expression. Clinical Oncohematology. 2018;11(1):78-88 (In Russian).
- Minetto P, Guolo F, Clavio M, de Astis E, Colombo N, Grasso R, Fugazza G, Sessarego M, Lemoli R, Gobbi M, Miglino M. Combined assessment of WT1 and BAALC gene expression at diagnosis may improve leukemia-free survival prediction in patients with myelodysplastic syndromes. Leukemia Res. 2015;39:866-873.
- Haferlach C, Kern W, Schindela S, Kohlmann A, Alpermann T, Schnittger S, Haferlach T. Gene expression of BAALC, CDKN1B, ERG, and MN1 adds independent prognostic information to cytogenetics and molecular mutations in adult acute myeloid leukemia. Genes Chromosomes Cancer. 2012;51(3):257-265.
- Gudozhnikova Y, Mamaev N, Barkhatov I, Katerina V, Gindina T, Shakirova A, Bondarenko S, Slesarchuk O, Darskaya E, Paina O, Zubarovskaya L, Afanasyev B. Results of Molecular Monitoring in Post-transplant Period by Means of Series Investigation of WT1 Gene Expression in Patients with Acute Myeloid Leukemia. Clinical Oncohematology. 2018;11(3):241-251 (In Russian).
- Shakirova A, Barkhatov I, Churkina A, Moiseev I, Gindina T, Bondarenko S, Afanasyev B. Prognostic significance of BAALC overexpression in patients with AML during the post-transplant period. Cell Ther Transplant. 2018;7(2):54-63.
- Cilloni D, Renneville A, Hermitte F, Hills R, Daly S, Jovanovic J, Gottardi E, Fava M, Schnittger S, Weiss T, Izzo B, Nomdedeu J, van der Heijden A, van der Reijden B, Jansen J, van der Velden V, Ommen H, Preudhomme C, Saglio G, Grimwade D. Real-time quantitative polymerase chain reaction detection of minimal residual disease by standardized WT1 assay to enhance risk stratification in acute myeloid leukemia: a European LeukemiaNet study. J Clin Oncol. 2009;27(31):5195-5201.
- Reinisch A, Thomas D, Corces MR, et al. A humanized bone marrow ossicle xenotransplantation model enables improved engraftment of healthy and leukemic human hematopoietic cells. Nat Med. 2016;22(7):812-821.
Алена И. Шакирова, Николай Н. Мамаев, Ильдар М. Бархатов, Яна В. Гудожникова, Татьяна Л. Гиндина, Елена В. Бабенко, Борис В. Афанасьев
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22272" ["VALUE"]=> array(2) { ["TEXT"]=> string(459) "<p>НИИ детской онкологии, гематологии и трансплантации им. Р. М. Горбачевой; кафедра гематологии, трансфузиологии и трансплантологии Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(447) "НИИ детской онкологии, гематологии и трансплантации им. Р. М. Горбачевой; кафедра гематологии, трансфузиологии и трансплантологии Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова, Санкт-Петербург, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_RU"]=> array(36) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22273" ["VALUE"]=> array(2) { ["TEXT"]=> string(4819) "<p style="text-align: justify;">Цель изучения состояла в выяснении тесных связей между популяциями костномозговых бластных элементов, повышение содержания которых определяет цитологический рецидив ОМЛ, и ответственных за рецидив лейкозных клеток предшественников. В клиническом плане, мы имели целью оценку потенциала развития рецидивов лейкоза после трансплантации гемопоэтических клеток (ТГСК). Посттрансплантационные рецидивы (ПТР), с точки зрения их биологических механизмов, могут выявляться по гиперэкспрессии определенных генов, связанных с клеточной дифференцировкой.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">В исследование вошло 61 больных ОМЛ, леченных с помощью алло-ТГСК, у которых осуществлено одновременное серийное измерение уровней экспрессии генов <i>BAALC</i> и <i>WT1</i> методом количественной ПЦР в реальном времени с использованием ген-специфических праймеров.</p> <h3>Результаты</h3> <p style="text-align: justify;">В группе из 12 больных с повышенным уровнем экспрессии гена <i>WT1</i> и с нормализованным до 4 % содержанием бластных элементов в костном мозге на момент проведения аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК) было показано, что подгруппа с повышенной экспрессией гена <i>BAALC</i> характеризуется: а) более высоким числом ПТР (р=0,002); а также б) укорочением сроков безрецидивной выживаемости (БРВ) при сопоставлении с группой сравнения (р=0,019). Дальнейшее использование этого прогностически неблагоприятного критерия, состоящего из одновременного повышения уровней экспрессии обоих генов при анализе основного массива данных, показало его более частое обнаружение у больных с М1, М2, М0, М4 и М5 ФАБ- цитологическими вариантами. При этом предварительные данные указывают на худшую общую выживаемость (228 дней) в группе больных ОМЛ, имевших сочетанную гиперэкспрессию обоих генов как непосредственно перед ТГСК, так и в посттрансплантационном периоде. </p> <h3>Заключение</h3> <p style="text-align: justify;">Потенциальная клиническая значимость полученных данных, касающихся повышенной экспрессии гена <i>BAALC</i> у взрослых и детей больных ОМЛ, леченных с использованием алло-ТГСК, и особенно, наличия феномена сочетания у них гиперэкспрессии генов <i>BAALC</i> и <i>WT1</i> несомненна, что диктует необходимость активного использования их в клинике. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Острый миелоидный лейкоз, аллогенная трансплантация гемопоэтических клеток, посттрансплантационные рецидивы, гены <i>BAALC</i> и <i>WT1</i>, одновременная гиперэкспрессия, клиническая значимость, прогноз.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(4553) "Цель изучения состояла в выяснении тесных связей между популяциями костномозговых бластных элементов, повышение содержания которых определяет цитологический рецидив ОМЛ, и ответственных за рецидив лейкозных клеток предшественников. В клиническом плане, мы имели целью оценку потенциала развития рецидивов лейкоза после трансплантации гемопоэтических клеток (ТГСК). Посттрансплантационные рецидивы (ПТР), с точки зрения их биологических механизмов, могут выявляться по гиперэкспрессии определенных генов, связанных с клеточной дифференцировкой.
Пациенты и методы
В исследование вошло 61 больных ОМЛ, леченных с помощью алло-ТГСК, у которых осуществлено одновременное серийное измерение уровней экспрессии генов BAALC и WT1 методом количественной ПЦР в реальном времени с использованием ген-специфических праймеров.
Результаты
В группе из 12 больных с повышенным уровнем экспрессии гена WT1 и с нормализованным до 4 % содержанием бластных элементов в костном мозге на момент проведения аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК) было показано, что подгруппа с повышенной экспрессией гена BAALC характеризуется: а) более высоким числом ПТР (р=0,002); а также б) укорочением сроков безрецидивной выживаемости (БРВ) при сопоставлении с группой сравнения (р=0,019). Дальнейшее использование этого прогностически неблагоприятного критерия, состоящего из одновременного повышения уровней экспрессии обоих генов при анализе основного массива данных, показало его более частое обнаружение у больных с М1, М2, М0, М4 и М5 ФАБ- цитологическими вариантами. При этом предварительные данные указывают на худшую общую выживаемость (228 дней) в группе больных ОМЛ, имевших сочетанную гиперэкспрессию обоих генов как непосредственно перед ТГСК, так и в посттрансплантационном периоде.
Заключение
Потенциальная клиническая значимость полученных данных, касающихся повышенной экспрессии гена BAALC у взрослых и детей больных ОМЛ, леченных с использованием алло-ТГСК, и особенно, наличия феномена сочетания у них гиперэкспрессии генов BAALC и WT1 несомненна, что диктует необходимость активного использования их в клинике.
Ключевые слова
Острый миелоидный лейкоз, аллогенная трансплантация гемопоэтических клеток, посттрансплантационные рецидивы, гены BAALC и WT1, одновременная гиперэкспрессия, клиническая значимость, прогноз.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22265" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-45-57" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-45-57" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22267" ["VALUE"]=> array(2) { ["TEXT"]=> string(171) "<p> Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko, <br>Boris V. Afanasyev </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(153) "
Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko,
Boris V. Afanasyev
Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22277" ["VALUE"]=> array(2) { ["TEXT"]=> string(2859) "<p style="text-align: justify;">The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of <i>WT1</i> and <i>BAALC</i> molecular markers expressed by appropriate cell types. In clinical terms, we sought to evaluate a potential for evolving leukemia relapses following hematopoietic stem cell transplantation (HSCT). The post-transplant relapses (PTR), in view of their biological mechanisms, may be detected by overexpression of distinct differentiation-related genes.</p> <h3>Patients and methods</h3> <p style="text-align: justify;">We have done parallel serial measurements of <i>BAALC</i> and <i>WT1</i> gene expression in bone marrow cells of the patients with acute myeloid leukemia, using quantitative real-time PCR (qPCR) with gene-specific primers.</p> <h3>Results</h3> <p style="text-align: justify;">An initial pilot study was carried out in twelve patients with elevated <i>WT1</i> expression levels and normal blast counts (<5%) in bone marrow at the time of allogeneic HSCT. It has shown that the relapse occurrence and shorter relapse-free survival (RFS) post-transplant were more common in the subgroup with higher <i>BAALC</i> gene expression level as compared to those without <i>BAALC</i> expression elevation (p=0.002, and p=0.019, respectively). Moreover, when analyzing the validating patient cohort, we have found that the simultaneous elevation of both <i>BAALC</i> and <i>WT1</i> expression, known as unfavorable prognostic factor, was more frequently observed in the patients with AML М1, М2, and М0 FAB-variants. Preliminary results show an inferior overall survival (a mean of 228 days) in AML patients with combined overexpression of the both genes immediately before HSCT, like as in post-transplant period. In conclusion, it should be noted that our findings of simultaneous overexpressions of <i>BAALC</i> and <i>WT1</i> genes in great cohort of adults and children patients with different FAB- variants of AML treated by means of allo-HSCT were revealed for the first time. Being associated with poor prognosis, this double test should be used actively for post-transplant monitoring of all patients with AML. </p> <h2>Keywords</h2> <p style="text-align: justify;">Acute myeloblastic leukemia, hematopoietic stem cell transplantation, allogeneic, post-transplant relapses, <i>BAALC</i>, <i>WT1</i>, gene overexpression, parallel assays, relapse risk, prognostic value. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2576) "The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of WT1 and BAALC molecular markers expressed by appropriate cell types. In clinical terms, we sought to evaluate a potential for evolving leukemia relapses following hematopoietic stem cell transplantation (HSCT). The post-transplant relapses (PTR), in view of their biological mechanisms, may be detected by overexpression of distinct differentiation-related genes.
Patients and methods
We have done parallel serial measurements of BAALC and WT1 gene expression in bone marrow cells of the patients with acute myeloid leukemia, using quantitative real-time PCR (qPCR) with gene-specific primers.
Results
An initial pilot study was carried out in twelve patients with elevated WT1 expression levels and normal blast counts (<5%) in bone marrow at the time of allogeneic HSCT. It has shown that the relapse occurrence and shorter relapse-free survival (RFS) post-transplant were more common in the subgroup with higher BAALC gene expression level as compared to those without BAALC expression elevation (p=0.002, and p=0.019, respectively). Moreover, when analyzing the validating patient cohort, we have found that the simultaneous elevation of both BAALC and WT1 expression, known as unfavorable prognostic factor, was more frequently observed in the patients with AML М1, М2, and М0 FAB-variants. Preliminary results show an inferior overall survival (a mean of 228 days) in AML patients with combined overexpression of the both genes immediately before HSCT, like as in post-transplant period. In conclusion, it should be noted that our findings of simultaneous overexpressions of BAALC and WT1 genes in great cohort of adults and children patients with different FAB- variants of AML treated by means of allo-HSCT were revealed for the first time. Being associated with poor prognosis, this double test should be used actively for post-transplant monitoring of all patients with AML.
Keywords
Acute myeloblastic leukemia, hematopoietic stem cell transplantation, allogeneic, post-transplant relapses, BAALC, WT1, gene overexpression, parallel assays, relapse risk, prognostic value.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22266" ["VALUE"]=> string(111) "Clinical significance of BAALC overexpression for predicting post-transplant relapses in acute myeloid leukemia" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(111) "Clinical significance of BAALC overexpression for predicting post-transplant relapses in acute myeloid leukemia" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22274" ["VALUE"]=> string(4) "1628" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1628" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22275" ["VALUE"]=> string(4) "1629" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1629" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(11) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22267" ["VALUE"]=> array(2) { ["TEXT"]=> string(171) "<p> Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko, <br>Boris V. Afanasyev </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(153) "
Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko,
Boris V. Afanasyev
Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko,
Boris V. Afanasyev
The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of WT1 and BAALC molecular markers expressed by appropriate cell types. In clinical terms, we sought to evaluate a potential for evolving leukemia relapses following hematopoietic stem cell transplantation (HSCT). The post-transplant relapses (PTR), in view of their biological mechanisms, may be detected by overexpression of distinct differentiation-related genes.
Patients and methods
We have done parallel serial measurements of BAALC and WT1 gene expression in bone marrow cells of the patients with acute myeloid leukemia, using quantitative real-time PCR (qPCR) with gene-specific primers.
Results
An initial pilot study was carried out in twelve patients with elevated WT1 expression levels and normal blast counts (<5%) in bone marrow at the time of allogeneic HSCT. It has shown that the relapse occurrence and shorter relapse-free survival (RFS) post-transplant were more common in the subgroup with higher BAALC gene expression level as compared to those without BAALC expression elevation (p=0.002, and p=0.019, respectively). Moreover, when analyzing the validating patient cohort, we have found that the simultaneous elevation of both BAALC and WT1 expression, known as unfavorable prognostic factor, was more frequently observed in the patients with AML М1, М2, and М0 FAB-variants. Preliminary results show an inferior overall survival (a mean of 228 days) in AML patients with combined overexpression of the both genes immediately before HSCT, like as in post-transplant period. In conclusion, it should be noted that our findings of simultaneous overexpressions of BAALC and WT1 genes in great cohort of adults and children patients with different FAB- variants of AML treated by means of allo-HSCT were revealed for the first time. Being associated with poor prognosis, this double test should be used actively for post-transplant monitoring of all patients with AML.
Keywords
Acute myeloblastic leukemia, hematopoietic stem cell transplantation, allogeneic, post-transplant relapses, BAALC, WT1, gene overexpression, parallel assays, relapse risk, prognostic value.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(2576) "The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of WT1 and BAALC molecular markers expressed by appropriate cell types. In clinical terms, we sought to evaluate a potential for evolving leukemia relapses following hematopoietic stem cell transplantation (HSCT). The post-transplant relapses (PTR), in view of their biological mechanisms, may be detected by overexpression of distinct differentiation-related genes.
Patients and methods
We have done parallel serial measurements of BAALC and WT1 gene expression in bone marrow cells of the patients with acute myeloid leukemia, using quantitative real-time PCR (qPCR) with gene-specific primers.
Results
An initial pilot study was carried out in twelve patients with elevated WT1 expression levels and normal blast counts (<5%) in bone marrow at the time of allogeneic HSCT. It has shown that the relapse occurrence and shorter relapse-free survival (RFS) post-transplant were more common in the subgroup with higher BAALC gene expression level as compared to those without BAALC expression elevation (p=0.002, and p=0.019, respectively). Moreover, when analyzing the validating patient cohort, we have found that the simultaneous elevation of both BAALC and WT1 expression, known as unfavorable prognostic factor, was more frequently observed in the patients with AML М1, М2, and М0 FAB-variants. Preliminary results show an inferior overall survival (a mean of 228 days) in AML patients with combined overexpression of the both genes immediately before HSCT, like as in post-transplant period. In conclusion, it should be noted that our findings of simultaneous overexpressions of BAALC and WT1 genes in great cohort of adults and children patients with different FAB- variants of AML treated by means of allo-HSCT were revealed for the first time. Being associated with poor prognosis, this double test should be used actively for post-transplant monitoring of all patients with AML.
Keywords
Acute myeloblastic leukemia, hematopoietic stem cell transplantation, allogeneic, post-transplant relapses, BAALC, WT1, gene overexpression, parallel assays, relapse risk, prognostic value.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22265" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-45-57" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-45-57" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-45-57" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22266" ["VALUE"]=> string(111) "Clinical significance of BAALC overexpression for predicting post-transplant relapses in acute myeloid leukemia" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(111) "Clinical significance of BAALC overexpression for predicting post-transplant relapses in acute myeloid leukemia" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(111) "Clinical significance of BAALC overexpression for predicting post-transplant relapses in acute myeloid leukemia" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22276" ["VALUE"]=> array(2) { ["TEXT"]=> string(197) "<p>Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(185) "Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(185) "Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22271" ["VALUE"]=> array(2) { ["TEXT"]=> string(255) "<p>Алена И. Шакирова, Николай Н. Мамаев, Ильдар М. Бархатов, Яна В. Гудожникова, Татьяна Л. Гиндина, Елена В. Бабенко, Борис В. Афанасьев</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(243) "Алена И. Шакирова, Николай Н. Мамаев, Ильдар М. Бархатов, Яна В. Гудожникова, Татьяна Л. Гиндина, Елена В. Бабенко, Борис В. Афанасьев
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(243) "Алена И. Шакирова, Николай Н. Мамаев, Ильдар М. Бархатов, Яна В. Гудожникова, Татьяна Л. Гиндина, Елена В. Бабенко, Борис В. Афанасьев
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22255" ["VALUE"]=> string(22) "05/08/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "05/08/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "05/08/2019 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22256" ["VALUE"]=> string(22) "06/28/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "06/28/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "06/28/2019 12:00:00 am" } ["CONTACT"]=> array(38) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22257" ["VALUE"]=> string(3) "361" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(3) "361" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(61) "Alena I. Shakirova" ["LINK_ELEMENT_VALUE"]=> bool(false) } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22273" ["VALUE"]=> array(2) { ["TEXT"]=> string(4819) "<p style="text-align: justify;">Цель изучения состояла в выяснении тесных связей между популяциями костномозговых бластных элементов, повышение содержания которых определяет цитологический рецидив ОМЛ, и ответственных за рецидив лейкозных клеток предшественников. В клиническом плане, мы имели целью оценку потенциала развития рецидивов лейкоза после трансплантации гемопоэтических клеток (ТГСК). Посттрансплантационные рецидивы (ПТР), с точки зрения их биологических механизмов, могут выявляться по гиперэкспрессии определенных генов, связанных с клеточной дифференцировкой.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">В исследование вошло 61 больных ОМЛ, леченных с помощью алло-ТГСК, у которых осуществлено одновременное серийное измерение уровней экспрессии генов <i>BAALC</i> и <i>WT1</i> методом количественной ПЦР в реальном времени с использованием ген-специфических праймеров.</p> <h3>Результаты</h3> <p style="text-align: justify;">В группе из 12 больных с повышенным уровнем экспрессии гена <i>WT1</i> и с нормализованным до 4 % содержанием бластных элементов в костном мозге на момент проведения аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК) было показано, что подгруппа с повышенной экспрессией гена <i>BAALC</i> характеризуется: а) более высоким числом ПТР (р=0,002); а также б) укорочением сроков безрецидивной выживаемости (БРВ) при сопоставлении с группой сравнения (р=0,019). Дальнейшее использование этого прогностически неблагоприятного критерия, состоящего из одновременного повышения уровней экспрессии обоих генов при анализе основного массива данных, показало его более частое обнаружение у больных с М1, М2, М0, М4 и М5 ФАБ- цитологическими вариантами. При этом предварительные данные указывают на худшую общую выживаемость (228 дней) в группе больных ОМЛ, имевших сочетанную гиперэкспрессию обоих генов как непосредственно перед ТГСК, так и в посттрансплантационном периоде. </p> <h3>Заключение</h3> <p style="text-align: justify;">Потенциальная клиническая значимость полученных данных, касающихся повышенной экспрессии гена <i>BAALC</i> у взрослых и детей больных ОМЛ, леченных с использованием алло-ТГСК, и особенно, наличия феномена сочетания у них гиперэкспрессии генов <i>BAALC</i> и <i>WT1</i> несомненна, что диктует необходимость активного использования их в клинике. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Острый миелоидный лейкоз, аллогенная трансплантация гемопоэтических клеток, посттрансплантационные рецидивы, гены <i>BAALC</i> и <i>WT1</i>, одновременная гиперэкспрессия, клиническая значимость, прогноз.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(4553) "Цель изучения состояла в выяснении тесных связей между популяциями костномозговых бластных элементов, повышение содержания которых определяет цитологический рецидив ОМЛ, и ответственных за рецидив лейкозных клеток предшественников. В клиническом плане, мы имели целью оценку потенциала развития рецидивов лейкоза после трансплантации гемопоэтических клеток (ТГСК). Посттрансплантационные рецидивы (ПТР), с точки зрения их биологических механизмов, могут выявляться по гиперэкспрессии определенных генов, связанных с клеточной дифференцировкой.
