Since 70s, Prof. Vladimir A. Almazov became Head of the Chair. Since that time, the studies of leukemogenesis were launched here by new generation of clinical hematologists headed by Boris V. Afanasyev. The ex vivo cultures of colony-forming units of granulocyte-macrophage progenitor cells allowed them to get the first evidence for intrinsic factors of granulo-monocytopoiesis in acute leukemia, chronic myeloid leukemia, especially in different blast crisis types, myelodysplastic syndromes in adults, along with pioneering studies of aplastic anemia in children. The summarized data were published in Progenitor Hematopoietic Human Cells (1985), the first monograph in this field.
The notorious Chernobyl nuclear accident (1986) has promoted studies in the area of acute cytostatic syndrome in USSR and abroad. Boris Afanasyev, who worked at the Pavlov Medical Institute, was sent to Seattle for training at the famous clinic by E. Donnal Thomas, the Nobel Prize winner of 1990 for successful transplantation of hematopoietic cells in human patients. Several years later, by the initiative of Prof. Boris Afanasyev, the University management has arranged the Department of Bone Marrow Transplantation at the Pavlov University (1997) where the implementation of program for different types of hematopoietic stem cell transplantation was started in children and adults.
One should note the extensive clinical aid and consultative efforts from our foreign friends and colleagues in the field of leukemia treatment protocols, immunological typing, leukemia diagnostics and treatment schedules. This support was extremely important during 1990-1996, at the earlier steps of our BMT activity. The Hematology, Oncology and HSCT units at the Pavlov University could not succeed in the field without stable professional contacts with outstanding experts from Europe and USA. We should be appreciated, first of all, to close cooperation with Hamburg University (Germany) arranged by Prof. R. Neth, A. Zander, Th. Büchner, other German leading specialists – Prof. H.-J. Kolb, D. Hoelzer, B. Fehse. The leading specialists from other countries were also involved into these cooperative efforts, e.g., Prof. R. Gale (USA), Prof. G. Wagemaker (The Netherlands), Prof. A. Bacigalupo (Italy) and many other renown clinicians. Prof. Axel Zander, Axel Fauser, Gerard Wagemaker, Dieter Hoelzer were awarded the titles of Doctor Honoris Causa at the Pavlov University due to their merits in cooperation with Russian specialists in the field.
In the last 15 years, the development of hematology at the University is associated with RM Gorbacheva Memorial Research Institute organized by Prof. B. V. Afanasyev, being among the most active BMT centers in the Europe. During this period, over 4500 allogeneic and autologous transplants were performed in children and adults with leukemia, lymphomas, multiple myeloma, aplastic anemia, immunodeficiencies, solid tumors and metabolic disorders. The staff of the Institute conducts experimental and clinical research in the field of leukemia, myeloproliferative diseases, lymphomas, myeloma, bone marrow failure and other areas of hematology.
The Journal Cellular Therapy and Transplantation (CTT) is a joint project of German and Russian specialists in BMT and oncohematology, being issued since 2008. CTT publishes original data in hematopoietic stem cell transplantation, cellular and immunotherapy, gene therapy and adjacent areas of medicine and biology. We hope that clinical, research and publishing activities in this field will further develop at the Pavlov University, in close cooperation with our Russian and foreign colleagues for the benefit of patients with leukemia and other severe disorders that may be cured now by modern therapeutic approaches.
" ["~DETAIL_TEXT"]=> string(4038) "
Since 70s, Prof. Vladimir A. Almazov became Head of the Chair. Since that time, the studies of leukemogenesis were launched here by new generation of clinical hematologists headed by Boris V. Afanasyev. The ex vivo cultures of colony-forming units of granulocyte-macrophage progenitor cells allowed them to get the first evidence for intrinsic factors of granulo-monocytopoiesis in acute leukemia, chronic myeloid leukemia, especially in different blast crisis types, myelodysplastic syndromes in adults, along with pioneering studies of aplastic anemia in children. The summarized data were published in Progenitor Hematopoietic Human Cells (1985), the first monograph in this field.
The notorious Chernobyl nuclear accident (1986) has promoted studies in the area of acute cytostatic syndrome in USSR and abroad. Boris Afanasyev, who worked at the Pavlov Medical Institute, was sent to Seattle for training at the famous clinic by E. Donnal Thomas, the Nobel Prize winner of 1990 for successful transplantation of hematopoietic cells in human patients. Several years later, by the initiative of Prof. Boris Afanasyev, the University management has arranged the Department of Bone Marrow Transplantation at the Pavlov University (1997) where the implementation of program for different types of hematopoietic stem cell transplantation was started in children and adults.
One should note the extensive clinical aid and consultative efforts from our foreign friends and colleagues in the field of leukemia treatment protocols, immunological typing, leukemia diagnostics and treatment schedules. This support was extremely important during 1990-1996, at the earlier steps of our BMT activity. The Hematology, Oncology and HSCT units at the Pavlov University could not succeed in the field without stable professional contacts with outstanding experts from Europe and USA. We should be appreciated, first of all, to close cooperation with Hamburg University (Germany) arranged by Prof. R. Neth, A. Zander, Th. Büchner, other German leading specialists – Prof. H.-J. Kolb, D. Hoelzer, B. Fehse. The leading specialists from other countries were also involved into these cooperative efforts, e.g., Prof. R. Gale (USA), Prof. G. Wagemaker (The Netherlands), Prof. A. Bacigalupo (Italy) and many other renown clinicians. Prof. Axel Zander, Axel Fauser, Gerard Wagemaker, Dieter Hoelzer were awarded the titles of Doctor Honoris Causa at the Pavlov University due to their merits in cooperation with Russian specialists in the field.
In the last 15 years, the development of hematology at the University is associated with RM Gorbacheva Memorial Research Institute organized by Prof. B. V. Afanasyev, being among the most active BMT centers in the Europe. During this period, over 4500 allogeneic and autologous transplants were performed in children and adults with leukemia, lymphomas, multiple myeloma, aplastic anemia, immunodeficiencies, solid tumors and metabolic disorders. The staff of the Institute conducts experimental and clinical research in the field of leukemia, myeloproliferative diseases, lymphomas, myeloma, bone marrow failure and other areas of hematology.
The Journal Cellular Therapy and Transplantation (CTT) is a joint project of German and Russian specialists in BMT and oncohematology, being issued since 2008. CTT publishes original data in hematopoietic stem cell transplantation, cellular and immunotherapy, gene therapy and adjacent areas of medicine and biology. We hope that clinical, research and publishing activities in this field will further develop at the Pavlov University, in close cooperation with our Russian and foreign colleagues for the benefit of patients with leukemia and other severe disorders that may be cured now by modern therapeutic approaches.
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "10" ["~SORT"]=> string(2) "10" ["CODE"]=> string(66) "universitet-im-akad-i-p-pavlova-125-let-issledovaniy-v-gematologii" ["~CODE"]=> string(66) "universitet-im-akad-i-p-pavlova-125-let-issledovaniy-v-gematologii" ["EXTERNAL_ID"]=> string(4) "2049" ["~EXTERNAL_ID"]=> string(4) "2049" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(172) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологииPavlov University: 125 years in blood research" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(2396) "<p style="text-align: justify;">В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением <sup>59</sup>Fe и других радиоактивных изотопов.</p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_META_TITLE"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_META_KEYWORDS"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_META_DESCRIPTION"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_PICTURE_FILE_ALT"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_PICTURE_FILE_TITLE"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_PICTURE_FILE_NAME"]=> string(70) "universitet-im-akad-i-p-pavlova-125-let-issledovaniy-v-gematologii-img" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(126) "Университет им. акад. И. П. Павлова: 125 лет исследований в гематологии" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(70) "universitet-im-akad-i-p-pavlova-125-let-issledovaniy-v-gematologii-img" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(70) "universitet-im-akad-i-p-pavlova-125-let-issledovaniy-v-gematologii-img" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(70) "universitet-im-akad-i-p-pavlova-125-let-issledovaniy-v-gematologii-img" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "205" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28495" ["VALUE"]=> array(2) { ["TEXT"]=> string(221) "<p>Профессор Александр Д. Кулагин, главный редактор журнала <i>«Клеточная Терапия и Трансплантация» (СТТ)</i></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(197) "
Профессор Александр Д. Кулагин, главный редактор журнала «Клеточная Терапия и Трансплантация» (СТТ)
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_RU"]=> array(36) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28496" ["VALUE"]=> array(2) { ["TEXT"]=> string(2396) "<p style="text-align: justify;">В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением <sup>59</sup>Fe и других радиоактивных изотопов.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2362) "В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением 59Fe и других радиоактивных изотопов.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28497" ["VALUE"]=> array(2) { ["TEXT"]=> string(131) "<p>Professor Alexander D. Kulagin, Editor-in-Chief, <i>Cellular Therapy and Transplantation Journal</i></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(107) "Professor Alexander D. Kulagin, Editor-in-Chief, Cellular Therapy and Transplantation Journal
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28498" ["VALUE"]=> array(2) { ["TEXT"]=> string(1331) "<p style="text-align: justify;"> In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125<sup>th</sup> anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with <sup>59</sup>Fe and other radionuclides. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1285) "In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125th anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with 59Fe and other radionuclides.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28499" ["VALUE"]=> string(46) "Pavlov University: 125 years in blood research" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(46) "Pavlov University: 125 years in blood research" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28500" ["VALUE"]=> array(2) { ["TEXT"]=> string(7751) "<p style="text-align: justify;">С 70-х годов кафедру возглавил проф. В. А. Алмазов. С этого времени здесь началось изучение лейкогенеза и регуляции кроветворения новым поколением клинических гематологов во главе с Б. В. Афанасьевым. Культивирование колониеобразующих единиц клеток-предшественников грануло-моноцитопоэза позволили получить первые данные о внутренних факторах регуляции грануломоноцитопоэза при острых лейкозах, хроническом миелолейкозе, особенно при различных типах бластных кризов, миелодиспластическом синдроме у взрослых и, впервые – при апластической анемии у детей. Эти данные были обобщены в первой монографии в этой области «Родоначальные стволовые кроветворные клетки человека» (1985). </p> <p style="text-align: justify;">Трагически известная Чернобыльская ядерная авария (1986 г.) способствовала развитию исследований в области острого цитостатического синдрома в СССР и за рубежом. Борис Владимирович Афанасьев, сотрудник 1-го Ленинградского медицинского института им. И. П. Павлова, был направлен в Сиэттл (США) для стажировки в знаменитую клинику Э. Доннела Томаса, в последующем лауреата Нобелевской премии 1990 г. за успешную трансплантацию гемопоэтических клеток в клинике. Через несколько лет, по инициативе профессора Б. В. Афанасьева, руководство Университета организовало отделение трансплантации костного мозга (1997 г.), где была начата программа по широкому внедрению различных видов трансплантации гемопоэтических стволовых клеток у детей и взрослых.