Пациенты и методы
В исследование вошло 61 больных ОМЛ, леченных с помощью алло-ТГСК, у которых осуществлено одновременное серийное измерение уровней экспрессии генов BAALC и WT1 методом количественной ПЦР в реальном времени с использованием ген-специфических праймеров.
Результаты
В группе из 12 больных с повышенным уровнем экспрессии гена WT1 и с нормализованным до 4 % содержанием бластных элементов в костном мозге на момент проведения аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК) было показано, что подгруппа с повышенной экспрессией гена BAALC характеризуется: а) более высоким числом ПТР (р=0,002); а также б) укорочением сроков безрецидивной выживаемости (БРВ) при сопоставлении с группой сравнения (р=0,019). Дальнейшее использование этого прогностически неблагоприятного критерия, состоящего из одновременного повышения уровней экспрессии обоих генов при анализе основного массива данных, показало его более частое обнаружение у больных с М1, М2, М0, М4 и М5 ФАБ- цитологическими вариантами. При этом предварительные данные указывают на худшую общую выживаемость (228 дней) в группе больных ОМЛ, имевших сочетанную гиперэкспрессию обоих генов как непосредственно перед ТГСК, так и в посттрансплантационном периоде.
Заключение
Потенциальная клиническая значимость полученных данных, касающихся повышенной экспрессии гена BAALC у взрослых и детей больных ОМЛ, леченных с использованием алло-ТГСК, и особенно, наличия феномена сочетания у них гиперэкспрессии генов BAALC и WT1 несомненна, что диктует необходимость активного использования их в клинике.
Ключевые слова
Острый миелоидный лейкоз, аллогенная трансплантация гемопоэтических клеток, посттрансплантационные рецидивы, гены BAALC и WT1, одновременная гиперэкспрессия, клиническая значимость, прогноз.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(4553) "Цель изучения состояла в выяснении тесных связей между популяциями костномозговых бластных элементов, повышение содержания которых определяет цитологический рецидив ОМЛ, и ответственных за рецидив лейкозных клеток предшественников. В клиническом плане, мы имели целью оценку потенциала развития рецидивов лейкоза после трансплантации гемопоэтических клеток (ТГСК). Посттрансплантационные рецидивы (ПТР), с точки зрения их биологических механизмов, могут выявляться по гиперэкспрессии определенных генов, связанных с клеточной дифференцировкой.
Пациенты и методы
В исследование вошло 61 больных ОМЛ, леченных с помощью алло-ТГСК, у которых осуществлено одновременное серийное измерение уровней экспрессии генов BAALC и WT1 методом количественной ПЦР в реальном времени с использованием ген-специфических праймеров.
Результаты
В группе из 12 больных с повышенным уровнем экспрессии гена WT1 и с нормализованным до 4 % содержанием бластных элементов в костном мозге на момент проведения аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК) было показано, что подгруппа с повышенной экспрессией гена BAALC характеризуется: а) более высоким числом ПТР (р=0,002); а также б) укорочением сроков безрецидивной выживаемости (БРВ) при сопоставлении с группой сравнения (р=0,019). Дальнейшее использование этого прогностически неблагоприятного критерия, состоящего из одновременного повышения уровней экспрессии обоих генов при анализе основного массива данных, показало его более частое обнаружение у больных с М1, М2, М0, М4 и М5 ФАБ- цитологическими вариантами. При этом предварительные данные указывают на худшую общую выживаемость (228 дней) в группе больных ОМЛ, имевших сочетанную гиперэкспрессию обоих генов как непосредственно перед ТГСК, так и в посттрансплантационном периоде.
Заключение
Потенциальная клиническая значимость полученных данных, касающихся повышенной экспрессии гена BAALC у взрослых и детей больных ОМЛ, леченных с использованием алло-ТГСК, и особенно, наличия феномена сочетания у них гиперэкспрессии генов BAALC и WT1 несомненна, что диктует необходимость активного использования их в клинике.
Ключевые слова
Острый миелоидный лейкоз, аллогенная трансплантация гемопоэтических клеток, посттрансплантационные рецидивы, гены BAALC и WT1, одновременная гиперэкспрессия, клиническая значимость, прогноз.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22272" ["VALUE"]=> array(2) { ["TEXT"]=> string(459) "<p>НИИ детской онкологии, гематологии и трансплантации им. Р. М. Горбачевой; кафедра гематологии, трансфузиологии и трансплантологии Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(447) "НИИ детской онкологии, гематологии и трансплантации им. Р. М. Горбачевой; кафедра гематологии, трансфузиологии и трансплантологии Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова, Санкт-Петербург, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(447) "НИИ детской онкологии, гематологии и трансплантации им. Р. М. Горбачевой; кафедра гематологии, трансфузиологии и трансплантологии Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова, Санкт-Петербург, Россия
" } } } [4]=> array(49) { ["IBLOCK_SECTION_ID"]=> string(3) "126" ["~IBLOCK_SECTION_ID"]=> string(3) "126" ["ID"]=> string(4) "1661" ["~ID"]=> string(4) "1661" ["IBLOCK_ID"]=> string(1) "2" ["~IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(193) "Эффективность клеточной терапии язвенного колита по данным морфологии слизистой оболочки толстой кишки" ["~NAME"]=> string(193) "Эффективность клеточной терапии язвенного колита по данным морфологии слизистой оболочки толстой кишки" ["ACTIVE_FROM"]=> NULL ["~ACTIVE_FROM"]=> NULL ["TIMESTAMP_X"]=> string(22) "09/29/2019 03:49:58 pm" ["~TIMESTAMP_X"]=> string(22) "09/29/2019 03:49:58 pm" ["DETAIL_PAGE_URL"]=> string(154) "/en/archive/tom-8-nomer-2/klinicheskie-issledovaniya/efficiency-of-mesenchymal-stem-cell-therapy-in-ulcerative-colitis-as-assessed-by-the-morphology-of-c/" ["~DETAIL_PAGE_URL"]=> string(154) "/en/archive/tom-8-nomer-2/klinicheskie-issledovaniya/efficiency-of-mesenchymal-stem-cell-therapy-in-ulcerative-colitis-as-assessed-by-the-morphology-of-c/" ["LIST_PAGE_URL"]=> string(12) "/en/archive/" ["~LIST_PAGE_URL"]=> string(12) "/en/archive/" ["DETAIL_TEXT"]=> string(15705) "Introduction
Modern therapy of inflammatory bowel disease takes into account the complex multifactorial pathogenetic mechanisms of development of this pathology [1, 2]. In view of the immunocorrective and immunosuppressive properties of mesenchymal stem cells, it is important to study the effectiveness of cellular therapy for patients with ulcerative colitis (UC). Immune component of pathogenesis in these immunological disorders is of sufficient importance. The inclusion of mesenchymal stromal cell transplantation in anticytokine and immunosuppressive therapy in patients with ulcerative colitis and Crohn's disease contributed to the positive dynamics of the clinical remission of these diseases [3]. However, morphological changes in large intestine mucosa (LIM) following cell therapy are still poorly understood from the standpoint of the “stem cell niche” and the mechanisms of participation of mesenchymal stem cells (MSCs) in the regulation of regenerative processes. Histological assessment of the complete remission of UC after conventional therapy considered a “golden standard for the treatment of inflammatory bowel disease” provides controversial results, due to severe destructive ulcers and reparative sclerotic changes of the colon mucosa (CM) in these diseases [4].
The purpose of our study was to evaluate the morpho-functional state of the colon mucosa in patients with ulcerative colitis after a single transplantation of autologous cultured mesenchymal bone marrow cells (MSC) against the background of standard therapy.
Patients and methods
Patients with ulcerative colitis were divided into 3 groups undergoing clinical, laboratory and morphological studies. The initial group of patients with UC before treatment included 18 subjects. Nine patients of them, received standard anti-inflammatory therapy (control group) which included 5-aminosalicylic acid (mesalazine), azathiopril, prednisone. Nine patients were treated with standard therapy supplemented by single MSC transplantation (main group) with a follow-up terms of about 10 months. Mesenchymal stem cells from bone marrow were cultured in DMEM culture medium for 14-21 days. Amounts and viability of in vitrocultured mesenchymal cells were evaluated by light microscopy, assessing activity of proliferation-associated Ki-67 antigen, production of specific biologically active substances. Transplantation of autologous mesenchymal bone marrow cells was performed once at a dose of 120-200 million cells in 200 ml of saline infused intravenously at a rate of 50 mL/h for 2.5 hours. Clinical and functional state of the patients (age from 24 to 57 years, men 11 and 7 women) with UC in the course of treatment was assessed according to the modified classifications by Truelove and Witts with updated recommendations G. Adler [5], Mayo and Rakhmilevich indices [6], extraintestinal manifestations, hemoglobin level, ESR, CRP and fecal calprotectin. 64 samples light-optical (semi-thin sections) and 320 microscopic examination of biopsy material taken endoscopically from different parts of the large intestine were subjected to histological and immunohistochemical studies. Histological sections of CM were stained with hematoxylin and eosin. Histological evaluation of the activity of inflammatory bowel disease was carried out semiquantitavely by K. Geboes et al. [7]. At the same time, structural changes, the density of inflammatory infiltration and the defects of the CM mucosa were assessed from 0 to 3 points. Immunohistochemical studies included detection of CD4, CD68, CD31, CD34, CD8, lgG, Ki-67 expression. For electron microscopy, the biopsy samples were fixed in in a 2.5% solution of glutaraldehyde with postfixation in 1% OsO4 and then processed according to the standard technique [8]. Semi-thin and ultra-thin sections were obtained in a Leica EM UC 7 ultramicrotome (Austria). Semi-thin sections, which allow high-resolution light microscopy, were stained with Methylene Blue, Azur 2, and basic fuchsin dye, according to C. Humphrey and F. Pittman [9]. Ultrathin sections were contrasted with uranyl acetate and lead citrate according to Reynolds. Ultrathin sections were observed and captured using a Libra 120 electron microscope (K. Zeiss, Germany).
Results
Ten months after the beginning of treatment, the entire clinical and laboratory symptomatics of the patients from MCS-treated group improved or stabilized as compared to the initial condition, remaining unchanged or more severe in the control group. Significant differences in the dynamics of hemoglobin, C-reactive protein and fecal calprotein in patients of the main and control groups were not observed. Positive dynamics of normalization of the ESR level in patients of MSC-treated group were noted. In 4 patients of the main group (44.5%), normalization of the ESR level was noted, in 3 of the studied (33.3%) ESR remained at the same level, in 2 patients (22.2%) there was an increase in the level of ESR. In the control group of patients receiving only standard therapy in 9 patients (100%), the level of ESR did not change, including in patients with elevated ESR. Thus, in the main group compared with the control group, there was a positive trend in the normalization of ESR.
Meanwhile, periods of exacerbation were noted in 3 of 9 patients in the control group. The index of inflammatory activity of ulcerative colitis according to Rakhmilevich in the main group decreased from 6-9 to 4-5 points remained unchanged in the control group, and even being increased in one patient. Mayo index in the main group also slightly decreased from 7 to 5-6 points, but remained unchanged or increased in the control group. According to Truelove and Wiits scale, the degree of inflammatory activity remained unchanged in both groups, which may be explained by more generalized characteristics of this classification. When evaluating histological and immunohistochemical changes of large intestinal mucosa (LIM) in patients of the main and control groups compared with patients of the initial group, a decrease in T-lymphocytic inflammatory response was observed from severe and moderate to moderate and weak (from 2-3 to 1-2 points) with a decrease in the population of CD8+ lymphocytes. The density of the inflammatory infiltrate decreased from 2 to 3 points (Fig. 1, a). Erosive and ulcerative defects of CM (2-3 points) remained at similar level, or changed slightly. However, the number, length of crypts, number of goblet cells in epithelium and crypts were increased, flattening of the epithelium was decreased (from 2 to 1 point) and damage to the crypts (1-2 to 0-1 points) was also diminished. Interepithelial neutrophilic infiltration with decreased. Eosinophilic infiltration of the lamina propria of the mucous membrane was absent. Indicators of the positive dynamics of improving the pathological characteristics of CM in the main group of patients were observed in 5 of 6 patients, in the control in 2 of 9 patients.
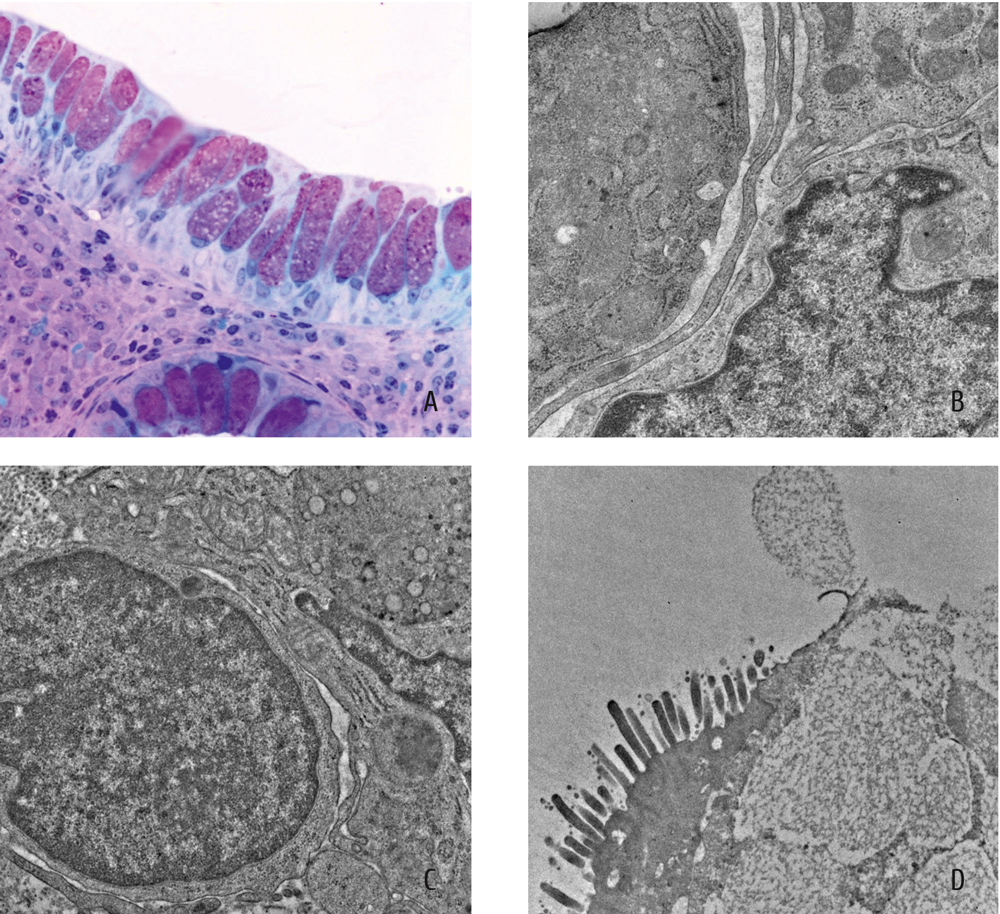
Figure 1. Morphology of large intestinal mucosa after 6 months of single MSCs transplantation with standard therapy
(a) Reduction in the density of lympho-plasmacytic inflammatory infiltrate increase in the number of goblet cells in the integumentary epithelium and crypts section. Semi-thin section. Staining with Methylene Blue, Azure-2 and basic fuchsin. x400.
(b) Tight intercellular contact between the lymphocyte and the macrophage. Electron diffraction technique.
(c) Telocyte between the cells of inflammatory infiltrate. Electron diffraction technique.
(d) Cylindrical cell with microvilli, and a goblet cell with granules of mucus. Electron diffraction technique.
Discussion
Electron microscopic data revealed possible mechanisms of the positive effect of the secretion of mesenchymal stem cells on the immunocompetent, microcirculatory, neurotrophic systems, cellular and non-cellular components of the stroma of the mucous membrane of the large intestine and restoration of the epithelium. Numerous intimate contacts and small exosomes between lymphocytes, plasma cells and macrophages with high phagocytic and secretory activity were noted electronically (Fig. 1, b). Macrophages are given a key role in the presentation of the antigen and the realization of the effect of regeneration with the participation of various populations of lymphoid cells [10]. It is quite possible that the immunomodulating function of macrophages was also carried out with the help of telocytes, the long processes which were everywhere located between the cells of the inflammatory infiltrate (Fig. 1, c). First described as a new type of interstitial cells, telocytes are presumably involved in the regeneration of tissues, the formation of stem cell niches and intercellular communication through the secretion of extracellular vesicles and nanocontacts [11]. A necessary requirement for assessing the number and condition of these cells is the visualization of their double immunohistochemical staining. Although the immunohistochemical indicators of the level of angiogenesis (CD 34+ cells) were as high as before the treatment, the blood capillaries were characterized by an increased “working” area of endothelium, pronounced vesicle formation and numerous outgrowth of the luminal and basal surface. Amyelinic terminal nerve endings were numerous and contained a large number of small axons. On semi-thin sections, we observed a decrease in the degree of fibrosis of the connective tissue, due to fibroclasia of collagen fibrils. The proliferative activity of the epithelium at the neck of crypts was high, as proven by the Ki-67 antigen expression. The proliferating cells were characterized by a high degree of differentiation into goblet cells, which indicates the restoration of the secretory function of the integumentary epithelium. Cylindrical cells located on the basement membrane had different degrees of differentiation. Less differentiated cells had the appearance of vacuolation cells with poorly developed microvilli. Typical cylindrical cells had well-developed microvilli and tight intercellular contacts between long cytoplasmic processes (Fig. 1, d). Single intercellular contacts such as desmosomes in the proliferating epithelium indicated the differentiation of stem cells in the direction of the squamous epithelium, as it was phylogenetically more ancient and stable. Multivesicular endosomes were related to secretory exosomes involved in the regulation of anti-inflammatory processes [12]. Destruction of the granular endoplasmic reticulum canaliculi, and the decrease in the density of secretory granules were noted in the cytoplasm of serotonin-containing cells. A decrease in the functional activity of serotonin-containing cells is characteristic of the stage of remission of ulcerative colitis [13].
Conclusion
Inclusion of a single autologous bone marrow MSC transplant into the standard therapy of patients with ulcerative colitis 10 months after treatment generally improved the clinical and laboratory picture of the disease, as compared with the initial state and the control group. In morphological study of LIM in patients of the main and control groups, erosive and ulcerative defects persisted or slightly decreased. Indicators of positive dynamics of improving the pathological characteristics of LIM manifested mainly in patients of the MSC-treated. Group, as a decrease in local inflammatory response and restoration of crypts (“epithelial niche”) with increased number of goblet cells and a decrease in permeability of the cover epithelium. Thus, a single transplantation of autologous mesenchymal cultured bone marrow cells accompanied by standard therapy had a positive effect on the morpho-functional state of LIM in UC patients. As a part of the ongoing scientific and technical program, multiple MSC transplantation will be studied in order to achieve a more efficient histological LIM recovery in patients with ulcerative colitis.
Conflict of interest
None declared.
Acknowledgement
The work was carried out within the framework of the scientific and technical program “Transplantation of stem (mesenchymal) cells in regenerative medicine” 013 (2017-2019).
References
- Soler D, Chapman T, Yang LL, Wyant T, Egan R, Fedyk ER. The binding specificity and selective antagonism of vedolizumab, an anti-alpha4beta7 integrin therapeutic antibody in development for inflammatory bowel diseases. J Pharmacol Exp Ther. 2009;330(3):864-875.
- Farre R, Vicario M. Abnormal barrier function in gastrointestinal disorders, Handbook Exp Pharmacol. 2017:239:193-217.doi:10.1007/164_2016_107.
- Knyazev OV, Fadeeva NA, Kagramanova AV, Lishchinskaya AA et al. Frequency of relapses in patients with ulcerative colitis and Crohn's disease, receiving cell therapy – 5 years of observation (Abstract). Materials of the III National Congress on Regenerative Medicine. Genes and Cells. 2017; 12 (3).
- Villanacci V, Antonelli E, Geboes K, Casella G, Bassotti G. Histological healing in inflammatory bowel disease: a still unfulfilled promise. World J Gastroenterol. 2013; 19(7): 968-978.
- Adler G. Crohn’s disease and ulcerative colitis. Moscow: Geotar MED, 2001 (In Russian).
- Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, Ferrante M, Götz M, Katsanos KH, Kießlich R, Ordás I, Repici A, Rosa B, Sebastian S, Kucharzik T, Eliakim R; European Crohn's and Colitis Organisation. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7(12):982-1018.
- Geboes K, Riddell R, Ost A, Jensfelt B, Persson T, Löfberg R. A reproducible grading scale for histological assessment of inflammation in ulcerative colitis. Gut. 2000;47(3):404-409.