</p> <p style="text-align: justify;">Следует отметить обширную клиническую помощь и консультационные усилия наших зарубежных друзей и коллег в области принципов лечения лейкозов, иммунологического типирования, диагностики лейкозов и схем лечения. Эта поддержка была чрезвычайно важной в 1990-1996 гг., на ранних этапах нашей работы по трансплантации костного мозга. Отделения гематологии, онкологии и ТГСК университета не смогли бы добиться успеха в этой области без устойчивых профессиональных контактов с выдающимися специалистами из Европы и США. Прежде всего, следует отметить тесное сотрудничество с Университетскими клиниками Гамбурга и другими университетами Германии при непосредственном участии проф. Р. Нета, А. Цандера, Т. Бюхнера, других ведущих германских специалистов – Х. И. Кольба, Д. Хёльцера, Б. Фезе. В эту совместную работу были вовлечены и ведущие специалисты из других стран, например, проф. Р. Гэйл, (США), Г. Вагемакер (Нидерланды), А. Бачигалупо (Италия) и многие другие известные клиницисты. Проф. Аксель Цандер, Аксель Фаузер, Герард Вaгемaкер, Дитер Хёльцер были удостоены звания почетных докторов ПСПбГМУ им. И. П. Павлова за заслуги в сотрудничестве с российскими специалистами в этой области. </p> <p style="text-align: justify;">В последние 15 лет развитие гематологии в Университете связано с организованным проф. Б. В. Афанасьевым НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, который входит в число крупнейших центров ТКМ в Европе. За этот период выполнено более 4500 аллогенных и аутологичных трансплантаций детям и взрослым с лейкозами, лимфомами, множественной миеломой, апластическими анемиями, солидными опухолями, иммунодефицитами заболеваниями и нарушениями обмена веществ. В Институте проводятся экспериментальные и клинические исследования в области лейкемий, миелопролиферативных заболеваний, лимфом, миеломы, костномозговой недостаточности и других областях гематологии.</p><p style="text-align: justify;"> Журнал «Клеточная терапия и трансплантация» (СТТ) – совместный проект немецких и российских специалистов в области ТКМ и онкогематологии, издается с 2008 года. Журнал публикует оригинальные данные по трансплантации гемопоэтических стволовых клеток, иммунотерапии, клеточной и генной терапии, а также смежным вопросам медицины и биологии. Мы надеемся, что клиническая, исследовательская и издательская деятельность в этой области будет и дальше развиваться в Первом Санкт-Петербургском государственном медицинском университете им. И. П. Павлова в тесном сотрудничестве с нашими российскими и зарубежными коллегами на благо пациентов с лейкозами и другими тяжелыми заболеваниями, которые сейчас могут быть излечены с помощью современных терапевтических подходов. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(7641) "С 70-х годов кафедру возглавил проф. В. А. Алмазов. С этого времени здесь началось изучение лейкогенеза и регуляции кроветворения новым поколением клинических гематологов во главе с Б. В. Афанасьевым. Культивирование колониеобразующих единиц клеток-предшественников грануло-моноцитопоэза позволили получить первые данные о внутренних факторах регуляции грануломоноцитопоэза при острых лейкозах, хроническом миелолейкозе, особенно при различных типах бластных кризов, миелодиспластическом синдроме у взрослых и, впервые – при апластической анемии у детей. Эти данные были обобщены в первой монографии в этой области «Родоначальные стволовые кроветворные клетки человека» (1985).
Трагически известная Чернобыльская ядерная авария (1986 г.) способствовала развитию исследований в области острого цитостатического синдрома в СССР и за рубежом. Борис Владимирович Афанасьев, сотрудник 1-го Ленинградского медицинского института им. И. П. Павлова, был направлен в Сиэттл (США) для стажировки в знаменитую клинику Э. Доннела Томаса, в последующем лауреата Нобелевской премии 1990 г. за успешную трансплантацию гемопоэтических клеток в клинике. Через несколько лет, по инициативе профессора Б. В. Афанасьева, руководство Университета организовало отделение трансплантации костного мозга (1997 г.), где была начата программа по широкому внедрению различных видов трансплантации гемопоэтических стволовых клеток у детей и взрослых.
Следует отметить обширную клиническую помощь и консультационные усилия наших зарубежных друзей и коллег в области принципов лечения лейкозов, иммунологического типирования, диагностики лейкозов и схем лечения. Эта поддержка была чрезвычайно важной в 1990-1996 гг., на ранних этапах нашей работы по трансплантации костного мозга. Отделения гематологии, онкологии и ТГСК университета не смогли бы добиться успеха в этой области без устойчивых профессиональных контактов с выдающимися специалистами из Европы и США. Прежде всего, следует отметить тесное сотрудничество с Университетскими клиниками Гамбурга и другими университетами Германии при непосредственном участии проф. Р. Нета, А. Цандера, Т. Бюхнера, других ведущих германских специалистов – Х. И. Кольба, Д. Хёльцера, Б. Фезе. В эту совместную работу были вовлечены и ведущие специалисты из других стран, например, проф. Р. Гэйл, (США), Г. Вагемакер (Нидерланды), А. Бачигалупо (Италия) и многие другие известные клиницисты. Проф. Аксель Цандер, Аксель Фаузер, Герард Вaгемaкер, Дитер Хёльцер были удостоены звания почетных докторов ПСПбГМУ им. И. П. Павлова за заслуги в сотрудничестве с российскими специалистами в этой области.