- Glauert A. Fixation,dehydration and embedding of biological specimens. In: Practical Methods in Electron Microscopy (Ed. By Glauert AM). North-Holland : American Elsevier.1975.
- Humphrey C, Pittman F. A simple methylene blue-azure II-basic fuchsin stain for epoxy-embedded tissue sections. Stain Technol. 1974;49(1):9-14.
- Murrey PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nature Rev Immunol. 2011; 11(11): 723-737.
- Popescu LM, Nicolescu MI. Telocytes and stem cells. (Inos Santos Goldenberg RC, de Carvalho ACC, eds). Resident stem cells and regenerative therapy. MA: Academic Press. 2013: 205-231.
- van Niel G, Raposo G, Candalh C, Boussac M, Hershberg R, Cerf-Bensussan N, Heyman M. Intestinal epithelial cells secrete exosome-like vesicles. Gastroenterology. 2001;121(2):337-349.
- Rybakova MG, Botina V, Solovyeva OI. Immunomorphological characteristic of the colon mucosal cells and endocrine structures in the patients with chronic ulcerous colitis. Arch Patol. 2005; 67(2):30-33 (In Russian).
Introduction
Modern therapy of inflammatory bowel disease takes into account the complex multifactorial pathogenetic mechanisms of development of this pathology [1, 2]. In view of the immunocorrective and immunosuppressive properties of mesenchymal stem cells, it is important to study the effectiveness of cellular therapy for patients with ulcerative colitis (UC). Immune component of pathogenesis in these immunological disorders is of sufficient importance. The inclusion of mesenchymal stromal cell transplantation in anticytokine and immunosuppressive therapy in patients with ulcerative colitis and Crohn's disease contributed to the positive dynamics of the clinical remission of these diseases [3]. However, morphological changes in large intestine mucosa (LIM) following cell therapy are still poorly understood from the standpoint of the “stem cell niche” and the mechanisms of participation of mesenchymal stem cells (MSCs) in the regulation of regenerative processes. Histological assessment of the complete remission of UC after conventional therapy considered a “golden standard for the treatment of inflammatory bowel disease” provides controversial results, due to severe destructive ulcers and reparative sclerotic changes of the colon mucosa (CM) in these diseases [4].
The purpose of our study was to evaluate the morpho-functional state of the colon mucosa in patients with ulcerative colitis after a single transplantation of autologous cultured mesenchymal bone marrow cells (MSC) against the background of standard therapy.
Patients and methods
Patients with ulcerative colitis were divided into 3 groups undergoing clinical, laboratory and morphological studies. The initial group of patients with UC before treatment included 18 subjects. Nine patients of them, received standard anti-inflammatory therapy (control group) which included 5-aminosalicylic acid (mesalazine), azathiopril, prednisone. Nine patients were treated with standard therapy supplemented by single MSC transplantation (main group) with a follow-up terms of about 10 months. Mesenchymal stem cells from bone marrow were cultured in DMEM culture medium for 14-21 days. Amounts and viability of in vitrocultured mesenchymal cells were evaluated by light microscopy, assessing activity of proliferation-associated Ki-67 antigen, production of specific biologically active substances. Transplantation of autologous mesenchymal bone marrow cells was performed once at a dose of 120-200 million cells in 200 ml of saline infused intravenously at a rate of 50 mL/h for 2.5 hours. Clinical and functional state of the patients (age from 24 to 57 years, men 11 and 7 women) with UC in the course of treatment was assessed according to the modified classifications by Truelove and Witts with updated recommendations G. Adler [5], Mayo and Rakhmilevich indices [6], extraintestinal manifestations, hemoglobin level, ESR, CRP and fecal calprotectin. 64 samples light-optical (semi-thin sections) and 320 microscopic examination of biopsy material taken endoscopically from different parts of the large intestine were subjected to histological and immunohistochemical studies. Histological sections of CM were stained with hematoxylin and eosin. Histological evaluation of the activity of inflammatory bowel disease was carried out semiquantitavely by K. Geboes et al. [7]. At the same time, structural changes, the density of inflammatory infiltration and the defects of the CM mucosa were assessed from 0 to 3 points. Immunohistochemical studies included detection of CD4, CD68, CD31, CD34, CD8, lgG, Ki-67 expression. For electron microscopy, the biopsy samples were fixed in in a 2.5% solution of glutaraldehyde with postfixation in 1% OsO4 and then processed according to the standard technique [8]. Semi-thin and ultra-thin sections were obtained in a Leica EM UC 7 ultramicrotome (Austria). Semi-thin sections, which allow high-resolution light microscopy, were stained with Methylene Blue, Azur 2, and basic fuchsin dye, according to C. Humphrey and F. Pittman [9]. Ultrathin sections were contrasted with uranyl acetate and lead citrate according to Reynolds. Ultrathin sections were observed and captured using a Libra 120 electron microscope (K. Zeiss, Germany).
Results
Ten months after the beginning of treatment, the entire clinical and laboratory symptomatics of the patients from MCS-treated group improved or stabilized as compared to the initial condition, remaining unchanged or more severe in the control group. Significant differences in the dynamics of hemoglobin, C-reactive protein and fecal calprotein in patients of the main and control groups were not observed. Positive dynamics of normalization of the ESR level in patients of MSC-treated group were noted. In 4 patients of the main group (44.5%), normalization of the ESR level was noted, in 3 of the studied (33.3%) ESR remained at the same level, in 2 patients (22.2%) there was an increase in the level of ESR. In the control group of patients receiving only standard therapy in 9 patients (100%), the level of ESR did not change, including in patients with elevated ESR. Thus, in the main group compared with the control group, there was a positive trend in the normalization of ESR.
Meanwhile, periods of exacerbation were noted in 3 of 9 patients in the control group. The index of inflammatory activity of ulcerative colitis according to Rakhmilevich in the main group decreased from 6-9 to 4-5 points remained unchanged in the control group, and even being increased in one patient. Mayo index in the main group also slightly decreased from 7 to 5-6 points, but remained unchanged or increased in the control group. According to Truelove and Wiits scale, the degree of inflammatory activity remained unchanged in both groups, which may be explained by more generalized characteristics of this classification. When evaluating histological and immunohistochemical changes of large intestinal mucosa (LIM) in patients of the main and control groups compared with patients of the initial group, a decrease in T-lymphocytic inflammatory response was observed from severe and moderate to moderate and weak (from 2-3 to 1-2 points) with a decrease in the population of CD8+ lymphocytes. The density of the inflammatory infiltrate decreased from 2 to 3 points (Fig. 1, a). Erosive and ulcerative defects of CM (2-3 points) remained at similar level, or changed slightly. However, the number, length of crypts, number of goblet cells in epithelium and crypts were increased, flattening of the epithelium was decreased (from 2 to 1 point) and damage to the crypts (1-2 to 0-1 points) was also diminished. Interepithelial neutrophilic infiltration with decreased. Eosinophilic infiltration of the lamina propria of the mucous membrane was absent. Indicators of the positive dynamics of improving the pathological characteristics of CM in the main group of patients were observed in 5 of 6 patients, in the control in 2 of 9 patients.
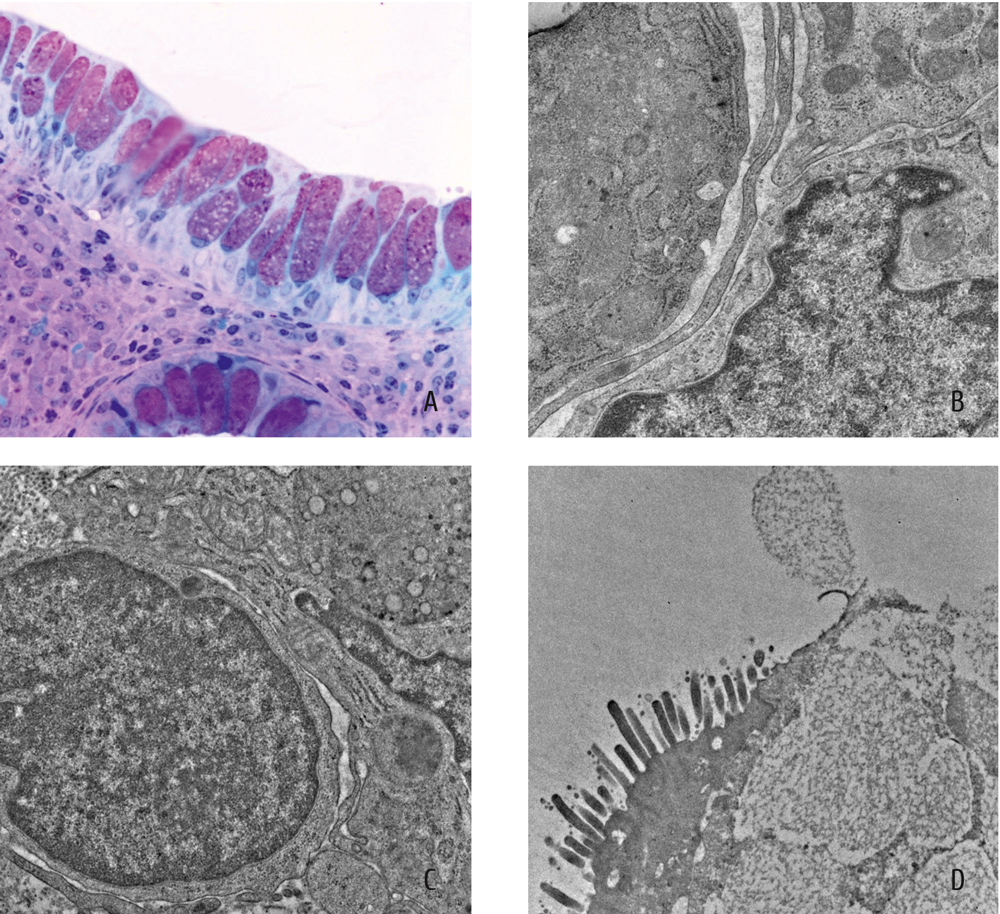
Figure 1. Morphology of large intestinal mucosa after 6 months of single MSCs transplantation with standard therapy
(a) Reduction in the density of lympho-plasmacytic inflammatory infiltrate increase in the number of goblet cells in the integumentary epithelium and crypts section. Semi-thin section. Staining with Methylene Blue, Azure-2 and basic fuchsin. x400.
(b) Tight intercellular contact between the lymphocyte and the macrophage. Electron diffraction technique.
(c) Telocyte between the cells of inflammatory infiltrate. Electron diffraction technique.
(d) Cylindrical cell with microvilli, and a goblet cell with granules of mucus. Electron diffraction technique.
Discussion
Electron microscopic data revealed possible mechanisms of the positive effect of the secretion of mesenchymal stem cells on the immunocompetent, microcirculatory, neurotrophic systems, cellular and non-cellular components of the stroma of the mucous membrane of the large intestine and restoration of the epithelium. Numerous intimate contacts and small exosomes between lymphocytes, plasma cells and macrophages with high phagocytic and secretory activity were noted electronically (Fig. 1, b). Macrophages are given a key role in the presentation of the antigen and the realization of the effect of regeneration with the participation of various populations of lymphoid cells [10]. It is quite possible that the immunomodulating function of macrophages was also carried out with the help of telocytes, the long processes which were everywhere located between the cells of the inflammatory infiltrate (Fig. 1, c). First described as a new type of interstitial cells, telocytes are presumably involved in the regeneration of tissues, the formation of stem cell niches and intercellular communication through the secretion of extracellular vesicles and nanocontacts [11]. A necessary requirement for assessing the number and condition of these cells is the visualization of their double immunohistochemical staining. Although the immunohistochemical indicators of the level of angiogenesis (CD 34+ cells) were as high as before the treatment, the blood capillaries were characterized by an increased “working” area of endothelium, pronounced vesicle formation and numerous outgrowth of the luminal and basal surface. Amyelinic terminal nerve endings were numerous and contained a large number of small axons. On semi-thin sections, we observed a decrease in the degree of fibrosis of the connective tissue, due to fibroclasia of collagen fibrils. The proliferative activity of the epithelium at the neck of crypts was high, as proven by the Ki-67 antigen expression. The proliferating cells were characterized by a high degree of differentiation into goblet cells, which indicates the restoration of the secretory function of the integumentary epithelium. Cylindrical cells located on the basement membrane had different degrees of differentiation. Less differentiated cells had the appearance of vacuolation cells with poorly developed microvilli. Typical cylindrical cells had well-developed microvilli and tight intercellular contacts between long cytoplasmic processes (Fig. 1, d). Single intercellular contacts such as desmosomes in the proliferating epithelium indicated the differentiation of stem cells in the direction of the squamous epithelium, as it was phylogenetically more ancient and stable. Multivesicular endosomes were related to secretory exosomes involved in the regulation of anti-inflammatory processes [12]. Destruction of the granular endoplasmic reticulum canaliculi, and the decrease in the density of secretory granules were noted in the cytoplasm of serotonin-containing cells. A decrease in the functional activity of serotonin-containing cells is characteristic of the stage of remission of ulcerative colitis [13].
Conclusion
Inclusion of a single autologous bone marrow MSC transplant into the standard therapy of patients with ulcerative colitis 10 months after treatment generally improved the clinical and laboratory picture of the disease, as compared with the initial state and the control group. In morphological study of LIM in patients of the main and control groups, erosive and ulcerative defects persisted or slightly decreased. Indicators of positive dynamics of improving the pathological characteristics of LIM manifested mainly in patients of the MSC-treated. Group, as a decrease in local inflammatory response and restoration of crypts (“epithelial niche”) with increased number of goblet cells and a decrease in permeability of the cover epithelium. Thus, a single transplantation of autologous mesenchymal cultured bone marrow cells accompanied by standard therapy had a positive effect on the morpho-functional state of LIM in UC patients. As a part of the ongoing scientific and technical program, multiple MSC transplantation will be studied in order to achieve a more efficient histological LIM recovery in patients with ulcerative colitis.
Conflict of interest
None declared.
Acknowledgement
The work was carried out within the framework of the scientific and technical program “Transplantation of stem (mesenchymal) cells in regenerative medicine” 013 (2017-2019).
References
- Soler D, Chapman T, Yang LL, Wyant T, Egan R, Fedyk ER. The binding specificity and selective antagonism of vedolizumab, an anti-alpha4beta7 integrin therapeutic antibody in development for inflammatory bowel diseases. J Pharmacol Exp Ther. 2009;330(3):864-875.
- Farre R, Vicario M. Abnormal barrier function in gastrointestinal disorders, Handbook Exp Pharmacol. 2017:239:193-217.doi:10.1007/164_2016_107.
- Knyazev OV, Fadeeva NA, Kagramanova AV, Lishchinskaya AA et al. Frequency of relapses in patients with ulcerative colitis and Crohn's disease, receiving cell therapy – 5 years of observation (Abstract). Materials of the III National Congress on Regenerative Medicine. Genes and Cells. 2017; 12 (3).
- Villanacci V, Antonelli E, Geboes K, Casella G, Bassotti G. Histological healing in inflammatory bowel disease: a still unfulfilled promise. World J Gastroenterol. 2013; 19(7): 968-978.
- Adler G. Crohn’s disease and ulcerative colitis. Moscow: Geotar MED, 2001 (In Russian).
- Annese V, Daperno M, Rutter MD, Amiot A, Bossuyt P, East J, Ferrante M, Götz M, Katsanos KH, Kießlich R, Ordás I, Repici A, Rosa B, Sebastian S, Kucharzik T, Eliakim R; European Crohn's and Colitis Organisation. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7(12):982-1018.
- Geboes K, Riddell R, Ost A, Jensfelt B, Persson T, Löfberg R. A reproducible grading scale for histological assessment of inflammation in ulcerative colitis. Gut. 2000;47(3):404-409.
- Glauert A. Fixation,dehydration and embedding of biological specimens. In: Practical Methods in Electron Microscopy (Ed. By Glauert AM). North-Holland : American Elsevier.1975.
- Humphrey C, Pittman F. A simple methylene blue-azure II-basic fuchsin stain for epoxy-embedded tissue sections. Stain Technol. 1974;49(1):9-14.
- Murrey PJ, Wynn TA. Protective and pathogenic functions of macrophage subsets. Nature Rev Immunol. 2011; 11(11): 723-737.
- Popescu LM, Nicolescu MI. Telocytes and stem cells. (Inos Santos Goldenberg RC, de Carvalho ACC, eds). Resident stem cells and regenerative therapy. MA: Academic Press. 2013: 205-231.
- van Niel G, Raposo G, Candalh C, Boussac M, Hershberg R, Cerf-Bensussan N, Heyman M. Intestinal epithelial cells secrete exosome-like vesicles. Gastroenterology. 2001;121(2):337-349.
- Rybakova MG, Botina V, Solovyeva OI. Immunomorphological characteristic of the colon mucosal cells and endocrine structures in the patients with chronic ulcerous colitis. Arch Patol. 2005; 67(2):30-33 (In Russian).
Галина В. Федотовских, Галия М. Шаймарданова, Манарбек Б. Аскаров, Майя С. Жумабаева, Гульмира С. Досатаева, Айгерим К. Смагулова, Сапаргуль Марат, Татьяна Г. Ежеленко
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22182" ["VALUE"]=> array(2) { ["TEXT"]=> string(161) "<p>АО «Национальный научный медицинский центр», г. Нур-Cултан (Астана), Казахстан </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(149) "АО «Национальный научный медицинский центр», г. Нур-Cултан (Астана), Казахстан
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_RU"]=> array(36) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22183" ["VALUE"]=> array(2) { ["TEXT"]=> string(5163) "<p style="text-align: justify;">Применение мезенхимных стволовых клеток костного мозга (МСК) при воспалительных заболеваниях кишечника показало свою выполнимость в клинических исследованиях. Целью настоящей работы было исследование морфо-функционального состояния слизистой толстого кишечника в срок 10 мес. после единичной инфузии культивированных <i>in vitro</i> и размноженных МСК в дополнение к стандартной терапии больных с язвенным колитом (ЯК).</p> <h3>Материалы и методы</h3> <p style="text-align: justify;">Исходная группа пациентов с ЯК включала 18 человек. Девять из них получали стандартную терапию (контрольная группа), а шесть человек проходили аналогичное лечение с добавлением разовой трансплантацией аутологичных МСК (экспериментальная группа). Клиническое и функциональное состояние пациентов оценивали по индексам Truelove и Wiits, а также Mayo и Rakhmilevich. Рутинная световая микроскопия, а также электронно-микроскопические (ЭМ) исследования проводили для 320 биоптатов слизистой толстого кишечника (СТК). Специфическое гистологическое и иммуногистохимическое обследование выполнено в 64 образцах. Гистологические признаки воспалительной активности оценивали в баллах по K.Geboes et al. Иммуногистохимические исследования включали анализ экспрессии маркеров CD4, CD68, CD31, CD34, CD8, IgG и Ki-67. ЭМ проводили по общепринятой методике. Полутонкие срезы окрашивали по Humphrey и Pittman. Ультратонкие срезы изучали и локализовали с помощью электронного микроскопа Libra 120. </p> <h3>Результаты</h3> <p style="text-align: justify;">Разовая трансплантация аутологичных культивированных МСК костного мозга в добавление к стандартной терапии больных с ЯК, в целом, улучшали клинические и лабораторные симптомы заболевания при исследовании через 10 мес. после лечения при сравнении с исходным клиническим статусом и контрольной группой. При морфологическом исследовании СТК в обеих группах была отмечена персистенция или некоторое уменьшение эрозивных и язвенных дефектов. Показатели позитивной динамики структуры СТК проявлялись, главным образом, у пациентов экспериментальной группы в виде снижения воспалительной реакции и восстановления кишечных крипт (<i>“эпителиальной ниши”</i>), с увеличением числа goblet-клеток и сниженной проницаемостью кишечного покровного эпителия.</p> <h3>Заключение</h3> <p style="text-align: justify;">Разовая трансплантация аутологичных культивированных МСК костного мозга может быть внедрена в стандартную терапию пациентов с ЯК, что оказывает позитивный эффект на морфофунциональное состояние СТК, тем самым способствуя снижению воспалительной реакции, восстановлению крипт и покровного эпителия. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Язвенный колит, аутологичная трансплантация костного мозга, мезенхимные клетки, трансплантация, кишечные крипты, морфология.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(4981) "Применение мезенхимных стволовых клеток костного мозга (МСК) при воспалительных заболеваниях кишечника показало свою выполнимость в клинических исследованиях. Целью настоящей работы было исследование морфо-функционального состояния слизистой толстого кишечника в срок 10 мес. после единичной инфузии культивированных in vitro и размноженных МСК в дополнение к стандартной терапии больных с язвенным колитом (ЯК).
Материалы и методы
Исходная группа пациентов с ЯК включала 18 человек. Девять из них получали стандартную терапию (контрольная группа), а шесть человек проходили аналогичное лечение с добавлением разовой трансплантацией аутологичных МСК (экспериментальная группа). Клиническое и функциональное состояние пациентов оценивали по индексам Truelove и Wiits, а также Mayo и Rakhmilevich. Рутинная световая микроскопия, а также электронно-микроскопические (ЭМ) исследования проводили для 320 биоптатов слизистой толстого кишечника (СТК). Специфическое гистологическое и иммуногистохимическое обследование выполнено в 64 образцах. Гистологические признаки воспалительной активности оценивали в баллах по K.Geboes et al. Иммуногистохимические исследования включали анализ экспрессии маркеров CD4, CD68, CD31, CD34, CD8, IgG и Ki-67. ЭМ проводили по общепринятой методике. Полутонкие срезы окрашивали по Humphrey и Pittman. Ультратонкие срезы изучали и локализовали с помощью электронного микроскопа Libra 120.
Результаты
Разовая трансплантация аутологичных культивированных МСК костного мозга в добавление к стандартной терапии больных с ЯК, в целом, улучшали клинические и лабораторные симптомы заболевания при исследовании через 10 мес. после лечения при сравнении с исходным клиническим статусом и контрольной группой. При морфологическом исследовании СТК в обеих группах была отмечена персистенция или некоторое уменьшение эрозивных и язвенных дефектов. Показатели позитивной динамики структуры СТК проявлялись, главным образом, у пациентов экспериментальной группы в виде снижения воспалительной реакции и восстановления кишечных крипт (“эпителиальной ниши”), с увеличением числа goblet-клеток и сниженной проницаемостью кишечного покровного эпителия.
Заключение
Разовая трансплантация аутологичных культивированных МСК костного мозга может быть внедрена в стандартную терапию пациентов с ЯК, что оказывает позитивный эффект на морфофунциональное состояние СТК, тем самым способствуя снижению воспалительной реакции, восстановлению крипт и покровного эпителия.
Ключевые слова
Язвенный колит, аутологичная трансплантация костного мозга, мезенхимные клетки, трансплантация, кишечные крипты, морфология.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22184" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-58-62" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-58-62" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22195" ["VALUE"]=> array(2) { ["TEXT"]=> string(192) "<p>Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(180) "Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22196" ["VALUE"]=> array(2) { ["TEXT"]=> string(86) "<p>National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(74) "National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22197" ["VALUE"]=> array(2) { ["TEXT"]=> string(3049) "<p style="text-align: justify;">Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured <i>in vitro</i> expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).</p> <h3>Materials and methods</h3> <p style="text-align: justify;">Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.</p> <h3>Results</h3> <p style="text-align: justify;">A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.</p> <h3>Conclusion</h3> <p style="text-align: justify;">Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.</p> <h2>Keywords</h2> <p style="text-align: justify;">Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2879) "Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured in vitro expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).
Materials and methods
Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.
Results
A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.
Conclusion
Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.
Keywords
Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22185" ["VALUE"]=> string(111) "Efficiency of mesenchymal stem cell therapy in ulcerative colitis as assessed by the morphology of colon mucosa" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(111) "Efficiency of mesenchymal stem cell therapy in ulcerative colitis as assessed by the morphology of colon mucosa" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22186" ["VALUE"]=> string(4) "1625" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1625" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22198" ["VALUE"]=> string(4) "1626" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1626" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(12) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22195" ["VALUE"]=> array(2) { ["TEXT"]=> string(192) "<p>Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(180) "Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(180) "Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22197" ["VALUE"]=> array(2) { ["TEXT"]=> string(3049) "<p style="text-align: justify;">Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured <i>in vitro</i> expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).</p> <h3>Materials and methods</h3> <p style="text-align: justify;">Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.</p> <h3>Results</h3> <p style="text-align: justify;">A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.</p> <h3>Conclusion</h3> <p style="text-align: justify;">Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.</p> <h2>Keywords</h2> <p style="text-align: justify;">Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2879) "Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured in vitro expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).
Materials and methods
Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.
Results
A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.
Conclusion
Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.
Keywords
Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(2879) "Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured in vitro expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).
Materials and methods
Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.
Results
A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.
Conclusion
Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.
Keywords
Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22184" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-58-62" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-58-62" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(37) "10.18620/ctt-1866-8836-2019-8-2-58-62" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22185" ["VALUE"]=> string(111) "Efficiency of mesenchymal stem cell therapy in ulcerative colitis as assessed by the morphology of colon mucosa" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(111) "Efficiency of mesenchymal stem cell therapy in ulcerative colitis as assessed by the morphology of colon mucosa" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(111) "Efficiency of mesenchymal stem cell therapy in ulcerative colitis as assessed by the morphology of colon mucosa" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22196" ["VALUE"]=> array(2) { ["TEXT"]=> string(86) "<p>National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(74) "National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(74) "National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan
" } ["AUTHORS"]=> array(38) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> array(8) { [0]=> string(5) "22483" [1]=> string(5) "22484" [2]=> string(5) "22485" [3]=> string(5) "22486" [4]=> string(5) "22487" [5]=> string(5) "22488" [6]=> string(5) "22489" [7]=> string(5) "22490" } ["VALUE"]=> array(8) { [0]=> string(4) "1653" [1]=> string(4) "1654" [2]=> string(4) "1655" [3]=> string(4) "1656" [4]=> string(4) "1657" [5]=> string(4) "1658" [6]=> string(4) "1659" [7]=> string(4) "1660" } ["DESCRIPTION"]=> array(8) { [0]=> string(0) "" [1]=> string(0) "" [2]=> string(0) "" [3]=> string(0) "" [4]=> string(0) "" [5]=> string(0) "" [6]=> string(0) "" [7]=> string(0) "" } ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(8) { [0]=> string(4) "1653" [1]=> string(4) "1654" [2]=> string(4) "1655" [3]=> string(4) "1656" [4]=> string(4) "1657" [5]=> string(4) "1658" [6]=> string(4) "1659" [7]=> string(4) "1660" } ["~DESCRIPTION"]=> array(8) { [0]=> string(0) "" [1]=> string(0) "" [2]=> string(0) "" [3]=> string(0) "" [4]=> string(0) "" [5]=> string(0) "" [6]=> string(0) "" [7]=> string(0) "" } ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> array(8) { [0]=> string(66) "Galina V. Fedotovskikh" [1]=> string(67) "Galija M. Shaymardanova" [2]=> string(63) "Manarbek B. Askarov" [3]=> string(64) "Maiya S. Zhumabayeva" [4]=> string(64) "Gulmira S. Dosataeva" [5]=> string(64) "Aigerim K. Smagulova" [6]=> string(58) "Sapargul Marat" [7]=> string(64) "Tatyana G. Ezhelenko" } ["LINK_ELEMENT_VALUE"]=> bool(false) } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22181" ["VALUE"]=> array(2) { ["TEXT"]=> string(317) "<p>Галина В. Федотовских, Галия М. Шаймарданова, Манарбек Б. Аскаров, Майя С. Жумабаева, Гульмира С. Досатаева, Айгерим К. Смагулова, Сапаргуль Марат, Татьяна Г. Ежеленко</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(305) "Галина В. Федотовских, Галия М. Шаймарданова, Манарбек Б. Аскаров, Майя С. Жумабаева, Гульмира С. Досатаева, Айгерим К. Смагулова, Сапаргуль Марат, Татьяна Г. Ежеленко
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(305) "Галина В. Федотовских, Галия М. Шаймарданова, Манарбек Б. Аскаров, Майя С. Жумабаева, Гульмира С. Досатаева, Айгерим К. Смагулова, Сапаргуль Марат, Татьяна Г. Ежеленко
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22170" ["VALUE"]=> string(22) "05/16/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "05/16/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "05/16/2019 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22171" ["VALUE"]=> string(22) "06/26/2019 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "06/26/2019 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "06/26/2019 12:00:00 am" } ["CONTACT"]=> array(38) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22172" ["VALUE"]=> string(4) "1653" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "1653" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(66) "Galina V. Fedotovskikh" ["LINK_ELEMENT_VALUE"]=> bool(false) } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22183" ["VALUE"]=> array(2) { ["TEXT"]=> string(5163) "<p style="text-align: justify;">Применение мезенхимных стволовых клеток костного мозга (МСК) при воспалительных заболеваниях кишечника показало свою выполнимость в клинических исследованиях. Целью настоящей работы было исследование морфо-функционального состояния слизистой толстого кишечника в срок 10 мес. после единичной инфузии культивированных <i>in vitro</i> и размноженных МСК в дополнение к стандартной терапии больных с язвенным колитом (ЯК).</p> <h3>Материалы и методы</h3> <p style="text-align: justify;">Исходная группа пациентов с ЯК включала 18 человек. Девять из них получали стандартную терапию (контрольная группа), а шесть человек проходили аналогичное лечение с добавлением разовой трансплантацией аутологичных МСК (экспериментальная группа). Клиническое и функциональное состояние пациентов оценивали по индексам Truelove и Wiits, а также Mayo и Rakhmilevich. Рутинная световая микроскопия, а также электронно-микроскопические (ЭМ) исследования проводили для 320 биоптатов слизистой толстого кишечника (СТК). Специфическое гистологическое и иммуногистохимическое обследование выполнено в 64 образцах. Гистологические признаки воспалительной активности оценивали в баллах по K.Geboes et al. Иммуногистохимические исследования включали анализ экспрессии маркеров CD4, CD68, CD31, CD34, CD8, IgG и Ki-67. ЭМ проводили по общепринятой методике. Полутонкие срезы окрашивали по Humphrey и Pittman. Ультратонкие срезы изучали и локализовали с помощью электронного микроскопа Libra 120. </p> <h3>Результаты</h3> <p style="text-align: justify;">Разовая трансплантация аутологичных культивированных МСК костного мозга в добавление к стандартной терапии больных с ЯК, в целом, улучшали клинические и лабораторные симптомы заболевания при исследовании через 10 мес. после лечения при сравнении с исходным клиническим статусом и контрольной группой. При морфологическом исследовании СТК в обеих группах была отмечена персистенция или некоторое уменьшение эрозивных и язвенных дефектов. Показатели позитивной динамики структуры СТК проявлялись, главным образом, у пациентов экспериментальной группы в виде снижения воспалительной реакции и восстановления кишечных крипт (<i>“эпителиальной ниши”</i>), с увеличением числа goblet-клеток и сниженной проницаемостью кишечного покровного эпителия.</p> <h3>Заключение</h3> <p style="text-align: justify;">Разовая трансплантация аутологичных культивированных МСК костного мозга может быть внедрена в стандартную терапию пациентов с ЯК, что оказывает позитивный эффект на морфофунциональное состояние СТК, тем самым способствуя снижению воспалительной реакции, восстановлению крипт и покровного эпителия. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Язвенный колит, аутологичная трансплантация костного мозга, мезенхимные клетки, трансплантация, кишечные крипты, морфология.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(4981) "Применение мезенхимных стволовых клеток костного мозга (МСК) при воспалительных заболеваниях кишечника показало свою выполнимость в клинических исследованиях. Целью настоящей работы было исследование морфо-функционального состояния слизистой толстого кишечника в срок 10 мес. после единичной инфузии культивированных in vitro и размноженных МСК в дополнение к стандартной терапии больных с язвенным колитом (ЯК).
Материалы и методы
Исходная группа пациентов с ЯК включала 18 человек. Девять из них получали стандартную терапию (контрольная группа), а шесть человек проходили аналогичное лечение с добавлением разовой трансплантацией аутологичных МСК (экспериментальная группа). Клиническое и функциональное состояние пациентов оценивали по индексам Truelove и Wiits, а также Mayo и Rakhmilevich. Рутинная световая микроскопия, а также электронно-микроскопические (ЭМ) исследования проводили для 320 биоптатов слизистой толстого кишечника (СТК). Специфическое гистологическое и иммуногистохимическое обследование выполнено в 64 образцах. Гистологические признаки воспалительной активности оценивали в баллах по K.Geboes et al. Иммуногистохимические исследования включали анализ экспрессии маркеров CD4, CD68, CD31, CD34, CD8, IgG и Ki-67. ЭМ проводили по общепринятой методике. Полутонкие срезы окрашивали по Humphrey и Pittman. Ультратонкие срезы изучали и локализовали с помощью электронного микроскопа Libra 120.
Результаты
Разовая трансплантация аутологичных культивированных МСК костного мозга в добавление к стандартной терапии больных с ЯК, в целом, улучшали клинические и лабораторные симптомы заболевания при исследовании через 10 мес. после лечения при сравнении с исходным клиническим статусом и контрольной группой. При морфологическом исследовании СТК в обеих группах была отмечена персистенция или некоторое уменьшение эрозивных и язвенных дефектов. Показатели позитивной динамики структуры СТК проявлялись, главным образом, у пациентов экспериментальной группы в виде снижения воспалительной реакции и восстановления кишечных крипт (“эпителиальной ниши”), с увеличением числа goblet-клеток и сниженной проницаемостью кишечного покровного эпителия.
Заключение
Разовая трансплантация аутологичных культивированных МСК костного мозга может быть внедрена в стандартную терапию пациентов с ЯК, что оказывает позитивный эффект на морфофунциональное состояние СТК, тем самым способствуя снижению воспалительной реакции, восстановлению крипт и покровного эпителия.
Ключевые слова
Язвенный колит, аутологичная трансплантация костного мозга, мезенхимные клетки, трансплантация, кишечные крипты, морфология.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(4981) "Применение мезенхимных стволовых клеток костного мозга (МСК) при воспалительных заболеваниях кишечника показало свою выполнимость в клинических исследованиях. Целью настоящей работы было исследование морфо-функционального состояния слизистой толстого кишечника в срок 10 мес. после единичной инфузии культивированных in vitro и размноженных МСК в дополнение к стандартной терапии больных с язвенным колитом (ЯК).
Материалы и методы
Исходная группа пациентов с ЯК включала 18 человек. Девять из них получали стандартную терапию (контрольная группа), а шесть человек проходили аналогичное лечение с добавлением разовой трансплантацией аутологичных МСК (экспериментальная группа). Клиническое и функциональное состояние пациентов оценивали по индексам Truelove и Wiits, а также Mayo и Rakhmilevich. Рутинная световая микроскопия, а также электронно-микроскопические (ЭМ) исследования проводили для 320 биоптатов слизистой толстого кишечника (СТК). Специфическое гистологическое и иммуногистохимическое обследование выполнено в 64 образцах. Гистологические признаки воспалительной активности оценивали в баллах по K.Geboes et al. Иммуногистохимические исследования включали анализ экспрессии маркеров CD4, CD68, CD31, CD34, CD8, IgG и Ki-67. ЭМ проводили по общепринятой методике. Полутонкие срезы окрашивали по Humphrey и Pittman. Ультратонкие срезы изучали и локализовали с помощью электронного микроскопа Libra 120.
Результаты
Разовая трансплантация аутологичных культивированных МСК костного мозга в добавление к стандартной терапии больных с ЯК, в целом, улучшали клинические и лабораторные симптомы заболевания при исследовании через 10 мес. после лечения при сравнении с исходным клиническим статусом и контрольной группой. При морфологическом исследовании СТК в обеих группах была отмечена персистенция или некоторое уменьшение эрозивных и язвенных дефектов. Показатели позитивной динамики структуры СТК проявлялись, главным образом, у пациентов экспериментальной группы в виде снижения воспалительной реакции и восстановления кишечных крипт (“эпителиальной ниши”), с увеличением числа goblet-клеток и сниженной проницаемостью кишечного покровного эпителия.
Заключение
Разовая трансплантация аутологичных культивированных МСК костного мозга может быть внедрена в стандартную терапию пациентов с ЯК, что оказывает позитивный эффект на морфофунциональное состояние СТК, тем самым способствуя снижению воспалительной реакции, восстановлению крипт и покровного эпителия.