В последние 15 лет развитие гематологии в Университете связано с организованным проф. Б. В. Афанасьевым НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, который входит в число крупнейших центров ТКМ в Европе. За этот период выполнено более 4500 аллогенных и аутологичных трансплантаций детям и взрослым с лейкозами, лимфомами, множественной миеломой, апластическими анемиями, солидными опухолями, иммунодефицитами заболеваниями и нарушениями обмена веществ. В Институте проводятся экспериментальные и клинические исследования в области лейкемий, миелопролиферативных заболеваний, лимфом, миеломы, костномозговой недостаточности и других областях гематологии.
Журнал «Клеточная терапия и трансплантация» (СТТ) – совместный проект немецких и российских специалистов в области ТКМ и онкогематологии, издается с 2008 года. Журнал публикует оригинальные данные по трансплантации гемопоэтических стволовых клеток, иммунотерапии, клеточной и генной терапии, а также смежным вопросам медицины и биологии. Мы надеемся, что клиническая, исследовательская и издательская деятельность в этой области будет и дальше развиваться в Первом Санкт-Петербургском государственном медицинском университете им. И. П. Павлова в тесном сотрудничестве с нашими российскими и зарубежными коллегами на благо пациентов с лейкозами и другими тяжелыми заболеваниями, которые сейчас могут быть излечены с помощью современных терапевтических подходов.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28501" ["VALUE"]=> string(4) "2759" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2759" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28502" ["VALUE"]=> string(4) "2760" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2760" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(6) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28497" ["VALUE"]=> array(2) { ["TEXT"]=> string(131) "<p>Professor Alexander D. Kulagin, Editor-in-Chief, <i>Cellular Therapy and Transplantation Journal</i></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(107) "Professor Alexander D. Kulagin, Editor-in-Chief, Cellular Therapy and Transplantation Journal
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(107) "Professor Alexander D. Kulagin, Editor-in-Chief, Cellular Therapy and Transplantation Journal
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28498" ["VALUE"]=> array(2) { ["TEXT"]=> string(1331) "<p style="text-align: justify;"> In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125<sup>th</sup> anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with <sup>59</sup>Fe and other radionuclides. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1285) "In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125th anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with 59Fe and other radionuclides.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(1285) "In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125th anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with 59Fe and other radionuclides.
" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28499" ["VALUE"]=> string(46) "Pavlov University: 125 years in blood research" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(46) "Pavlov University: 125 years in blood research" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(46) "Pavlov University: 125 years in blood research" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28495" ["VALUE"]=> array(2) { ["TEXT"]=> string(221) "<p>Профессор Александр Д. Кулагин, главный редактор журнала <i>«Клеточная Терапия и Трансплантация» (СТТ)</i></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(197) "Профессор Александр Д. Кулагин, главный редактор журнала «Клеточная Терапия и Трансплантация» (СТТ)
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(197) "Профессор Александр Д. Кулагин, главный редактор журнала «Клеточная Терапия и Трансплантация» (СТТ)
" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28496" ["VALUE"]=> array(2) { ["TEXT"]=> string(2396) "<p style="text-align: justify;">В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением <sup>59</sup>Fe и других радиоактивных изотопов.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2362) "В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением 59Fe и других радиоактивных изотопов.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(2362) "В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением 59Fe и других радиоактивных изотопов.
" } ["FULL_TEXT_RU"]=> array(37) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28500" ["VALUE"]=> array(2) { ["TEXT"]=> string(7751) "<p style="text-align: justify;">С 70-х годов кафедру возглавил проф. В. А. Алмазов. С этого времени здесь началось изучение лейкогенеза и регуляции кроветворения новым поколением клинических гематологов во главе с Б. В. Афанасьевым. Культивирование колониеобразующих единиц клеток-предшественников грануло-моноцитопоэза позволили получить первые данные о внутренних факторах регуляции грануломоноцитопоэза при острых лейкозах, хроническом миелолейкозе, особенно при различных типах бластных кризов, миелодиспластическом синдроме у взрослых и, впервые – при апластической анемии у детей. Эти данные были обобщены в первой монографии в этой области «Родоначальные стволовые кроветворные клетки человека» (1985). </p> <p style="text-align: justify;">Трагически известная Чернобыльская ядерная авария (1986 г.) способствовала развитию исследований в области острого цитостатического синдрома в СССР и за рубежом. Борис Владимирович Афанасьев, сотрудник 1-го Ленинградского медицинского института им. И. П. Павлова, был направлен в Сиэттл (США) для стажировки в знаменитую клинику Э. Доннела Томаса, в последующем лауреата Нобелевской премии 1990 г. за успешную трансплантацию гемопоэтических клеток в клинике. Через несколько лет, по инициативе профессора Б. В. Афанасьева, руководство Университета организовало отделение трансплантации костного мозга (1997 г.), где была начата программа по широкому внедрению различных видов трансплантации гемопоэтических стволовых клеток у детей и взрослых.