Ключевые слова
Язвенный колит, аутологичная трансплантация костного мозга, мезенхимные клетки, трансплантация, кишечные крипты, морфология.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "22182" ["VALUE"]=> array(2) { ["TEXT"]=> string(161) "<p>АО «Национальный научный медицинский центр», г. Нур-Cултан (Астана), Казахстан </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(149) "АО «Национальный научный медицинский центр», г. Нур-Cултан (Астана), Казахстан
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(149) "АО «Национальный научный медицинский центр», г. Нур-Cултан (Астана), Казахстан
" } } } }Clinical studies
Marina O. Popova 1, Alisa G. Volkova 1, Inna V. Markova 1, Oksana V. Ayzsilnieks 1, Yulia A. Rogacheva 1, Anastasia S. Frolova 1, Aleksandr N. Shvetcov 1, Ilya Y. Nikolaev 1, Svetlana M. Ignatyeva 2, Tatyana S. Bogomolova 2, Asmic G. Gevorgian 1, Olesya V. Paina 1, Tatiana A. Bykova 1, Elena I. Darskaya 1, Maria V. Vladovskaya 1, Ivan S. Moiseev 1, Ludmila S. Zubarovskaya 1, Nikolay N. Klimko 1,2, Boris V. Afanasyev 1
Egor A. Kulagin 1, Alisa G. Volkova 2, Ilya Yu. Nikolaev 2, Oleg V. Goloshchapov 2, Anna G. Smirnova 2, Tatiana A. Rudakova 2, Elena I. Darskaya 2, Elena V. Morozova 2, Nataliya B. Mikhaylova 2, Julia D. Rabik 3, Victoria G. Timchik 3, Tatiana I. Shchemelinina 3, Ruf D. Skvortsova 3, Tatiana S. Razumovskaya 3, Sergey N. Bondarenko 2, Ivan S. Moiseev 2, Valeriy N. Marchenko 1, Vasiliy I. Trofimov 1, Boris V. Afanasyev 2
Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev
Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko,
Boris V. Afanasyev
Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 23004
[VALUE] => 07/30/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 07/30/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 23005
[VALUE] => 08/09/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 08/09/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => 23006
[VALUE] => 1241
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1241
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => Array
(
[0] => 23210
[1] => 23211
[2] => 23212
[3] => 23213
[4] => 23214
[5] => 23215
[6] => 23216
[7] => 23217
[8] => 23218
[9] => 23219
[10] => 23220
[11] => 23221
[12] => 23222
[13] => 23223
[14] => 23224
[15] => 23225
[16] => 23226
[17] => 23227
[18] => 23228
)
[VALUE] => Array
(
[0] => 1241
[1] => 1665
[2] => 135
[3] => 1675
[4] => 1676
[5] => 1677
[6] => 1678
[7] => 1666
[8] => 1679
[9] => 1680
[10] => 165
[11] => 130
[12] => 1642
[13] => 285
[14] => 1681
[15] => 60
[16] => 42
[17] => 1247
[18] => 34
)
[DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
[8] =>
[9] =>
[10] =>
[11] =>
[12] =>
[13] =>
[14] =>
[15] =>
[16] =>
[17] =>
[18] =>
)
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[0] => 1241
[1] => 1665
[2] => 135
[3] => 1675
[4] => 1676
[5] => 1677
[6] => 1678
[7] => 1666
[8] => 1679
[9] => 1680
[10] => 165
[11] => 130
[12] => 1642
[13] => 285
[14] => 1681
[15] => 60
[16] => 42
[17] => 1247
[18] => 34
)
[~DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
[8] =>
[9] =>
[10] =>
[11] =>
[12] =>
[13] =>
[14] =>
[15] =>
[16] =>
[17] =>
[18] =>
)
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 23050
[VALUE] => Array
(
[TEXT] => <p>Марина О. Попова <sup>1</sup>, Алиса Г. Волкова <sup>1</sup>, Инна В. Маркова <sup>1</sup>, Оксана В. Айзсилниекс <sup>1</sup>, Юлия А. Рогачева <sup>1</sup>, Анастасия С. Фролова <sup>1</sup>, Александр Н. Швецов <sup>1</sup>, Илья Ю. Николаев <sup>1</sup>, Светлана М. Игнатьева <sup>2</sup>, Татьяна С. Богомолова <sup>2</sup>, Асмик Г. Геворгян <sup>1</sup>, Олеся В. Паина <sup>1</sup>, Татьяна А. Быкова <sup>1</sup>, Елена И. Дарская <sup>1</sup>, Мария В. Владовская <sup>1</sup>, Иван С. Моисеев <sup>1</sup>, Людмила С. Зубаровская <sup>1</sup>, Николай Н. Климко <sup>1,2</sup>, Борис В. Афанасьев <sup>1</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Марина О. Попова 1, Алиса Г. Волкова 1, Инна В. Маркова 1, Оксана В. Айзсилниекс 1, Юлия А. Рогачева 1, Анастасия С. Фролова 1, Александр Н. Швецов 1, Илья Ю. Николаев 1, Светлана М. Игнатьева 2, Татьяна С. Богомолова 2, Асмик Г. Геворгян 1, Олеся В. Паина 1, Татьяна А. Быкова 1, Елена И. Дарская 1, Мария В. Владовская 1, Иван С. Моисеев 1, Людмила С. Зубаровская 1, Николай Н. Климко 1,2, Борис В. Афанасьев 1
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 23051
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургсий государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия<br>
<sup>2</sup> НИИ Медицинской микологии им. П. Н. Кашкина, Северо-западный государственный медицинский университет им. И. И. Мечникова, Санкт-Петербург, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургсий государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 НИИ Медицинской микологии им. П. Н. Кашкина, Северо-западный государственный медицинский университет им. И. И. Мечникова, Санкт-Петербург, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 23052
[VALUE] => Array
(
[TEXT] => <p style="text-align:justify";>Внедрение новых противогрибковых средств и диагностических процедур улучшило прогноз гематологических пациентов с инвазивными микозами (ИМ). Увеличилось число пациентов с ИМ, кандидатов на аллогенную трансплантацию гемопоэтических стволовых клеток (алло-ТГСК). Роль ИМ, развившихся до алло-ТГСК, по-прежнему не определена. Нет опубликованных данных о результатах алло-ТГСК у педиатрических пациентов с предшествующим ИМ. Цель исследования – оценить влияние предшествующего ИМ на результаты алло-ТГСК. </p>
<h3>Пациенты и методы</h3>
<p style="text-align:justify";>В проспективное исследование были включены 504 реципиента алло-ТГСК в период с января 2013 года по июль 2016 года. Средний возраст составил 24 года (2 месяца – 76 лет), дети (<18 лет) – 164, взрослые – 340, мужчины – 52%. Преимущественно пациенты с диагнозом острый лейкоз группы высокого риска (74,6%). Алло-ТГСК от неродственного совместимого донора были выполнены у 58,5%, совместимого родственного донора – 22,5%, гаплоидентичного – 19%, преимущественно с использованием режима кондиционирования со сниженной интенсивностью (67%). Непосредственно перед алло-ТГСК всем пациентам с обнаруженными изменениями ткани легких, в результате компьютерной томографии органов грудной клетки, выполнялась бронхоскопия с исследованием жидкости бронхоальвеолярного лаважа: микроскопии, культуры и теста на галактоманнан. Для диагностики доказанного и вероятного ИМ и оценки ответа на терапию были использованы критерии EORTC/MSG 2008. «Активный ИМ» – ИМ, диагностированный непосредственно перед трансплантацией. Медиана наблюдения составила 20 месяцев. Основными конечными точками были общая выживаемость (ОВ), частота рецидива или прогрессирования ИМ после алло-ТГСК; вторичные точки – частота острой и хронической РТПХ, рецидива основного заболевания.</p>
<h3>Результаты</h3>
<p style="text-align:justify";>Частота ИМ до алло-ТГСК составила 15% (n=76). Согласно критериям EORTS/MSG 2008, 90,8% пациентов имели вероятный и 9,2% доказанный ИМ. Этиология ИМ до трансплантации: инвазивный аспергиллез (ИА) – 75%, инвазивный кандидоз (ИК) – 13%, мукормикоз (М) – 4%, пневмоцистная пневмония (ПП) – 1,3% и комбинация ИА с М диагностирована у 2 пациентов, с ИК – 1, с ПП – 1. Основным органом поражения были легкие – 95%, другие локализации, преимущественно в сочетании с вовлечением легких: синусы – 9%, селезенка – 6%, печень – 6%, и мягкие ткани – 3%. Противогрибковая терапия перед алло-ТГСК применялась у 75% пациентов с медианой продолжительности – 2 месяца. Полный ответ на противогрибковую терапию был достигнут у 38,2% пациентов, частичный ответ или стабилизация – 35,5%, а у 26,3% пациентов был «активный ИМ». После алло-ТГСК все пациенты получали противогрибковую терапию или вторичную профилактику в соответствии с этиологией ИМ. Кумулятивная частота рецидива или прогрессирования ИМ после алло-ТГСК составила 14,5%. Отсутствие ремиссии основного заболевания в момент трансплантации был единственным фактором риска рецидива или прогрессирования ИМ после алло-ТГСК (11,5% против 21,1%, p=0,03). Существенных различий в кумулятивной частоте острой (p=0,28), хронической РТПХ (p=0,25) и рецидива (p=0,31) не было обнаружено в сравнении с группой пациентов без ИМ в анамнезе. 3-летняя ОВ после алло-ТГСК составила 67,5%. Общая выживаемость у реципиентов аллоТГСК без ИМ и имевших ИМ в анамнезе статистически не различалась во всех группах (60,5% против 68,7%, р=0,1), как отдельно у детей (50,0% против 57,4% , P=0,32) так и у взрослых (63,3% против 74,6%, p=0,09). Наихудший результат наблюдался у пациентов с «активным ИМ» и отсутствием ремиссии основного заболевания на момент трансплантации (3-летняя ОВ – 20%, р <0,001). Однако у пациентов с «активным ИМ» и ремиссией основного заболевания ОВ была аналогична выживаемости пациентов без ИМ в ананмнезе (80% против 68,7%, р=0,57).</p>
<h3>Выводы</h3>
<p style="text-align:justify";>Пятнадцать процентов реципиентов алло-ТГСК имели инвазивный микоз в анамнезе. Кумулятивная частота рецидива или прогрессирования инвазивных микозов после алло-ТГСК составила 14,5%. Предшествующий инвазивный микоз не оказывал существенного влияния на результаты трансплантации и общую выживаемость детей и взрослых после алло-ТГСК. Отсутствие ремиссии основного заболевания на момент трансплантации было единственным фактором риска рецидива или прогрессирования инвазивного микоза, и ухудшения результатов алло-ТГСК.</p>
<h2>Ключевые слова</h2>
<p style="text-align:justify";>Предшествующие инвазивные микозы, аллогенная трансплантация гемопоэтических стволовых клеток, дети и взрослые, клинические исходы.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Внедрение новых противогрибковых средств и диагностических процедур улучшило прогноз гематологических пациентов с инвазивными микозами (ИМ). Увеличилось число пациентов с ИМ, кандидатов на аллогенную трансплантацию гемопоэтических стволовых клеток (алло-ТГСК). Роль ИМ, развившихся до алло-ТГСК, по-прежнему не определена. Нет опубликованных данных о результатах алло-ТГСК у педиатрических пациентов с предшествующим ИМ. Цель исследования – оценить влияние предшествующего ИМ на результаты алло-ТГСК.
Пациенты и методы
В проспективное исследование были включены 504 реципиента алло-ТГСК в период с января 2013 года по июль 2016 года. Средний возраст составил 24 года (2 месяца – 76 лет), дети (<18 лет) – 164, взрослые – 340, мужчины – 52%. Преимущественно пациенты с диагнозом острый лейкоз группы высокого риска (74,6%). Алло-ТГСК от неродственного совместимого донора были выполнены у 58,5%, совместимого родственного донора – 22,5%, гаплоидентичного – 19%, преимущественно с использованием режима кондиционирования со сниженной интенсивностью (67%). Непосредственно перед алло-ТГСК всем пациентам с обнаруженными изменениями ткани легких, в результате компьютерной томографии органов грудной клетки, выполнялась бронхоскопия с исследованием жидкости бронхоальвеолярного лаважа: микроскопии, культуры и теста на галактоманнан. Для диагностики доказанного и вероятного ИМ и оценки ответа на терапию были использованы критерии EORTC/MSG 2008. «Активный ИМ» – ИМ, диагностированный непосредственно перед трансплантацией. Медиана наблюдения составила 20 месяцев. Основными конечными точками были общая выживаемость (ОВ), частота рецидива или прогрессирования ИМ после алло-ТГСК; вторичные точки – частота острой и хронической РТПХ, рецидива основного заболевания.
Результаты
Частота ИМ до алло-ТГСК составила 15% (n=76). Согласно критериям EORTS/MSG 2008, 90,8% пациентов имели вероятный и 9,2% доказанный ИМ. Этиология ИМ до трансплантации: инвазивный аспергиллез (ИА) – 75%, инвазивный кандидоз (ИК) – 13%, мукормикоз (М) – 4%, пневмоцистная пневмония (ПП) – 1,3% и комбинация ИА с М диагностирована у 2 пациентов, с ИК – 1, с ПП – 1. Основным органом поражения были легкие – 95%, другие локализации, преимущественно в сочетании с вовлечением легких: синусы – 9%, селезенка – 6%, печень – 6%, и мягкие ткани – 3%. Противогрибковая терапия перед алло-ТГСК применялась у 75% пациентов с медианой продолжительности – 2 месяца. Полный ответ на противогрибковую терапию был достигнут у 38,2% пациентов, частичный ответ или стабилизация – 35,5%, а у 26,3% пациентов был «активный ИМ». После алло-ТГСК все пациенты получали противогрибковую терапию или вторичную профилактику в соответствии с этиологией ИМ. Кумулятивная частота рецидива или прогрессирования ИМ после алло-ТГСК составила 14,5%. Отсутствие ремиссии основного заболевания в момент трансплантации был единственным фактором риска рецидива или прогрессирования ИМ после алло-ТГСК (11,5% против 21,1%, p=0,03). Существенных различий в кумулятивной частоте острой (p=0,28), хронической РТПХ (p=0,25) и рецидива (p=0,31) не было обнаружено в сравнении с группой пациентов без ИМ в анамнезе. 3-летняя ОВ после алло-ТГСК составила 67,5%. Общая выживаемость у реципиентов аллоТГСК без ИМ и имевших ИМ в анамнезе статистически не различалась во всех группах (60,5% против 68,7%, р=0,1), как отдельно у детей (50,0% против 57,4% , P=0,32) так и у взрослых (63,3% против 74,6%, p=0,09). Наихудший результат наблюдался у пациентов с «активным ИМ» и отсутствием ремиссии основного заболевания на момент трансплантации (3-летняя ОВ – 20%, р <0,001). Однако у пациентов с «активным ИМ» и ремиссией основного заболевания ОВ была аналогична выживаемости пациентов без ИМ в ананмнезе (80% против 68,7%, р=0,57).
Выводы
Пятнадцать процентов реципиентов алло-ТГСК имели инвазивный микоз в анамнезе. Кумулятивная частота рецидива или прогрессирования инвазивных микозов после алло-ТГСК составила 14,5%. Предшествующий инвазивный микоз не оказывал существенного влияния на результаты трансплантации и общую выживаемость детей и взрослых после алло-ТГСК. Отсутствие ремиссии основного заболевания на момент трансплантации было единственным фактором риска рецидива или прогрессирования инвазивного микоза, и ухудшения результатов алло-ТГСК.
Ключевые слова
Предшествующие инвазивные микозы, аллогенная трансплантация гемопоэтических стволовых клеток, дети и взрослые, клинические исходы.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 23026
[VALUE] => 10.18620/ctt-1866-8836-2019-8-2-17-25
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2019-8-2-17-25
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 23073
[VALUE] => Array
(
[TEXT] => <p>Marina O. Popova <sup>1</sup>, Alisa G. Volkova <sup>1</sup>, Inna V. Markova <sup>1</sup>, Oksana V. Ayzsilnieks <sup>1</sup>, Yulia A. Rogacheva <sup>1</sup>, Anastasia S. Frolova <sup>1</sup>, Aleksandr N. Shvetcov <sup>1</sup>, Ilya Y. Nikolaev <sup>1</sup>, Svetlana M. Ignatyeva <sup>2</sup>, Tatyana S. Bogomolova <sup>2</sup>, Asmic G. Gevorgian <sup>1</sup>, Olesya V. Paina <sup>1</sup>, Tatiana A. Bykova <sup>1</sup>, Elena I. Darskaya <sup>1</sup>, Maria V. Vladovskaya <sup>1</sup>, Ivan S. Moiseev <sup>1</sup>, Ludmila S. Zubarovskaya <sup>1</sup>, Nikolay N. Klimko <sup>1,2</sup>, Boris V. Afanasyev <sup>1</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Marina O. Popova 1, Alisa G. Volkova 1, Inna V. Markova 1, Oksana V. Ayzsilnieks 1, Yulia A. Rogacheva 1, Anastasia S. Frolova 1, Aleksandr N. Shvetcov 1, Ilya Y. Nikolaev 1, Svetlana M. Ignatyeva 2, Tatyana S. Bogomolova 2, Asmic G. Gevorgian 1, Olesya V. Paina 1, Tatiana A. Bykova 1, Elena I. Darskaya 1, Maria V. Vladovskaya 1, Ivan S. Moiseev 1, Ludmila S. Zubarovskaya 1, Nikolay N. Klimko 1,2, Boris V. Afanasyev 1
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 23074
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br>
<sup>2</sup> Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 23075
[VALUE] => Array
(
[TEXT] => <p style="text-align:justify";>Invasive fungal diseases (IFD) are a major cause of morbidity and mortality in hematological patients, but prognosis of IFD has improved recently, due to introduction of new antifungals and efficient diagnostic procedures. Number of patients with IFD who are candidates for allogeneic hematopoietic stem cell transplant (allo-HSCT) increased. However, publications on the field are limited and there are no data on results of pediatric allo-HSCT patients with prior IFD. This study focuses on the outcomes of allo-HSCT in children and adults with prior IFD.</p>
<h3>Patients and methods</h3>
<p style="text-align:justify";>In a prospective study, 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016. The median age was 24 y.o. [2 months to 76 years] including 164 children (<18 yo) and 340 adults. The cohort included 52% male patients. Most patients (74.6%) were diagnosed with high-risk acute leukemia. Allo-HSCT from HLA-matched unrelated donors (MUD) was performed in 58.5%, from matched related donors (MRD), 22.5%; haploidentical HSCT was performed in 19% of patients, predominantly with RIC (67%). EORTC/MSG 2008 criteria for diagnosis and response to therapy were used. In the patients with pre-transplant lung lesions detected by CT scan, bronchoscopy with BAL was used. “Active IFD” means IFD diagnosed just before HSCT.</p>
<h3>Results</h3>
<p style="text-align:justify";>Incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria, 90.8% of patients had probable and 9.2% presented with proven IFD. Etiology of IFD prior to HSCT was as follows: invasive aspergillosis (IA), 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; <i>Pneumocystis pneumoniae</i> (PCP), 1.3%, and combination of IA with Mu (2 cases), IC (n=1), PCP (n=1). The main sites of infection were lungs (95%), other localizations were predominantly combined with lung involvement: sinuses (9%), spleen (6%), liver (6%), and soft tissues (3%). Antifungal therapy before allo-HSCT was used in 75% patients with median duration of 2 months. Complete response to antifungal therapy was observed in 38.2% of the cases, partial response or stabilization was achieved in 35.5%, and “active IFD” was detected in 26.3% of the patients. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology. Cumulative incidence of relapse or progression of IFD after allo-HSCT was observed in 14.5%. Active underlying disease (hematology malignancy) at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% <i>vs</i> 21.1%, p=0,03). We detected no significant differences in the cumulative incidence of acute, chronic GVHD and relapse in the study group as compared to the patients without history of IFD. 3-year overall survival (OS) after allo-HSCT was 67.5%. The impact of prior IFD on overall survival in allo-HSCT recipients was not statistically significant for the entire group (60.5% <i>vs</i> 68.7%, p=0.1), and, separately, for children (50.0% <i>vs</i> 57.4%, p=0,3) and adults (63.3% <i>vs</i> 74.6%, p=0.09). The worst outcome was observed in the patients with “active IFD” and active underlying disease at the moment of HSCT (3-year OS was 20%, p<0.001 compared to patients without history of IFD). However, in the patients with “active IFD” and remission of underlying disease, OS value was similar to survival rate of patients without history of IFD (80% <i>vs</i> 68.7%, p=0.2). </p>
<h3>Conclusion</h3>
<p style="text-align:justify";>Incidence of IFD before allo-HSCT was 15%. Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5%. Prior IFD had no significant impact on transplant-related complications and overall survival in children and adults undergoing allo-HSCT. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT.</p>
<h2>Keywords</h2>
<p style="text-align:justify";>Invasive fungal disease, pre-existing IFD, allogeneic hematopoietic stem cell transplantation, children and adults, clinical outcomes.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Invasive fungal diseases (IFD) are a major cause of morbidity and mortality in hematological patients, but prognosis of IFD has improved recently, due to introduction of new antifungals and efficient diagnostic procedures. Number of patients with IFD who are candidates for allogeneic hematopoietic stem cell transplant (allo-HSCT) increased. However, publications on the field are limited and there are no data on results of pediatric allo-HSCT patients with prior IFD. This study focuses on the outcomes of allo-HSCT in children and adults with prior IFD.
Patients and methods
In a prospective study, 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016. The median age was 24 y.o. [2 months to 76 years] including 164 children (<18 yo) and 340 adults. The cohort included 52% male patients. Most patients (74.6%) were diagnosed with high-risk acute leukemia. Allo-HSCT from HLA-matched unrelated donors (MUD) was performed in 58.5%, from matched related donors (MRD), 22.5%; haploidentical HSCT was performed in 19% of patients, predominantly with RIC (67%). EORTC/MSG 2008 criteria for diagnosis and response to therapy were used. In the patients with pre-transplant lung lesions detected by CT scan, bronchoscopy with BAL was used. “Active IFD” means IFD diagnosed just before HSCT.
Results
Incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria, 90.8% of patients had probable and 9.2% presented with proven IFD. Etiology of IFD prior to HSCT was as follows: invasive aspergillosis (IA), 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; Pneumocystis pneumoniae (PCP), 1.3%, and combination of IA with Mu (2 cases), IC (n=1), PCP (n=1). The main sites of infection were lungs (95%), other localizations were predominantly combined with lung involvement: sinuses (9%), spleen (6%), liver (6%), and soft tissues (3%). Antifungal therapy before allo-HSCT was used in 75% patients with median duration of 2 months. Complete response to antifungal therapy was observed in 38.2% of the cases, partial response or stabilization was achieved in 35.5%, and “active IFD” was detected in 26.3% of the patients. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology. Cumulative incidence of relapse or progression of IFD after allo-HSCT was observed in 14.5%. Active underlying disease (hematology malignancy) at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% vs 21.1%, p=0,03). We detected no significant differences in the cumulative incidence of acute, chronic GVHD and relapse in the study group as compared to the patients without history of IFD. 3-year overall survival (OS) after allo-HSCT was 67.5%. The impact of prior IFD on overall survival in allo-HSCT recipients was not statistically significant for the entire group (60.5% vs 68.7%, p=0.1), and, separately, for children (50.0% vs 57.4%, p=0,3) and adults (63.3% vs 74.6%, p=0.09). The worst outcome was observed in the patients with “active IFD” and active underlying disease at the moment of HSCT (3-year OS was 20%, p<0.001 compared to patients without history of IFD). However, in the patients with “active IFD” and remission of underlying disease, OS value was similar to survival rate of patients without history of IFD (80% vs 68.7%, p=0.2).
Conclusion
Incidence of IFD before allo-HSCT was 15%. Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5%. Prior IFD had no significant impact on transplant-related complications and overall survival in children and adults undergoing allo-HSCT. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT.
Keywords
Invasive fungal disease, pre-existing IFD, allogeneic hematopoietic stem cell transplantation, children and adults, clinical outcomes.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 23027
[VALUE] => Outcomes of allogeneic hematopoietic stem cell transplantation in children and adults with prior invasive fungal diseases
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Outcomes of allogeneic hematopoietic stem cell transplantation in children and adults with prior invasive fungal diseases
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 23053
[VALUE] => 1662
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1662
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 23076
[VALUE] => 1663
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1663
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Marina O. Popova 1, Alisa G. Volkova 1, Inna V. Markova 1, Oksana V. Ayzsilnieks 1, Yulia A. Rogacheva 1, Anastasia S. Frolova 1, Aleksandr N. Shvetcov 1, Ilya Y. Nikolaev 1, Svetlana M. Ignatyeva 2, Tatyana S. Bogomolova 2, Asmic G. Gevorgian 1, Olesya V. Paina 1, Tatiana A. Bykova 1, Elena I. Darskaya 1, Maria V. Vladovskaya 1, Ivan S. Moiseev 1, Ludmila S. Zubarovskaya 1, Nikolay N. Klimko 1,2, Boris V. Afanasyev 1
1 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Dept. of Clinical Mycology, I. Mechnikov North-Western State Medical University, St. Petersburg, Russia
Invasive fungal diseases (IFD) are a major cause of morbidity and mortality in hematological patients, but prognosis of IFD has improved recently, due to introduction of new antifungals and efficient diagnostic procedures. Number of patients with IFD who are candidates for allogeneic hematopoietic stem cell transplant (allo-HSCT) increased. However, publications on the field are limited and there are no data on results of pediatric allo-HSCT patients with prior IFD. This study focuses on the outcomes of allo-HSCT in children and adults with prior IFD.