</p> <p style="text-align: justify;">Следует отметить обширную клиническую помощь и консультационные усилия наших зарубежных друзей и коллег в области принципов лечения лейкозов, иммунологического типирования, диагностики лейкозов и схем лечения. Эта поддержка была чрезвычайно важной в 1990-1996 гг., на ранних этапах нашей работы по трансплантации костного мозга. Отделения гематологии, онкологии и ТГСК университета не смогли бы добиться успеха в этой области без устойчивых профессиональных контактов с выдающимися специалистами из Европы и США. Прежде всего, следует отметить тесное сотрудничество с Университетскими клиниками Гамбурга и другими университетами Германии при непосредственном участии проф. Р. Нета, А. Цандера, Т. Бюхнера, других ведущих германских специалистов – Х. И. Кольба, Д. Хёльцера, Б. Фезе. В эту совместную работу были вовлечены и ведущие специалисты из других стран, например, проф. Р. Гэйл, (США), Г. Вагемакер (Нидерланды), А. Бачигалупо (Италия) и многие другие известные клиницисты. Проф. Аксель Цандер, Аксель Фаузер, Герард Вaгемaкер, Дитер Хёльцер были удостоены звания почетных докторов ПСПбГМУ им. И. П. Павлова за заслуги в сотрудничестве с российскими специалистами в этой области. </p> <p style="text-align: justify;">В последние 15 лет развитие гематологии в Университете связано с организованным проф. Б. В. Афанасьевым НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, который входит в число крупнейших центров ТКМ в Европе. За этот период выполнено более 4500 аллогенных и аутологичных трансплантаций детям и взрослым с лейкозами, лимфомами, множественной миеломой, апластическими анемиями, солидными опухолями, иммунодефицитами заболеваниями и нарушениями обмена веществ. В Институте проводятся экспериментальные и клинические исследования в области лейкемий, миелопролиферативных заболеваний, лимфом, миеломы, костномозговой недостаточности и других областях гематологии.</p><p style="text-align: justify;"> Журнал «Клеточная терапия и трансплантация» (СТТ) – совместный проект немецких и российских специалистов в области ТКМ и онкогематологии, издается с 2008 года. Журнал публикует оригинальные данные по трансплантации гемопоэтических стволовых клеток, иммунотерапии, клеточной и генной терапии, а также смежным вопросам медицины и биологии. Мы надеемся, что клиническая, исследовательская и издательская деятельность в этой области будет и дальше развиваться в Первом Санкт-Петербургском государственном медицинском университете им. И. П. Павлова в тесном сотрудничестве с нашими российскими и зарубежными коллегами на благо пациентов с лейкозами и другими тяжелыми заболеваниями, которые сейчас могут быть излечены с помощью современных терапевтических подходов. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(7641) "С 70-х годов кафедру возглавил проф. В. А. Алмазов. С этого времени здесь началось изучение лейкогенеза и регуляции кроветворения новым поколением клинических гематологов во главе с Б. В. Афанасьевым. Культивирование колониеобразующих единиц клеток-предшественников грануло-моноцитопоэза позволили получить первые данные о внутренних факторах регуляции грануломоноцитопоэза при острых лейкозах, хроническом миелолейкозе, особенно при различных типах бластных кризов, миелодиспластическом синдроме у взрослых и, впервые – при апластической анемии у детей. Эти данные были обобщены в первой монографии в этой области «Родоначальные стволовые кроветворные клетки человека» (1985).
Трагически известная Чернобыльская ядерная авария (1986 г.) способствовала развитию исследований в области острого цитостатического синдрома в СССР и за рубежом. Борис Владимирович Афанасьев, сотрудник 1-го Ленинградского медицинского института им. И. П. Павлова, был направлен в Сиэттл (США) для стажировки в знаменитую клинику Э. Доннела Томаса, в последующем лауреата Нобелевской премии 1990 г. за успешную трансплантацию гемопоэтических клеток в клинике. Через несколько лет, по инициативе профессора Б. В. Афанасьева, руководство Университета организовало отделение трансплантации костного мозга (1997 г.), где была начата программа по широкому внедрению различных видов трансплантации гемопоэтических стволовых клеток у детей и взрослых.
Следует отметить обширную клиническую помощь и консультационные усилия наших зарубежных друзей и коллег в области принципов лечения лейкозов, иммунологического типирования, диагностики лейкозов и схем лечения. Эта поддержка была чрезвычайно важной в 1990-1996 гг., на ранних этапах нашей работы по трансплантации костного мозга. Отделения гематологии, онкологии и ТГСК университета не смогли бы добиться успеха в этой области без устойчивых профессиональных контактов с выдающимися специалистами из Европы и США. Прежде всего, следует отметить тесное сотрудничество с Университетскими клиниками Гамбурга и другими университетами Германии при непосредственном участии проф. Р. Нета, А. Цандера, Т. Бюхнера, других ведущих германских специалистов – Х. И. Кольба, Д. Хёльцера, Б. Фезе. В эту совместную работу были вовлечены и ведущие специалисты из других стран, например, проф. Р. Гэйл, (США), Г. Вагемакер (Нидерланды), А. Бачигалупо (Италия) и многие другие известные клиницисты. Проф. Аксель Цандер, Аксель Фаузер, Герард Вaгемaкер, Дитер Хёльцер были удостоены звания почетных докторов ПСПбГМУ им. И. П. Павлова за заслуги в сотрудничестве с российскими специалистами в этой области.
В последние 15 лет развитие гематологии в Университете связано с организованным проф. Б. В. Афанасьевым НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, который входит в число крупнейших центров ТКМ в Европе. За этот период выполнено более 4500 аллогенных и аутологичных трансплантаций детям и взрослым с лейкозами, лимфомами, множественной миеломой, апластическими анемиями, солидными опухолями, иммунодефицитами заболеваниями и нарушениями обмена веществ. В Институте проводятся экспериментальные и клинические исследования в области лейкемий, миелопролиферативных заболеваний, лимфом, миеломы, костномозговой недостаточности и других областях гематологии.
Журнал «Клеточная терапия и трансплантация» (СТТ) – совместный проект немецких и российских специалистов в области ТКМ и онкогематологии, издается с 2008 года. Журнал публикует оригинальные данные по трансплантации гемопоэтических стволовых клеток, иммунотерапии, клеточной и генной терапии, а также смежным вопросам медицины и биологии. Мы надеемся, что клиническая, исследовательская и издательская деятельность в этой области будет и дальше развиваться в Первом Санкт-Петербургском государственном медицинском университете им. И. П. Павлова в тесном сотрудничестве с нашими российскими и зарубежными коллегами на благо пациентов с лейкозами и другими тяжелыми заболеваниями, которые сейчас могут быть излечены с помощью современных терапевтических подходов.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(7641) "С 70-х годов кафедру возглавил проф. В. А. Алмазов. С этого времени здесь началось изучение лейкогенеза и регуляции кроветворения новым поколением клинических гематологов во главе с Б. В. Афанасьевым. Культивирование колониеобразующих единиц клеток-предшественников грануло-моноцитопоэза позволили получить первые данные о внутренних факторах регуляции грануломоноцитопоэза при острых лейкозах, хроническом миелолейкозе, особенно при различных типах бластных кризов, миелодиспластическом синдроме у взрослых и, впервые – при апластической анемии у детей. Эти данные были обобщены в первой монографии в этой области «Родоначальные стволовые кроветворные клетки человека» (1985).
Трагически известная Чернобыльская ядерная авария (1986 г.) способствовала развитию исследований в области острого цитостатического синдрома в СССР и за рубежом. Борис Владимирович Афанасьев, сотрудник 1-го Ленинградского медицинского института им. И. П. Павлова, был направлен в Сиэттл (США) для стажировки в знаменитую клинику Э. Доннела Томаса, в последующем лауреата Нобелевской премии 1990 г. за успешную трансплантацию гемопоэтических клеток в клинике. Через несколько лет, по инициативе профессора Б. В. Афанасьева, руководство Университета организовало отделение трансплантации костного мозга (1997 г.), где была начата программа по широкому внедрению различных видов трансплантации гемопоэтических стволовых клеток у детей и взрослых.
Следует отметить обширную клиническую помощь и консультационные усилия наших зарубежных друзей и коллег в области принципов лечения лейкозов, иммунологического типирования, диагностики лейкозов и схем лечения. Эта поддержка была чрезвычайно важной в 1990-1996 гг., на ранних этапах нашей работы по трансплантации костного мозга. Отделения гематологии, онкологии и ТГСК университета не смогли бы добиться успеха в этой области без устойчивых профессиональных контактов с выдающимися специалистами из Европы и США. Прежде всего, следует отметить тесное сотрудничество с Университетскими клиниками Гамбурга и другими университетами Германии при непосредственном участии проф. Р. Нета, А. Цандера, Т. Бюхнера, других ведущих германских специалистов – Х. И. Кольба, Д. Хёльцера, Б. Фезе. В эту совместную работу были вовлечены и ведущие специалисты из других стран, например, проф. Р. Гэйл, (США), Г. Вагемакер (Нидерланды), А. Бачигалупо (Италия) и многие другие известные клиницисты. Проф. Аксель Цандер, Аксель Фаузер, Герард Вaгемaкер, Дитер Хёльцер были удостоены звания почетных докторов ПСПбГМУ им. И. П. Павлова за заслуги в сотрудничестве с российскими специалистами в этой области.
В последние 15 лет развитие гематологии в Университете связано с организованным проф. Б. В. Афанасьевым НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, который входит в число крупнейших центров ТКМ в Европе. За этот период выполнено более 4500 аллогенных и аутологичных трансплантаций детям и взрослым с лейкозами, лимфомами, множественной миеломой, апластическими анемиями, солидными опухолями, иммунодефицитами заболеваниями и нарушениями обмена веществ. В Институте проводятся экспериментальные и клинические исследования в области лейкемий, миелопролиферативных заболеваний, лимфом, миеломы, костномозговой недостаточности и других областях гематологии.
Журнал «Клеточная терапия и трансплантация» (СТТ) – совместный проект немецких и российских специалистов в области ТКМ и онкогематологии, издается с 2008 года. Журнал публикует оригинальные данные по трансплантации гемопоэтических стволовых клеток, иммунотерапии, клеточной и генной терапии, а также смежным вопросам медицины и биологии. Мы надеемся, что клиническая, исследовательская и издательская деятельность в этой области будет и дальше развиваться в Первом Санкт-Петербургском государственном медицинском университете им. И. П. Павлова в тесном сотрудничестве с нашими российскими и зарубежными коллегами на благо пациентов с лейкозами и другими тяжелыми заболеваниями, которые сейчас могут быть излечены с помощью современных терапевтических подходов.