Patients and methods
In a prospective study, 504 allo-HSCT recipients were included from Jan 2013 to Jul 2016. The median age was 24 y.o. [2 months to 76 years] including 164 children (<18 yo) and 340 adults. The cohort included 52% male patients. Most patients (74.6%) were diagnosed with high-risk acute leukemia. Allo-HSCT from HLA-matched unrelated donors (MUD) was performed in 58.5%, from matched related donors (MRD), 22.5%; haploidentical HSCT was performed in 19% of patients, predominantly with RIC (67%). EORTC/MSG 2008 criteria for diagnosis and response to therapy were used. In the patients with pre-transplant lung lesions detected by CT scan, bronchoscopy with BAL was used. “Active IFD” means IFD diagnosed just before HSCT.
Results
Incidence of IFD before allo-HSCT was 15% (n=76). According to EORTS/MSG 2008 criteria, 90.8% of patients had probable and 9.2% presented with proven IFD. Etiology of IFD prior to HSCT was as follows: invasive aspergillosis (IA), 75%; invasive candidiasis (IC), 13%; mucormycosis (Mu), 4%; Pneumocystis pneumoniae (PCP), 1.3%, and combination of IA with Mu (2 cases), IC (n=1), PCP (n=1). The main sites of infection were lungs (95%), other localizations were predominantly combined with lung involvement: sinuses (9%), spleen (6%), liver (6%), and soft tissues (3%). Antifungal therapy before allo-HSCT was used in 75% patients with median duration of 2 months. Complete response to antifungal therapy was observed in 38.2% of the cases, partial response or stabilization was achieved in 35.5%, and “active IFD” was detected in 26.3% of the patients. After allo-HSCT, all the patients received antifungal therapy or secondary prophylaxis according to the IFD etiology. Cumulative incidence of relapse or progression of IFD after allo-HSCT was observed in 14.5%. Active underlying disease (hematology malignancy) at the moment of HSCT was the only risk factor for relapse or progression of IFD after allo-HSCT (11.5% vs 21.1%, p=0,03). We detected no significant differences in the cumulative incidence of acute, chronic GVHD and relapse in the study group as compared to the patients without history of IFD. 3-year overall survival (OS) after allo-HSCT was 67.5%. The impact of prior IFD on overall survival in allo-HSCT recipients was not statistically significant for the entire group (60.5% vs 68.7%, p=0.1), and, separately, for children (50.0% vs 57.4%, p=0,3) and adults (63.3% vs 74.6%, p=0.09). The worst outcome was observed in the patients with “active IFD” and active underlying disease at the moment of HSCT (3-year OS was 20%, p<0.001 compared to patients without history of IFD). However, in the patients with “active IFD” and remission of underlying disease, OS value was similar to survival rate of patients without history of IFD (80% vs 68.7%, p=0.2).
Conclusion
Incidence of IFD before allo-HSCT was 15%. Cumulative incidence of relapse or progression of IFD after allo-HSCT was 14.5%. Prior IFD had no significant impact on transplant-related complications and overall survival in children and adults undergoing allo-HSCT. Active underlying disease at the moment of HSCT was the only risk factor for relapse or progression of IFD and impaired outcome of allo-HSCT.
Keywords
Invasive fungal disease, pre-existing IFD, allogeneic hematopoietic stem cell transplantation, children and adults, clinical outcomes.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22574
[VALUE] => 07/30/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 07/30/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22575
[VALUE] => 08/09/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 08/09/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22576
[VALUE] => 1664
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1664
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => Array
(
[0] => 23756
[1] => 23757
[2] => 23758
[3] => 23759
[4] => 23760
[5] => 23761
[6] => 23762
[7] => 23763
[8] => 23764
[9] => 23765
[10] => 23766
[11] => 23767
[12] => 23768
[13] => 23769
[14] => 23770
[15] => 23771
[16] => 23772
[17] => 23773
[18] => 23774
)
[VALUE] => Array
(
[0] => 1664
[1] => 1665
[2] => 1666
[3] => 1244
[4] => 304
[5] => 1630
[6] => 285
[7] => 147
[8] => 1182
[9] => 1667
[10] => 1668
[11] => 1669
[12] => 1670
[13] => 1671
[14] => 1631
[15] => 60
[16] => 1672
[17] => 1673
[18] => 34
)
[DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
[8] =>
[9] =>
[10] =>
[11] =>
[12] =>
[13] =>
[14] =>
[15] =>
[16] =>
[17] =>
[18] =>
)
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[0] => 1664
[1] => 1665
[2] => 1666
[3] => 1244
[4] => 304
[5] => 1630
[6] => 285
[7] => 147
[8] => 1182
[9] => 1667
[10] => 1668
[11] => 1669
[12] => 1670
[13] => 1671
[14] => 1631
[15] => 60
[16] => 1672
[17] => 1673
[18] => 34
)
[~DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
[8] =>
[9] =>
[10] =>
[11] =>
[12] =>
[13] =>
[14] =>
[15] =>
[16] =>
[17] =>
[18] =>
)
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22617
[VALUE] => Array
(
[TEXT] => <p>Егор А. Кулагин <sup>1</sup>, Алиса Г. Волкова <sup>2</sup>, Илья Ю. Николаев <sup>2</sup>, Олег В. Голощапов <sup>2</sup>, Анна Г. Смирнова <sup>2</sup>,
Татьяна А. Рудакова <sup>2</sup>, Елена И. Дарская <sup>2</sup>, Елена В. Морозова <sup>2</sup>, Наталья Б. Михайлова <sup>2</sup>, Юлия Д. Рабик <sup>3</sup>,
Виктория Г. Тимчик <sup>3</sup>, Татьяна И. Щемелинина <sup>3</sup>, Руфь Д. Скворцова <sup>3</sup>, Татьяна С. Разумовская <sup>3</sup>, Сергей Н. Бондаренко <sup>2</sup>, Иван С. Моисеев <sup>2</sup>, Валерий Н. Марченко <sup>1</sup>, Василий И. Трофимов <sup>1</sup>, Борис В. Афанасьев <sup>2</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Егор А. Кулагин 1, Алиса Г. Волкова 2, Илья Ю. Николаев 2, Олег В. Голощапов 2, Анна Г. Смирнова 2,
Татьяна А. Рудакова 2, Елена И. Дарская 2, Елена В. Морозова 2, Наталья Б. Михайлова 2, Юлия Д. Рабик 3,
Виктория Г. Тимчик 3, Татьяна И. Щемелинина 3, Руфь Д. Скворцова 3, Татьяна С. Разумовская 3, Сергей Н. Бондаренко 2, Иван С. Моисеев 2, Валерий Н. Марченко 1, Василий И. Трофимов 1, Борис В. Афанасьев 2
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22618
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Кафедра госпитальной терапии с курсом аллергологии и иммунологии имени академика М.В. Черноруцкого, Санкт-Петербург, Россия<br>
<sup>2</sup> НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Санкт-Петербург, Россия<br>
<sup>3</sup> Отделение функциональной диагностики №2 Научно-клинического исследовательского центра,
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова» Минздрава России, Санкт-Петербург, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Кафедра госпитальной терапии с курсом аллергологии и иммунологии имени академика М.В. Черноруцкого, Санкт-Петербург, Россия
2 НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Санкт-Петербург, Россия
3 Отделение функциональной диагностики №2 Научно-клинического исследовательского центра,
ФГБОУ ВО «Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова» Минздрава России, Санкт-Петербург, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22619
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Высокая эффективность аллогенной трансплантации гемопоэтических стволовых клеток (алло-
ТГСК) при широком спектре злокачественных и незлокачественных заболеваний системы крови ограничивается риском тяжелых осложнений и летального исхода без признаков рецидива или прогрессирования основного заболевания (безрецидивная летальность). Среди ключевых факторов безрецидивной летальности рассматривается коморбидность до момента алло-ТГСК. Целью настоящего исследования было охарактеризовать потенциальные предтрансплантационные факторы легочной коморбидности и интегральные показатели функции внешнего дыхания (ФВД) и оценить их прогностическое значение для исходов алло-ТГСК у взрослых пациентов.</p>
<h3>Пациенты и методы</h3>
<p style="text-align: justify;">Исследование включало 355 больных, в том числе 149 (42%) в проспективной фазе исследования. Сформированная когорта включала пациентов с острыми лейкозами (60%), миелопролифератив-<br>ными заболеваниями (10%), миелодиспластическим синдромом (5%), лимфомами (17%) и тяжелой апластической анемией (8%). Медиана возраста на момент алло-ТГСК составила 33 года (18-66). Анализировались все потенциальные предтрансплантационные факторы легочной компрометации. Степень тяжести легочной коморбидности оценивалась на основании параметров ФВД – объема форсированного выдоха за первую секунду (ОФВ1) и диффузионной способности лёгких для оксида углерода (CO) (DLco) в соответствии с критериями индекса коморбидности Hematopoietic cell transplantation specific comorbidity index (HCT-CI). Прогностическое значение степени легочной коморбидности исследовано в отношении кумулятивной частоты перевода на искусственную вентиляцию легких (ИВЛ) и безрецидивной летальности.</p>
<h3>Результаты</h3>
<p style="text-align: justify;">Среди наиболее частых факторов легочной компрометации до алло-ТГСК идентифицированы курение (32%), анамнез хронической обструктивной болезни легких (ХОБЛ) и бронхиальной астмы (БА) (5%), инфекции легких (45%), потенциально пульмонотоксичная химиотерапия (79%), аутологичная ТГСК (8%), ингибиторы иммунных контрольных точек (5%), лучевая терапия на область средостения (6%) и др. Критериальное снижение ОФВ1 от должного имело место у 90 (25%) больных, включая 14%, 9% и 2% легкой, средней и тяжелой степени соответственно. Нарушение DLco было выявлено у 69% обследованных пациентов, включая 29%, 28% и 12% легкой, средней и тяжелой степени соответственно. Кумулятивная частота перевода на ИВЛ в течение 100 дней после алло-ТГСК составила 7,2%, 10,9%, 16,7% и 22,1% у пациентов с легочной коморбидностью 0, 1, 2, 3 степени соответственно. Степень легочной коморбидности была независимым фактором риска безрецидивной летальности (отношение рисков 1,39, ДИ 95%, 1.03-1.89, p=0.033) и ассоциировалась со снижением общей выживаемости. </p>
<h3>Выводы</h3>
<p style="text-align: justify;">Взрослые пациенты имеют широкий спектр факторов легочной коморбидности до алло-ТГСК. Легочная коморбидность по HCT-CI является фактором риска перевода на ИВЛ в течение первых 100 дней после алло-ТГСК и безрецидивной летальности. </p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Аллогенная трансплантация гемопоэтических стволовых клеток, взрослые, коморбидная патология легких, функция внешнего дыхания, клинический прогноз. </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Высокая эффективность аллогенной трансплантации гемопоэтических стволовых клеток (алло-
ТГСК) при широком спектре злокачественных и незлокачественных заболеваний системы крови ограничивается риском тяжелых осложнений и летального исхода без признаков рецидива или прогрессирования основного заболевания (безрецидивная летальность). Среди ключевых факторов безрецидивной летальности рассматривается коморбидность до момента алло-ТГСК. Целью настоящего исследования было охарактеризовать потенциальные предтрансплантационные факторы легочной коморбидности и интегральные показатели функции внешнего дыхания (ФВД) и оценить их прогностическое значение для исходов алло-ТГСК у взрослых пациентов.
Пациенты и методы
Исследование включало 355 больных, в том числе 149 (42%) в проспективной фазе исследования. Сформированная когорта включала пациентов с острыми лейкозами (60%), миелопролифератив-
ными заболеваниями (10%), миелодиспластическим синдромом (5%), лимфомами (17%) и тяжелой апластической анемией (8%). Медиана возраста на момент алло-ТГСК составила 33 года (18-66). Анализировались все потенциальные предтрансплантационные факторы легочной компрометации. Степень тяжести легочной коморбидности оценивалась на основании параметров ФВД – объема форсированного выдоха за первую секунду (ОФВ1) и диффузионной способности лёгких для оксида углерода (CO) (DLco) в соответствии с критериями индекса коморбидности Hematopoietic cell transplantation specific comorbidity index (HCT-CI). Прогностическое значение степени легочной коморбидности исследовано в отношении кумулятивной частоты перевода на искусственную вентиляцию легких (ИВЛ) и безрецидивной летальности.
Результаты
Среди наиболее частых факторов легочной компрометации до алло-ТГСК идентифицированы курение (32%), анамнез хронической обструктивной болезни легких (ХОБЛ) и бронхиальной астмы (БА) (5%), инфекции легких (45%), потенциально пульмонотоксичная химиотерапия (79%), аутологичная ТГСК (8%), ингибиторы иммунных контрольных точек (5%), лучевая терапия на область средостения (6%) и др. Критериальное снижение ОФВ1 от должного имело место у 90 (25%) больных, включая 14%, 9% и 2% легкой, средней и тяжелой степени соответственно. Нарушение DLco было выявлено у 69% обследованных пациентов, включая 29%, 28% и 12% легкой, средней и тяжелой степени соответственно. Кумулятивная частота перевода на ИВЛ в течение 100 дней после алло-ТГСК составила 7,2%, 10,9%, 16,7% и 22,1% у пациентов с легочной коморбидностью 0, 1, 2, 3 степени соответственно. Степень легочной коморбидности была независимым фактором риска безрецидивной летальности (отношение рисков 1,39, ДИ 95%, 1.03-1.89, p=0.033) и ассоциировалась со снижением общей выживаемости.
Выводы
Взрослые пациенты имеют широкий спектр факторов легочной коморбидности до алло-ТГСК. Легочная коморбидность по HCT-CI является фактором риска перевода на ИВЛ в течение первых 100 дней после алло-ТГСК и безрецидивной летальности.
Ключевые слова
Аллогенная трансплантация гемопоэтических стволовых клеток, взрослые, коморбидная патология легких, функция внешнего дыхания, клинический прогноз.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22596
[VALUE] => 10.18620/ctt-1866-8836-2019-8-2-26-37
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2019-8-2-26-37
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22716
[VALUE] => Array
(
[TEXT] => <p>Egor A. Kulagin <sup>1</sup>, Alisa G. Volkova <sup>2</sup>, Ilya Yu. Nikolaev <sup>2</sup>, Oleg V. Goloshchapov <sup>2</sup>, Anna G. Smirnova <sup>2</sup>, Tatiana A. Rudakova <sup>2</sup>, Elena I. Darskaya <sup>2</sup>, Elena V. Morozova <sup>2</sup>, Nataliya B. Mikhaylova <sup>2</sup>, Julia D. Rabik <sup>3</sup>, Victoria G. Timchik <sup>3</sup>, Tatiana I. Shchemelinina <sup>3</sup>, Ruf D. Skvortsova <sup>3</sup>, Tatiana S. Razumovskaya <sup>3</sup>, Sergey N. Bondarenko <sup>2</sup>, Ivan S. Moiseev <sup>2</sup>, Valeriy N. Marchenko <sup>1</sup>, Vasiliy I. Trofimov <sup>1</sup>, Boris V. Afanasyev <sup>2</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Egor A. Kulagin 1, Alisa G. Volkova 2, Ilya Yu. Nikolaev 2, Oleg V. Goloshchapov 2, Anna G. Smirnova 2, Tatiana A. Rudakova 2, Elena I. Darskaya 2, Elena V. Morozova 2, Nataliya B. Mikhaylova 2, Julia D. Rabik 3, Victoria G. Timchik 3, Tatiana I. Shchemelinina 3, Ruf D. Skvortsova 3, Tatiana S. Razumovskaya 3, Sergey N. Bondarenko 2, Ivan S. Moiseev 2, Valeriy N. Marchenko 1, Vasiliy I. Trofimov 1, Boris V. Afanasyev 2
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22717
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br>
<sup>2</sup> Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia<br>
<sup>3</sup> Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
3 Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22718
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">High efficacy of allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a wide range of malignant and non-malignant hematopoietic disorders system is limited to the risk of serious complications and non-relapse mortality (NRM). Pre-existing comorbidities before allo-HSCT are among key factors for NRM.</p>
<p style="text-align: justify;">The purpose of this study was to characterize the potential pre-transplant factors of pulmonary comorbidity and integral indicators of pulmonary function tests (PFT) and to evaluate their prognostic value for the allo-HSCT outcomes in adult patients.</p>
<h3>Patients and methods</h3>
<p style="text-align: justify;">The study included 355 patients, among them 149 (42%) in the prospective phase of the study. The cohort included patients with acute leukemia (60%), myeloproliferative diseases (10%), myelodysplastic syndrome (5%), lymphomas (17%), and severe aplastic anemia (8%). The median age at the time of allo-HSCT was 33 years old (18 to 66). We analyzed all the factors that could affect lung function before allo-HSCT. The severity of pulmonary comorbidity was assessed on the basis of forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco), in accordance with the criteria of the Hematopoietic Cell Transplantation Specific Comorbidity Index (HCT-CI). The prognostic value of pulmonary comorbidity was investigated with respect to the cumulative incidence of mechanical ventilation (MV) and NRM rates.</p>
<h3>Results</h3>
<p style="text-align: justify;">Tobacco smoking (32%), history of chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) (5%), previous pulmonary infections (45%), potentially pulmonary toxic chemotherapy (79%), previous auto-HSCT (8%), usage of immune checkpoint inhibitors (5%), mediastinal radiation therapy (6%) were the most common pulmonary compromising factors before allo-HSCT. According to the HCT-CI criteria, 90 patients (25%) had low FEV1 values, with 14%, 9% and 2% of mild, moderate and severe grade respectively. DLco disorders were diagnosed in 69% of the patients examined, including 29%, 28%, and 12% of mild, moderate, and severe grade respectively. Cumulative incidence of MV within 100 days after allo-HSCT was 7.2%, 10.9%, 16.7%, and 22.1% in patients with pulmonary comorbidity of 0, 1, 2, 3 degrees, respectively. The degree of pulmonary comorbidity was an independent risk factor for NRM (hazard ratio 1.39; CI 95%; 1.03-1.89; p=0.033), being associated with a decrease in overall survival (OS).</p>
<h3>Conclusions</h3>
<p style="text-align: justify;">Adult patients have a wide range of pulmonary comorbidity factors before allo-HSCT. HCT-CI pulmonary comorbidity is an independent risk factor for MV during the first 100 days after allo-HSCT and NRM. </p>
<h2>Keywords</h2>
<p style="text-align: justify;">Allogeneic hematopoietic stem cell transplantation, adults, pulmonary comorbidity, pulmonary functional tests, clinical prognosis. </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => High efficacy of allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a wide range of malignant and non-malignant hematopoietic disorders system is limited to the risk of serious complications and non-relapse mortality (NRM). Pre-existing comorbidities before allo-HSCT are among key factors for NRM.
The purpose of this study was to characterize the potential pre-transplant factors of pulmonary comorbidity and integral indicators of pulmonary function tests (PFT) and to evaluate their prognostic value for the allo-HSCT outcomes in adult patients.
Patients and methods
The study included 355 patients, among them 149 (42%) in the prospective phase of the study. The cohort included patients with acute leukemia (60%), myeloproliferative diseases (10%), myelodysplastic syndrome (5%), lymphomas (17%), and severe aplastic anemia (8%). The median age at the time of allo-HSCT was 33 years old (18 to 66). We analyzed all the factors that could affect lung function before allo-HSCT. The severity of pulmonary comorbidity was assessed on the basis of forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco), in accordance with the criteria of the Hematopoietic Cell Transplantation Specific Comorbidity Index (HCT-CI). The prognostic value of pulmonary comorbidity was investigated with respect to the cumulative incidence of mechanical ventilation (MV) and NRM rates.
Results
Tobacco smoking (32%), history of chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) (5%), previous pulmonary infections (45%), potentially pulmonary toxic chemotherapy (79%), previous auto-HSCT (8%), usage of immune checkpoint inhibitors (5%), mediastinal radiation therapy (6%) were the most common pulmonary compromising factors before allo-HSCT. According to the HCT-CI criteria, 90 patients (25%) had low FEV1 values, with 14%, 9% and 2% of mild, moderate and severe grade respectively. DLco disorders were diagnosed in 69% of the patients examined, including 29%, 28%, and 12% of mild, moderate, and severe grade respectively. Cumulative incidence of MV within 100 days after allo-HSCT was 7.2%, 10.9%, 16.7%, and 22.1% in patients with pulmonary comorbidity of 0, 1, 2, 3 degrees, respectively. The degree of pulmonary comorbidity was an independent risk factor for NRM (hazard ratio 1.39; CI 95%; 1.03-1.89; p=0.033), being associated with a decrease in overall survival (OS).
Conclusions
Adult patients have a wide range of pulmonary comorbidity factors before allo-HSCT. HCT-CI pulmonary comorbidity is an independent risk factor for MV during the first 100 days after allo-HSCT and NRM.