" } } } [1]=> array(49) { ["IBLOCK_SECTION_ID"]=> string(3) "206" ["~IBLOCK_SECTION_ID"]=> string(3) "206" ["ID"]=> string(4) "2050" ["~ID"]=> string(4) "2050" ["IBLOCK_ID"]=> string(1) "2" ["~IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["~NAME"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["ACTIVE_FROM"]=> NULL ["~ACTIVE_FROM"]=> NULL ["TIMESTAMP_X"]=> string(22) "04/18/2022 11:59:36 am" ["~TIMESTAMP_X"]=> string(22) "04/18/2022 11:59:36 am" ["DETAIL_PAGE_URL"]=> string(143) "/en/archive/tom-11-nomer-1/obzornye-stati/vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr/" ["~DETAIL_PAGE_URL"]=> string(143) "/en/archive/tom-11-nomer-1/obzornye-stati/vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr/" ["LIST_PAGE_URL"]=> string(12) "/en/archive/" ["~LIST_PAGE_URL"]=> string(12) "/en/archive/" ["DETAIL_TEXT"]=> string(27638) "Introduction
General issues
Retinoblastoma (RB) is the most common pediatric eye cancer developing from immature cells of the retina [1-3]. In infants it is most commonly associated with biallelic mutation of RB1 gene [4]. In these cases the tumor may involve one, as well as both, eyes and also may produce synchronous or metachronous ectopic lesions in the pineal gland (pineoblastoma). Based on extent of involvement these forms are classified as uni- bi- and trilateral [5]. The RB incidence is 1 in 15000-18000 newborn and about 5000 new cases are registered each year [6].
Most treatment programs in patients with RB combine different treatment modalities, which are chosen based in risk group and extent of tumor involvement [7, 8]. In high-risk patients the tumor spreads beyond the eye often developing ectopic metastatic lesions, which may become lethal if no systemic method is applied in addition to local control measures [9]. During the last few decades a number of methods were used to control the disease including systemic polychemotherapy (CT), external beam radiation therapy (EBRT) and other local treatment methods. However, these standard measures may still be ineffective in some cases, so we are ever in need of new global strategies aimed at survival improvement in high-risk RB.
High-dose chemotherapy with autologous hemopoietic stem cell transplantation in patients with RB
In developed countries most children with RB are referred to pediatric oncologist in early stages. Most advanced cases with extraocular and metastatic RB are therefore treated in developing countries. Most deaths in RB patients are due to metastatic disease, pineoblastoma development or secondary cancers, which are most often seen in patients with hereditary forms of disease. The treatment schedule is always personalized in accordance to individual tumor characteristics. Up to this moment the main therapeutic modalities are systemic polychemotherapy (PCT) and local one, which may be delivered as inraarterial chemotherapy (IAC) or intravitreal one (IVitC). There are also additional local control methods such as transpupillary thermotherapy (TTT), cryotherapy, and brachytherapy or enucleation, which may be performed in cases with optical nerve or choroidal invasion [10, 11].
Each of these methods has certain disadvantages and unwanted sequelae. Most clinics limit the use of external beam radiation therapy (EBRT) due to the risk of secondary cancers, facial bones growth disturbance and subsequent deformations. Enucleation is a radical surgical technique based on entire eye removal [12]. While chemoreduction (tumor shrinking in response to systemic chemotherapy) and local control measures are effective in patients with intraocular RB and have fewer adverse effects, they are less effective in patients high-risk disease characterized by initial extraocualr disease, tumor relapse involving extra- or intraocular structures (including distant metastases), tumor invasion of the optic nerve resection line, trilateral RB. As a result, high-risk patients may need more aggressive treatment modalities [10-13]. Therefore, there is still an ongoing search for more effective strategies able to improve long-term survival and quality of life in this cohort.
RB is a highly chemosensitive tumor with exponential log kill curve in tumor cell cultures, so dose-intensive consolidation regimens are expected to increase the overall treatment effectiveness. High-dose chemotherapy (HDCT) is being considered a viable option [14-17]. However, this method is associated with some drawbacks due to its toxic effects, primarily profound myelosuppression, which may lead to serious or even fatal complications if no attempts for bone marrow reconstitution via cryopreserved autologous hemopoietic stem cells (bone marrow or peripheral blood precursors) reinfusion are taken. Autologous hemopoietic stem cells transplantation (auto-HSCT) is the most effective measure to limit secondary myelotoxicity and allows using much higher peak doses of cytostatics potentially increasing RB treatment effectiveness [16].
A number of researchers have demonstrated different high-dose regimens effectiveness in auto-HSCT settings. These regimens are used as consolidation in patients with high-risk pediatric solid tumors as part of a multidisciplinary approach incorporating also surgical treatment and standard dose chemotherapy [12], in some cases they may also help to avoid bilateral enucleation preserving the vision in RB patients.
There is currently no consensus on optimal treatment regimen in late stage RB, although most experts agree on the use of several drugs in combination. These drugs, which may be potentially effective in RB patients, include platinum agents (carboplatin and cisplatin), etoposide, vincristine, cyclophosphamide and anthracyclines [18, 19]. Vincristine, etoposide and carboplatin are characterized by better eye penetration and are therefore most often used in conditioning regimens prior to auto-HSCT.