Keywords
Allogeneic hematopoietic stem cell transplantation, adults, pulmonary comorbidity, pulmonary functional tests, clinical prognosis.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22597
[VALUE] => Clinical features and prognostic value of functional disorders and pulmonary comorbidity in adult patients prior to allogeneic hematopoietic stem cell transplantation
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Clinical features and prognostic value of functional disorders and pulmonary comorbidity in adult patients prior to allogeneic hematopoietic stem cell transplantation
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22620
[VALUE] => 1649
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1649
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22719
[VALUE] => 1650
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1650
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Egor A. Kulagin 1, Alisa G. Volkova 2, Ilya Yu. Nikolaev 2, Oleg V. Goloshchapov 2, Anna G. Smirnova 2, Tatiana A. Rudakova 2, Elena I. Darskaya 2, Elena V. Morozova 2, Nataliya B. Mikhaylova 2, Julia D. Rabik 3, Victoria G. Timchik 3, Tatiana I. Shchemelinina 3, Ruf D. Skvortsova 3, Tatiana S. Razumovskaya 3, Sergey N. Bondarenko 2, Ivan S. Moiseev 2, Valeriy N. Marchenko 1, Vasiliy I. Trofimov 1, Boris V. Afanasyev 2
1 M. Chernorutskiy Department of Hospital Therapy, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
2 Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
3 Department of Functional Diagnostics №2, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
High efficacy of allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a wide range of malignant and non-malignant hematopoietic disorders system is limited to the risk of serious complications and non-relapse mortality (NRM). Pre-existing comorbidities before allo-HSCT are among key factors for NRM.
The purpose of this study was to characterize the potential pre-transplant factors of pulmonary comorbidity and integral indicators of pulmonary function tests (PFT) and to evaluate their prognostic value for the allo-HSCT outcomes in adult patients.
Patients and methods
The study included 355 patients, among them 149 (42%) in the prospective phase of the study. The cohort included patients with acute leukemia (60%), myeloproliferative diseases (10%), myelodysplastic syndrome (5%), lymphomas (17%), and severe aplastic anemia (8%). The median age at the time of allo-HSCT was 33 years old (18 to 66). We analyzed all the factors that could affect lung function before allo-HSCT. The severity of pulmonary comorbidity was assessed on the basis of forced expiratory volume in one second (FEV1) and diffusing capacity of carbon monoxide (CO) (DLco), in accordance with the criteria of the Hematopoietic Cell Transplantation Specific Comorbidity Index (HCT-CI). The prognostic value of pulmonary comorbidity was investigated with respect to the cumulative incidence of mechanical ventilation (MV) and NRM rates.
Results
Tobacco smoking (32%), history of chronic obstructive pulmonary disease (COPD) and bronchial asthma (BA) (5%), previous pulmonary infections (45%), potentially pulmonary toxic chemotherapy (79%), previous auto-HSCT (8%), usage of immune checkpoint inhibitors (5%), mediastinal radiation therapy (6%) were the most common pulmonary compromising factors before allo-HSCT. According to the HCT-CI criteria, 90 patients (25%) had low FEV1 values, with 14%, 9% and 2% of mild, moderate and severe grade respectively. DLco disorders were diagnosed in 69% of the patients examined, including 29%, 28%, and 12% of mild, moderate, and severe grade respectively. Cumulative incidence of MV within 100 days after allo-HSCT was 7.2%, 10.9%, 16.7%, and 22.1% in patients with pulmonary comorbidity of 0, 1, 2, 3 degrees, respectively. The degree of pulmonary comorbidity was an independent risk factor for NRM (hazard ratio 1.39; CI 95%; 1.03-1.89; p=0.033), being associated with a decrease in overall survival (OS).
Conclusions
Adult patients have a wide range of pulmonary comorbidity factors before allo-HSCT. HCT-CI pulmonary comorbidity is an independent risk factor for MV during the first 100 days after allo-HSCT and NRM.
Keywords
Allogeneic hematopoietic stem cell transplantation, adults, pulmonary comorbidity, pulmonary functional tests, clinical prognosis.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22278
[VALUE] => 07/31/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 07/31/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22279
[VALUE] => 08/09/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 08/09/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22280
[VALUE] => 1630
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1630
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => Array
(
[0] => 22470
[1] => 22471
[2] => 22472
[3] => 22473
[4] => 22474
[5] => 22475
[6] => 22476
[7] => 22477
[8] => 22478
[9] => 22479
[10] => 22480
[11] => 22481
[12] => 22482
)
[VALUE] => Array
(
[0] => 1630
[1] => 503
[2] => 60
[3] => 1642
[4] => 1631
[5] => 146
[6] => 1629
[7] => 1643
[8] => 303
[9] => 498
[10] => 285
[11] => 147
[12] => 34
)
[DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
[8] =>
[9] =>
[10] =>
[11] =>
[12] =>
)
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[0] => 1630
[1] => 503
[2] => 60
[3] => 1642
[4] => 1631
[5] => 146
[6] => 1629
[7] => 1643
[8] => 303
[9] => 498
[10] => 285
[11] => 147
[12] => 34
)
[~DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
[8] =>
[9] =>
[10] =>
[11] =>
[12] =>
)
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22294
[VALUE] => Array
(
[TEXT] => <p>Татьяна А. Рудакова, Александр Д. Кулагин, Иван С. Моисеев, Татьяна А. Быкова, Сергей Н. Бондаренко,
Мария В. Барабанщикова, Анастасия В. Бейнарович, Анна А. Осипова, Варвара Н. Овечкина, Александр Л. Алянский, Елена И. Дарская, Елена В. Морозова, Борис В. Афанасьев</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Татьяна А. Рудакова, Александр Д. Кулагин, Иван С. Моисеев, Татьяна А. Быкова, Сергей Н. Бондаренко,
Мария В. Барабанщикова, Анастасия В. Бейнарович, Анна А. Осипова, Варвара Н. Овечкина, Александр Л. Алянский, Елена И. Дарская, Елена В. Морозова, Борис В. Афанасьев
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22295
[VALUE] => Array
(
[TEXT] => <p>НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой Первого Санкт-Петербургского
государственного медицинского университета им. И. П. Павлова, Санкт-Петербург, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой Первого Санкт-Петербургского
государственного медицинского университета им. И. П. Павлова, Санкт-Петербург, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22296
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Посттрансплантационные цитопении в структуре гипофункции трансплантата являются жизнеугрожающим осложнением аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК). Общепринятые терапевтические опции для лечения ограничены повторными инфузиями гемопоэтических стволовых клеток. Однако миметики тромбопоэтина (ТПО), показавшие свою эффективность при идиопатической апластической анемией и тромбоцитопении (ромиплостим, элтромбопаг), могут рассматриваться в качестве возможной альтернативной стратегии терапии гипофункции трансплантата после алло-ТГСК. В данной работе представлен опыт использования агонистов рецептора тромбопоэтина для лечения посттрансплантационных цитопений, в том числе критериальной тяжелой гипофункции трансплантата после алло-ТГСК в нашем центре.</p>
<p style="text-align: justify;">В общей сложности 31 пациент (15 мужчин, 16 женщин) со средним возрастом 22 года (18-57) получили терапию агонистами рецептора ТПО (АР-ТПО) для посттрансплантационной тромбоцитопении <20×10<sup>9</sup>/л (n=7) и ГФТ (n=24). Для терапии использовался ромиплостим (n=17) со средней дозой 5 мкг/кг в неделю (3-5) или элтромбопаг (n=14) со средней дозой 50 мг/день (50-150). Критериями тяжелой гипофункции трансплантата (тГФТ) были: цитопения в двух или более миелоидных линиях (тромбоциты <20×10<sup>9</sup>/л, абсолютное число нейтрофилов (АЧН) <0,5×10<sup>9</sup>/л, гемоглобин <70 г/л в любое время после документированного приживления, полный или стабильный смешанный донорский химеризм >90% без признаков рецидива основного заболевания. Общий ответ включал полный ответ (ПО) (тромбоциты ≥100×10<sup>9</sup>/л, АЧН ≥1,5×109/л, гемоглобин ≥100 г/л) и частичный ответ (ЧО) (тромбоциты >20×10<sup>9</sup>/л, АЧН ≥0,5×10<sup>9</sup>/л, гемоглобин >70 г/л). Медиана времени от постановки диагноза тГФТ до начала терапии АР-ТПО составила 14 дней (0-119), медиана продолжительности терапии АР-ТПО составила 3 недели (1-43). Переносимость АР-ТПО была удовлетворительной, без признаков токсичности II-IV степени. В общей сложности в 8 случаях (28%) АР-ТПО использовались в комбинации с ритуксимабом (n=4), ритуксимабом и инфузиями донорских лимфоцитов (ИДЛ) (n=3), а также с инфузиями CD34-клеток (n=1). Всего 14 (48%) пациентов достигли ответа (ПО: n=4, 14%; ЧО: n=10, 34%). Комбинированная терапия не показала преимущества в скорости ответа по сравнению с АР-ТПО в монорежиме. Медиана прироста АЧН у ответивших на терапию составила 3,4×10<sup>9</sup>/л (0,8-6,0), тромбоцитов – 48×10<sup>9</sup>/л (21-205). В общей сложности 15 пациентов (3 ответивших, 12 не ответивших на терапию) умерли от инфекции (n=10), рецидива (n=2) и острой реакции «трансплантат-против-хозяина» (оРТПХ) III-IV степени (n=3). Однолетняя общая выживаемость (ОВ) от начала терапии составила 60% (95% ДИ, 40-76), при этом наблюдалась существенная разница между ответившими и неответившими на АР-ТПО: 79% (95% ДИ, 47-93) против 39% (95% ДИ, 14-63) (р=0,01). Наше исследование показало многообещающую эффективность и удовлетворительную безопасность АР-ТПО у пациентов с тГФТ после алло-ТГСК. Необходимо проведение многоцентровых проспективных исследований для установления оптимальной дозы и продолжительности приема, а также критериев отмены этих препаратов. </p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Алло-ТГСК, гипофункция трансплантата, агонисты рецепторов тромбопоэтина.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Посттрансплантационные цитопении в структуре гипофункции трансплантата являются жизнеугрожающим осложнением аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК). Общепринятые терапевтические опции для лечения ограничены повторными инфузиями гемопоэтических стволовых клеток. Однако миметики тромбопоэтина (ТПО), показавшие свою эффективность при идиопатической апластической анемией и тромбоцитопении (ромиплостим, элтромбопаг), могут рассматриваться в качестве возможной альтернативной стратегии терапии гипофункции трансплантата после алло-ТГСК. В данной работе представлен опыт использования агонистов рецептора тромбопоэтина для лечения посттрансплантационных цитопений, в том числе критериальной тяжелой гипофункции трансплантата после алло-ТГСК в нашем центре.
В общей сложности 31 пациент (15 мужчин, 16 женщин) со средним возрастом 22 года (18-57) получили терапию агонистами рецептора ТПО (АР-ТПО) для посттрансплантационной тромбоцитопении <20×109/л (n=7) и ГФТ (n=24). Для терапии использовался ромиплостим (n=17) со средней дозой 5 мкг/кг в неделю (3-5) или элтромбопаг (n=14) со средней дозой 50 мг/день (50-150). Критериями тяжелой гипофункции трансплантата (тГФТ) были: цитопения в двух или более миелоидных линиях (тромбоциты <20×109/л, абсолютное число нейтрофилов (АЧН) <0,5×109/л, гемоглобин <70 г/л в любое время после документированного приживления, полный или стабильный смешанный донорский химеризм >90% без признаков рецидива основного заболевания. Общий ответ включал полный ответ (ПО) (тромбоциты ≥100×109/л, АЧН ≥1,5×109/л, гемоглобин ≥100 г/л) и частичный ответ (ЧО) (тромбоциты >20×109/л, АЧН ≥0,5×109/л, гемоглобин >70 г/л). Медиана времени от постановки диагноза тГФТ до начала терапии АР-ТПО составила 14 дней (0-119), медиана продолжительности терапии АР-ТПО составила 3 недели (1-43). Переносимость АР-ТПО была удовлетворительной, без признаков токсичности II-IV степени. В общей сложности в 8 случаях (28%) АР-ТПО использовались в комбинации с ритуксимабом (n=4), ритуксимабом и инфузиями донорских лимфоцитов (ИДЛ) (n=3), а также с инфузиями CD34-клеток (n=1). Всего 14 (48%) пациентов достигли ответа (ПО: n=4, 14%; ЧО: n=10, 34%). Комбинированная терапия не показала преимущества в скорости ответа по сравнению с АР-ТПО в монорежиме. Медиана прироста АЧН у ответивших на терапию составила 3,4×109/л (0,8-6,0), тромбоцитов – 48×109/л (21-205). В общей сложности 15 пациентов (3 ответивших, 12 не ответивших на терапию) умерли от инфекции (n=10), рецидива (n=2) и острой реакции «трансплантат-против-хозяина» (оРТПХ) III-IV степени (n=3). Однолетняя общая выживаемость (ОВ) от начала терапии составила 60% (95% ДИ, 40-76), при этом наблюдалась существенная разница между ответившими и неответившими на АР-ТПО: 79% (95% ДИ, 47-93) против 39% (95% ДИ, 14-63) (р=0,01). Наше исследование показало многообещающую эффективность и удовлетворительную безопасность АР-ТПО у пациентов с тГФТ после алло-ТГСК. Необходимо проведение многоцентровых проспективных исследований для установления оптимальной дозы и продолжительности приема, а также критериев отмены этих препаратов.
Ключевые слова
Алло-ТГСК, гипофункция трансплантата, агонисты рецепторов тромбопоэтина.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22297
[VALUE] => 10.18620/ctt-1866-8836-2019-8-2-38-44
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2019-8-2-38-44
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22313
[VALUE] => Array
(
[TEXT] => <p>Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22314
[VALUE] => Array
(
[TEXT] => <p>Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22331
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT. </p>
<p style="text-align: justify;">A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×10<sup>9</sup>/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×10<sup>9</sup>/l, absolute neutrophil count (ANC) <0.5×10<sup>9</sup>/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×10<sup>9</sup>/l, ANC ≥1.5×10<sup>9</sup>/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×10<sup>9</sup>/l, ANC ≥0.5×10<sup>9</sup>/l, hemoglobin >70 g/l).
Median time from diagnosis of sPGF to the start of
TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×10<sup>9</sup>/l (0.8-6.0), platelets – 48×10<sup>9</sup>/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) <i>vs</i> 39% (95% CI, 14-63) (p=0.01). </p>
<p style="text-align: justify;">Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.</p>
<h2>Keywords</h2>
<p style="text-align: justify;">Allo-HSCT, poor graft function, thrombopoietin receptor agonists.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT.
A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×109/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×109/l, absolute neutrophil count (ANC) <0.5×109/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×109/l, ANC ≥1.5×109/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×109/l, ANC ≥0.5×109/l, hemoglobin >70 g/l).
Median time from diagnosis of sPGF to the start of
TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×109/l (0.8-6.0), platelets – 48×109/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) vs 39% (95% CI, 14-63) (p=0.01).
Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.
Keywords
Allo-HSCT, poor graft function, thrombopoietin receptor agonists.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22298
[VALUE] => Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Thrombopoietin receptor agonists for treatment of poor graft function after allogeneic hematopoietic stem cell transplantation in adults
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22299
[VALUE] => 1645
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1645
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22315
[VALUE] => 1646
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1646
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Tatiana A. Rudakova, Alexander D. Kulagin, Ivan S. Moiseev, Tatyana A. Bykova, Sergey N. Bondarenko, Maria V. Barabanshikova, Anastasia V. Beinarovich, Anna A. Osipova, Varvara N. Ovechkina, Alexander L. Alyanskiy, Elena I. Darskaya, Elena V. Morozova, Boris V. Afanasyev
Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Chair of Hematology, Transfusiology and Transplantology, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
Posttransplant cytopenias due to poor graft function (PGF) are a severe complication of allogeneic transplantation of hematopoietic stem cells (allo-HSCT). Conventional therapeutic options for poor graft function are limited to infusions of CD34-selected cells. However, having shown encouraging results in idiopathic thrombocytopenia and aplastic anemia, thrombopoietin receptor agonists (TPO-RA) romiplostim and eltrombopag might be a possible alternative treatment strategy for PGF after allo-HSCT. Current study aims to summarize single-center experience of TPO-RA for treatment of posttransplant cytopenias including PGF after allo-HSCT.
A total of 31 patients (15 males, 16 females) with median age of 22 years (18-57) received therapy with TPO agonists for posttransplant thrombocytopenia <20×109/l (n=7) and PGF (n=24). Romiplostim (n=17) with the median dose 5 mkg/kg weekly (3-5) or eltrombopag (n=14) with the median dose 50 mg/day (50-150) were used. Criteria for severe poor graft function (sPGF) were the following: cytopenia in two or more myeloid lineages (platelets <20×109/l, absolute neutrophil count (ANC) <0.5×109/l, hemoglobin <70 g/l) any time after documented engraftment, full or stable mixed donor chimerism >90% without signs of relapse of underlying disease. Overall response included complete response (CR) (platelets ≥100×109/l, ANC ≥1.5×109/l, hemoglobin ≥100 g/l) and partial response (PR) (platelets >20×109/l, ANC ≥0.5×109/l, hemoglobin >70 g/l). Median time from diagnosis of sPGF to the start of TPO-RA therapy was 14 days (0-119), median length of TPO-RA therapy was 3 weeks (1-43). TPO-RA was well tolerated, with no signs of II-IV grade toxicity. In a total of 8 cases (28%) TPO-RA were used in combination with rituximab (n=4), rituximab and donor lymphocyte infusions (DLI) (n=3), as well as CD34-cell infusions (n=1). A total of 14 (48%) patients achieved response (CR: n=4, 14%; PR: n=10, 34%). Combination therapy showed no advantage in response rate compared to TPO-RA alone. Median increase of ANC in responders was 3.4×109/l (0.8-6.0), platelets – 48×109/l (21-205). A total of 15 patients (3 responders, 12 non-responders) died of infection (n=10), relapse (n=2) and acute graft-versus-host disease (aGVHD) III-IV grade (n=3). One-year overall survival (OS) from the therapy start was 60% (95% CI, 40-76), with a significant difference between responders and non-responders: 79% (95% CI, 47-93) vs 39% (95% CI, 14-63) (p=0.01).
Our study showed a promising efficacy and safety of TPO-RA in patients with sPGF after allo-HSCT. Multicenter prospective studies are needed to establish optimal dose and duration of the drug administration, as well as the criteria for discontinuation of these drugs.
Keywords
Allo-HSCT, poor graft function, thrombopoietin receptor agonists.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22255
[VALUE] => 05/08/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 05/08/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22256
[VALUE] => 06/28/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 06/28/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22257
[VALUE] => 361
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 361
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22271
[VALUE] => Array
(
[TEXT] => <p>Алена И. Шакирова, Николай Н. Мамаев, Ильдар М. Бархатов, Яна В. Гудожникова, Татьяна Л. Гиндина,
Елена В. Бабенко, Борис В. Афанасьев</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Алена И. Шакирова, Николай Н. Мамаев, Ильдар М. Бархатов, Яна В. Гудожникова, Татьяна Л. Гиндина,
Елена В. Бабенко, Борис В. Афанасьев
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22272
[VALUE] => Array
(
[TEXT] => <p>НИИ детской онкологии, гематологии и трансплантации им. Р. М. Горбачевой; кафедра гематологии, трансфузиологии и трансплантологии Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова, Санкт-Петербург, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => НИИ детской онкологии, гематологии и трансплантации им. Р. М. Горбачевой; кафедра гематологии, трансфузиологии и трансплантологии Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова, Санкт-Петербург, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22273
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Цель изучения состояла в выяснении тесных связей между популяциями костномозговых бластных элементов, повышение содержания которых определяет цитологический рецидив ОМЛ, и ответственных за рецидив лейкозных клеток предшественников. В клиническом плане, мы имели целью оценку потенциала развития рецидивов лейкоза после трансплантации гемопоэтических клеток (ТГСК). Посттрансплантационные рецидивы (ПТР), с точки зрения их биологических механизмов, могут выявляться по гиперэкспрессии определенных генов, связанных с клеточной дифференцировкой.</p>
<h3>Пациенты и методы</h3>
<p style="text-align: justify;">В исследование вошло 61 больных ОМЛ, леченных с помощью алло-ТГСК, у которых осуществлено одновременное серийное измерение уровней экспрессии генов <i>BAALC</i> и <i>WT1</i> методом количественной ПЦР в реальном времени с использованием ген-специфических праймеров.</p>
<h3>Результаты</h3>
<p style="text-align: justify;">В группе из 12 больных с повышенным уровнем экспрессии гена <i>WT1</i> и с нормализованным до 4 % содержанием бластных элементов в костном мозге на момент проведения аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК) было показано, что подгруппа с повышенной экспрессией гена <i>BAALC</i> характеризуется: а) более высоким числом ПТР (р=0,002); а также б) укорочением сроков безрецидивной выживаемости (БРВ) при сопоставлении с группой сравнения (р=0,019). Дальнейшее использование этого прогностически неблагоприятного критерия, состоящего из одновременного повышения уровней экспрессии обоих генов при анализе основного массива данных, показало его более частое обнаружение у больных с М1, М2, М0, М4 и М5 ФАБ- цитологическими вариантами. При этом предварительные данные указывают на худшую общую выживаемость (228 дней) в группе больных ОМЛ, имевших сочетанную гиперэкспрессию обоих генов как непосредственно перед ТГСК, так и в посттрансплантационном периоде. </p>
<h3>Заключение</h3>
<p style="text-align: justify;">Потенциальная клиническая значимость полученных данных, касающихся повышенной экспрессии гена <i>BAALC</i> у взрослых и детей больных ОМЛ, леченных с использованием алло-ТГСК, и особенно, наличия феномена сочетания у них гиперэкспрессии генов <i>BAALC</i> и <i>WT1</i> несомненна, что диктует необходимость активного использования их в клинике. </p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Острый миелоидный лейкоз, аллогенная трансплантация гемопоэтических клеток, посттрансплантационные рецидивы, гены <i>BAALC</i> и <i>WT1</i>, одновременная гиперэкспрессия, клиническая значимость, прогноз.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Цель изучения состояла в выяснении тесных связей между популяциями костномозговых бластных элементов, повышение содержания которых определяет цитологический рецидив ОМЛ, и ответственных за рецидив лейкозных клеток предшественников. В клиническом плане, мы имели целью оценку потенциала развития рецидивов лейкоза после трансплантации гемопоэтических клеток (ТГСК). Посттрансплантационные рецидивы (ПТР), с точки зрения их биологических механизмов, могут выявляться по гиперэкспрессии определенных генов, связанных с клеточной дифференцировкой.
Пациенты и методы
В исследование вошло 61 больных ОМЛ, леченных с помощью алло-ТГСК, у которых осуществлено одновременное серийное измерение уровней экспрессии генов BAALC и WT1 методом количественной ПЦР в реальном времени с использованием ген-специфических праймеров.
Результаты
В группе из 12 больных с повышенным уровнем экспрессии гена WT1 и с нормализованным до 4 % содержанием бластных элементов в костном мозге на момент проведения аллогенной трансплантации гемопоэтических стволовых клеток (алло-ТГСК) было показано, что подгруппа с повышенной экспрессией гена BAALC характеризуется: а) более высоким числом ПТР (р=0,002); а также б) укорочением сроков безрецидивной выживаемости (БРВ) при сопоставлении с группой сравнения (р=0,019). Дальнейшее использование этого прогностически неблагоприятного критерия, состоящего из одновременного повышения уровней экспрессии обоих генов при анализе основного массива данных, показало его более частое обнаружение у больных с М1, М2, М0, М4 и М5 ФАБ- цитологическими вариантами. При этом предварительные данные указывают на худшую общую выживаемость (228 дней) в группе больных ОМЛ, имевших сочетанную гиперэкспрессию обоих генов как непосредственно перед ТГСК, так и в посттрансплантационном периоде.
Заключение
Потенциальная клиническая значимость полученных данных, касающихся повышенной экспрессии гена BAALC у взрослых и детей больных ОМЛ, леченных с использованием алло-ТГСК, и особенно, наличия феномена сочетания у них гиперэкспрессии генов BAALC и WT1 несомненна, что диктует необходимость активного использования их в клинике.
Ключевые слова
Острый миелоидный лейкоз, аллогенная трансплантация гемопоэтических клеток, посттрансплантационные рецидивы, гены BAALC и WT1, одновременная гиперэкспрессия, клиническая значимость, прогноз.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22265
[VALUE] => 10.18620/ctt-1866-8836-2019-8-2-45-57
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2019-8-2-45-57
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22267
[VALUE] => Array
(
[TEXT] => <p>
Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko, <br>Boris V. Afanasyev
</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] =>
Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko,
Boris V. Afanasyev
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22276
[VALUE] => Array
(
[TEXT] => <p>Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22277
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of <i>WT1</i> and <i>BAALC</i> molecular markers expressed by appropriate cell types. In clinical terms, we sought to evaluate a potential for evolving leukemia relapses following hematopoietic stem cell transplantation (HSCT). The post-transplant relapses (PTR), in view of their biological mechanisms, may be detected by overexpression of distinct differentiation-related genes.</p>
<h3>Patients and methods</h3>
<p style="text-align: justify;">We have done parallel serial measurements of <i>BAALC</i> and <i>WT1</i> gene expression in bone marrow cells of the patients with acute myeloid leukemia, using quantitative real-time PCR (qPCR) with gene-specific primers.</p>
<h3>Results</h3>
<p style="text-align: justify;">An initial pilot study was carried out in twelve patients with elevated <i>WT1</i> expression levels and normal blast counts (<5%) in bone marrow at the time of allogeneic HSCT. It has shown that the relapse occurrence and shorter relapse-free survival (RFS) post-transplant were more common in the subgroup with higher <i>BAALC</i> gene expression level as compared to those without <i>BAALC</i> expression elevation (p=0.002, and p=0.019, respectively). Moreover, when analyzing the validating patient cohort, we have found that the simultaneous elevation of both <i>BAALC</i> and <i>WT1</i> expression, known as unfavorable prognostic factor, was more frequently observed in the patients with AML М1, М2, and М0 FAB-variants. Preliminary results show an inferior overall survival
(a mean of 228 days) in AML patients with combined overexpression of the both genes immediately before HSCT, like as in post-transplant period. In conclusion, it should be noted that our findings of simultaneous overexpressions of <i>BAALC</i> and <i>WT1</i> genes in great cohort of adults and children patients with different FAB- variants of AML treated by means of allo-HSCT were revealed for the first time. Being associated with poor prognosis, this double test should be used actively for post-transplant monitoring of all patients with AML. </p>
<h2>Keywords</h2>
<p style="text-align: justify;">Acute myeloblastic leukemia, hematopoietic stem cell transplantation, allogeneic, post-transplant relapses, <i>BAALC</i>, <i>WT1</i>, gene overexpression, parallel assays, relapse risk, prognostic value. </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of WT1 and BAALC molecular markers expressed by appropriate cell types. In clinical terms, we sought to evaluate a potential for evolving leukemia relapses following hematopoietic stem cell transplantation (HSCT). The post-transplant relapses (PTR), in view of their biological mechanisms, may be detected by overexpression of distinct differentiation-related genes.
Patients and methods
We have done parallel serial measurements of BAALC and WT1 gene expression in bone marrow cells of the patients with acute myeloid leukemia, using quantitative real-time PCR (qPCR) with gene-specific primers.
Results
An initial pilot study was carried out in twelve patients with elevated WT1 expression levels and normal blast counts (<5%) in bone marrow at the time of allogeneic HSCT. It has shown that the relapse occurrence and shorter relapse-free survival (RFS) post-transplant were more common in the subgroup with higher BAALC gene expression level as compared to those without BAALC expression elevation (p=0.002, and p=0.019, respectively). Moreover, when analyzing the validating patient cohort, we have found that the simultaneous elevation of both BAALC and WT1 expression, known as unfavorable prognostic factor, was more frequently observed in the patients with AML М1, М2, and М0 FAB-variants. Preliminary results show an inferior overall survival
(a mean of 228 days) in AML patients with combined overexpression of the both genes immediately before HSCT, like as in post-transplant period. In conclusion, it should be noted that our findings of simultaneous overexpressions of BAALC and WT1 genes in great cohort of adults and children patients with different FAB- variants of AML treated by means of allo-HSCT were revealed for the first time. Being associated with poor prognosis, this double test should be used actively for post-transplant monitoring of all patients with AML.
Keywords
Acute myeloblastic leukemia, hematopoietic stem cell transplantation, allogeneic, post-transplant relapses, BAALC, WT1, gene overexpression, parallel assays, relapse risk, prognostic value.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22266
[VALUE] => Clinical significance of BAALC overexpression for predicting post-transplant relapses in acute myeloid leukemia
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Clinical significance of BAALC overexpression for predicting post-transplant relapses in acute myeloid leukemia
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22274
[VALUE] => 1628
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1628
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22275
[VALUE] => 1629
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1629
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Alena I. Shakirova, Nikolay N. Mamaev, Ildar M. Barkhatov, Yana V. Gudozhnikova, Tatiana L. Gindina, Elena V. Babenko,
Boris V. Afanasyev
Raisa Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation, Pavlov First Saint Petersburg State Medical University, St. Petersburg, Russia
The aim of this study was to clarify close associations between population of bone marrow blast elements defining cytological relapse, and that of leukemic precursor cells by means of serial quantitative measurement of WT1 and BAALC molecular markers expressed by appropriate cell types. In clinical terms, we sought to evaluate a potential for evolving leukemia relapses following hematopoietic stem cell transplantation (HSCT). The post-transplant relapses (PTR), in view of their biological mechanisms, may be detected by overexpression of distinct differentiation-related genes.
Patients and methods
We have done parallel serial measurements of BAALC and WT1 gene expression in bone marrow cells of the patients with acute myeloid leukemia, using quantitative real-time PCR (qPCR) with gene-specific primers.
Results
An initial pilot study was carried out in twelve patients with elevated WT1 expression levels and normal blast counts (<5%) in bone marrow at the time of allogeneic HSCT. It has shown that the relapse occurrence and shorter relapse-free survival (RFS) post-transplant were more common in the subgroup with higher BAALC gene expression level as compared to those without BAALC expression elevation (p=0.002, and p=0.019, respectively). Moreover, when analyzing the validating patient cohort, we have found that the simultaneous elevation of both BAALC and WT1 expression, known as unfavorable prognostic factor, was more frequently observed in the patients with AML М1, М2, and М0 FAB-variants. Preliminary results show an inferior overall survival (a mean of 228 days) in AML patients with combined overexpression of the both genes immediately before HSCT, like as in post-transplant period. In conclusion, it should be noted that our findings of simultaneous overexpressions of BAALC and WT1 genes in great cohort of adults and children patients with different FAB- variants of AML treated by means of allo-HSCT were revealed for the first time. Being associated with poor prognosis, this double test should be used actively for post-transplant monitoring of all patients with AML.
Keywords
Acute myeloblastic leukemia, hematopoietic stem cell transplantation, allogeneic, post-transplant relapses, BAALC, WT1, gene overexpression, parallel assays, relapse risk, prognostic value.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22170
[VALUE] => 05/16/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 05/16/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22171
[VALUE] => 06/26/2019 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 06/26/2019 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22172
[VALUE] => 1653
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1653
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] => Array
(
[0] => 22483
[1] => 22484
[2] => 22485
[3] => 22486
[4] => 22487
[5] => 22488
[6] => 22489
[7] => 22490
)
[VALUE] => Array
(
[0] => 1653
[1] => 1654
[2] => 1655
[3] => 1656
[4] => 1657
[5] => 1658
[6] => 1659
[7] => 1660
)
[DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
)
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[0] => 1653
[1] => 1654
[2] => 1655
[3] => 1656
[4] => 1657
[5] => 1658
[6] => 1659
[7] => 1660
)
[~DESCRIPTION] => Array
(
[0] =>
[1] =>
[2] =>
[3] =>
[4] =>
[5] =>
[6] =>
[7] =>
)
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22181
[VALUE] => Array
(
[TEXT] => <p>Галина В. Федотовских, Галия М. Шаймарданова, Манарбек Б. Аскаров, Майя С. Жумабаева, Гульмира С. Досатаева, Айгерим К. Смагулова, Сапаргуль Марат, Татьяна Г. Ежеленко</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Галина В. Федотовских, Галия М. Шаймарданова, Манарбек Б. Аскаров, Майя С. Жумабаева, Гульмира С. Досатаева, Айгерим К. Смагулова, Сапаргуль Марат, Татьяна Г. Ежеленко
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22182
[VALUE] => Array
(
[TEXT] => <p>АО «Национальный научный медицинский центр», г. Нур-Cултан (Астана), Казахстан </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => АО «Национальный научный медицинский центр», г. Нур-Cултан (Астана), Казахстан
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22183
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Применение мезенхимных стволовых клеток костного мозга (МСК) при воспалительных заболеваниях кишечника показало свою выполнимость в клинических исследованиях. Целью настоящей работы было исследование морфо-функционального состояния слизистой толстого кишечника в срок 10 мес. после единичной инфузии культивированных <i>in vitro</i> и размноженных МСК в дополнение к стандартной терапии больных с язвенным колитом (ЯК).</p>
<h3>Материалы и методы</h3>
<p style="text-align: justify;">Исходная группа пациентов с ЯК включала 18 человек. Девять из них получали стандартную терапию (контрольная группа), а шесть человек проходили аналогичное лечение с добавлением разовой трансплантацией аутологичных МСК (экспериментальная группа). Клиническое и функциональное состояние пациентов оценивали по индексам Truelove и Wiits, а также Mayo и Rakhmilevich. Рутинная световая микроскопия, а также электронно-микроскопические (ЭМ) исследования проводили для 320 биоптатов слизистой толстого кишечника (СТК). Специфическое гистологическое и иммуногистохимическое обследование выполнено в 64 образцах. Гистологические признаки воспалительной активности оценивали в баллах по K.Geboes et al. Иммуногистохимические исследования включали анализ экспрессии маркеров CD4, CD68, CD31, CD34, CD8, IgG и Ki-67. ЭМ проводили по общепринятой методике. Полутонкие срезы окрашивали по Humphrey и Pittman. Ультратонкие срезы изучали и локализовали с помощью электронного микроскопа Libra 120. </p>
<h3>Результаты</h3>
<p style="text-align: justify;">Разовая трансплантация аутологичных культивированных МСК костного мозга в добавление к стандартной терапии больных с ЯК, в целом, улучшали клинические и лабораторные симптомы заболевания при исследовании через 10 мес. после лечения при сравнении с исходным клиническим статусом и контрольной группой. При морфологическом исследовании СТК в обеих группах была отмечена персистенция или некоторое уменьшение эрозивных и язвенных дефектов. Показатели позитивной динамики структуры СТК проявлялись, главным образом, у пациентов экспериментальной группы в виде снижения воспалительной реакции и восстановления кишечных крипт (<i>“эпителиальной ниши”</i>), с увеличением числа goblet-клеток и сниженной проницаемостью кишечного покровного эпителия.</p>
<h3>Заключение</h3>
<p style="text-align: justify;">Разовая трансплантация аутологичных культивированных МСК костного мозга может быть внедрена в стандартную терапию пациентов с ЯК, что оказывает позитивный эффект на морфофунциональное состояние СТК, тем самым способствуя снижению воспалительной реакции, восстановлению крипт и покровного эпителия. </p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Язвенный колит, аутологичная трансплантация костного мозга, мезенхимные клетки, трансплантация, кишечные крипты, морфология.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Применение мезенхимных стволовых клеток костного мозга (МСК) при воспалительных заболеваниях кишечника показало свою выполнимость в клинических исследованиях. Целью настоящей работы было исследование морфо-функционального состояния слизистой толстого кишечника в срок 10 мес. после единичной инфузии культивированных in vitro и размноженных МСК в дополнение к стандартной терапии больных с язвенным колитом (ЯК).
Материалы и методы
Исходная группа пациентов с ЯК включала 18 человек. Девять из них получали стандартную терапию (контрольная группа), а шесть человек проходили аналогичное лечение с добавлением разовой трансплантацией аутологичных МСК (экспериментальная группа). Клиническое и функциональное состояние пациентов оценивали по индексам Truelove и Wiits, а также Mayo и Rakhmilevich. Рутинная световая микроскопия, а также электронно-микроскопические (ЭМ) исследования проводили для 320 биоптатов слизистой толстого кишечника (СТК). Специфическое гистологическое и иммуногистохимическое обследование выполнено в 64 образцах. Гистологические признаки воспалительной активности оценивали в баллах по K.Geboes et al. Иммуногистохимические исследования включали анализ экспрессии маркеров CD4, CD68, CD31, CD34, CD8, IgG и Ki-67. ЭМ проводили по общепринятой методике. Полутонкие срезы окрашивали по Humphrey и Pittman. Ультратонкие срезы изучали и локализовали с помощью электронного микроскопа Libra 120.
Результаты
Разовая трансплантация аутологичных культивированных МСК костного мозга в добавление к стандартной терапии больных с ЯК, в целом, улучшали клинические и лабораторные симптомы заболевания при исследовании через 10 мес. после лечения при сравнении с исходным клиническим статусом и контрольной группой. При морфологическом исследовании СТК в обеих группах была отмечена персистенция или некоторое уменьшение эрозивных и язвенных дефектов. Показатели позитивной динамики структуры СТК проявлялись, главным образом, у пациентов экспериментальной группы в виде снижения воспалительной реакции и восстановления кишечных крипт (“эпителиальной ниши”), с увеличением числа goblet-клеток и сниженной проницаемостью кишечного покровного эпителия.
Заключение
Разовая трансплантация аутологичных культивированных МСК костного мозга может быть внедрена в стандартную терапию пациентов с ЯК, что оказывает позитивный эффект на морфофунциональное состояние СТК, тем самым способствуя снижению воспалительной реакции, восстановлению крипт и покровного эпителия.
Ключевые слова
Язвенный колит, аутологичная трансплантация костного мозга, мезенхимные клетки, трансплантация, кишечные крипты, морфология.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22184
[VALUE] => 10.18620/ctt-1866-8836-2019-8-2-58-62
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2019-8-2-58-62
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22195
[VALUE] => Array
(
[TEXT] => <p>Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22196
[VALUE] => Array
(
[TEXT] => <p>National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 22197
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured <i>in vitro</i> expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).</p>
<h3>Materials and methods</h3>
<p style="text-align: justify;">Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.</p>
<h3>Results</h3>
<p style="text-align: justify;">A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.</p>
<h3>Conclusion</h3>
<p style="text-align: justify;">Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.</p>
<h2>Keywords</h2>
<p style="text-align: justify;">Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured in vitro expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).
Materials and methods
Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.
Results
A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.
Conclusion
Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.
Keywords
Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22185
[VALUE] => Efficiency of mesenchymal stem cell therapy in ulcerative colitis as assessed by the morphology of colon mucosa
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Efficiency of mesenchymal stem cell therapy in ulcerative colitis as assessed by the morphology of colon mucosa
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22186
[VALUE] => 1625
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1625
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 22198
[VALUE] => 1626
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 1626
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Galina V. Fedotovskikh, Galija M. Shaymardanova, Manarbek B. Askarov, Maiya S. Zhumabayeva, Gulmira S. Dosataeva, Aigerim K. Smagulova, Sapargul Marat, Tatyana G. Ezhelenko
National Scientific Medical Center, Nur-Sultan (Astana), Kazakhstan
Usage of bone marrow mesenchymal stromal cells (MSCs) in human inflammatory bowel disease has proven its feasibility in clinical studies. The purpose of this work was to study morpho-functional state of large intestine mucosa (LIM) at the term of 10 months after a single infusion of cultured in vitro expanded mesenchymal bone marrow cells (MSC) added to standard therapy of patients with ulcerative colitis (UC).
Materials and methods
Initial group of the patients with UC included 18 subjects. Of those, nine patients received standard drug therapy (control group), six subjects underwent similar therapy supplied by a single transplantation of autologous MSCs (the study group). Clinical and functional state of the patients was assessed by indices, according to Truelove and Wiits, Mayo and Rakhmilevich. Routine light microscopy, as well as electron microscopic studies were performed for 320 large intestinal mucosa (LIM) biopsies. Specific histological and immunohistochemical examination was carried out in 64 samples. Histological signs of inflammatory activity were evaluated in points according to K.Geboes et al. (2000). Immunohistochemistry studies included expression of CD4, CD68, CD31, CD34, CD8, lgG, and Ki-67 markers. The electron microscopic technique was used as generally accepted. Semi-thin sections were stained by C. Humphrey and F. Pittman (1974). Ultrathin sections were observed and captured using a Libra 120 electron microscope.
Results
A single transplantation of autologous cultured bone marrow MSCs, in addition to standard therapy of patients with ulcerative colitis has generally improved clinical and laboratory signs of the disease as examined 10 months after treatment, when compared with initial clinical state and the control group. Upon morphological study of LIM in the study and control groups, erosive and ulcerative defects did persist or were slightly decreased. Indicators of positive dynamics in the LIM structure have manifested mainly in the patients of study group, as a decreased inflammatory response and restoration of intestinal crypts (“epithelial niche”), with increased number of goblet cells and decreased permeability of intestinal cover epithelium.
Conclusion
Single transplantation of autologous cultured bone marrow MSC could be implemented into the standard therapy of patients with ulcerative colitis, providing a positive effect upon morpho-functional state of LIM, thus promoting reduction of inflammatory response, recovery of crypts and cover epithelium.
Keywords
Ulcerative colitis, autologous bone marrow, mesenchymal cells, transplantation, intestinal crypts, morphology.