World experience with auto-HSCT in the RB patients
The HDCT with auto-HSCT is now being used in patients with high-risk RB for more than 20 years. The first patient cohort was described in 1997 by French researchers from Institut Curie (Paris). The HDCT was performed as consolidation for high-risk patients (initially extraocular disease, relapse or tumor invasion of optical nerve resection line). A total of 25 patents received a regimen consisting of carboplatin (250 mg/m2/day from day 1 day 5 in 6 initially high-risk patients after enucleation and standard-dose CT and 250 mg/m2/day in 19 patients with chemosensitive relapse), etoposide (350 mg/m2/day from day 1 to day 5), and cyclophosphamide (1.6 g/m2/day from day 2 to day 5) with subsequent autologous stem cells reinfusion. The 3-year disease-free survival was 67.1%. In 7 of 19 patients with relapse it developed in central nervous system. All patients with CNS relapse except one died of disease progression. The main toxic complications were hematological toxicity and gastrointestinal mucositis (oral mucositis, enterocolitis). Also, 2 of 13 patients developed grade III-IV ototoxicity. In one case a grade I acute re-versible cardiotoxicity was registered. Therefore, while high-dose regimen consisting of carboplatin, etoposide and cyclophosphamide seemed a feasible strategy in high-risk RB patients, especially those with bones and bone marrow involvement, it did not improve the results in cases with CNS involvement [20].
In 2003, a group of German researchers published their data on auto-HSCT outcome in 5 RB patients, 4 of them with bone marrow metastases and one with extraorbital involvement. All patients have achieved response after previous enucleation and standard-dose chemotherapy, a child with extraorbital tumor also received EBRT. In 4 cases the conditioning regimen consisted of thiotepa (900 mg/m2), etoposide (40 mg/kg), and carboplatin (1.5 g/m2), and in 1 case it included carmustine (300 mg/m2), cyclophosphamide (6.8 g/m2), and etoposide (1.6 g/m2). A rapid hemopoiesis reconstitution was observed in all 5 cases. Main toxic complications were mucositis and cytopenia with consequent infections. None of the patients died due to regimen toxicity or experienced any long-term sequelae. A patient with initial extrorbital disease developed a relapse with meningheal involvement 10 months after auto-HSCT, but was salvaged by surgery and standard-dose chemotherapy and remained in remission after 105 months follow-up. Four other patients were still in remission 107, 57, 9, and 8 months after auto-HSCT. The conditioning regimen with thiotepa, etoposide and carboplatin may be a good option for children with extrabulbar or disseminated chemosensitive RB [21].
In 2021, a group of authors from the Faculty of Medicine, University of Indonesia published a review on available data in auto-HSCT for high-risk RB patients [22]. A total of 35 publications describing 160 patients were included. After auto-HSCT 108 of 160 (67.5%) patients are alive and disease free at the last follow-up. The secondary cancer developed in 16 of 160 (10%) patients, which is a comparably low rate. The most common side effects were hematological and gastrointestinal toxicity. As a whole, 41 of 160 (25.6%) died with signs of active disease due to primary CNS involvement (in 25 of 41; 60.9%), disease relapse (12 of 41; 29.3%), or secondary cancer (3 of 41; 7.3%). Only in 1 of 41 (2.4%) cases there was evident metastatic involvement outside CNS. Only 11 of 160 (6.7%) were alive, but not disease-free, at the last fol-low-up. According to this review, the use of HDCT with subsequent auto-HSCT is effective in patients with disseminated RB as 108 of 160 (67.5%) of auto-HSCT recipients stayed alive and disease-free. It corresponds to the data published in previous review by Jaradat I. et al. (2012) [23].
Russian experience with auto-HSCT in children with retinoblastoma
There are several large Russian centers treating most children with RB, i.e., the Helmholtz National Medical Ophthalmology Research Center, S. N. Fedorov National Medical Research Center for Eye Microsurgery, and Research Institute of Pediatric Oncology and Hematology at the N. N. Blokhin National Medical Research Center of Oncology. However, only the latter institution performed HDCT with auto-HSCT in these patients.
There is a description of earlier (2001-2008) experience of auto-HSCT performed in a cohort of 15 RB patients in the Institute of Pediatric Oncology and Hematology at the N. N.Blokhin National Medical Research Center of Oncology. The treatment program included IVitC, EBRT, and high-dose consolidation with busulfan and melphalan followed by auto-HSCT. During the follow-up 1 of 15 patients died of sepsis and 7 of disease progression with CNS involvement. Seven patients are currently alive (5 children with stage II, one with stage IIIа, one with stage IIIb). The new strategy allowed to double the disease- and event-free survival rate of RB patients. The overall survival in high-risk group (optical nerve resection line invasion, extrascleral spread of the tumor) reached 71.4%. The researchers concluded that HDCT with auto-HSCT is an effective method in patients with stage II and III, although more effective options are still warranted for children with disseminated RB [24].
Clinical cases
We present a series of 3 clinical cases of children (aged 3-6 years) with high-risk RB receiving HDCT with auto-HSCT treated at the Pediatric Hematology and Oncology Department (BMT unit) at N. N. Blokhin National Medical Research Center of Oncology (February to October 2021). All the patients achieved remission prior to HSCT after surgery and standard-dose systemic polychemotherapy. The patients’ characteristics are listed in Table 1. Patient 1 had initially demonstrated extraocular tumor growth by the optical nerve, there were also tumor cells in resected margin; patient 2 had initially disseminated disease with cervical lymph nodes involvement, and patient 3 had bilateral disease with extrabulbar and intracranial penetration of the right eye tumor via optical nerve with involvement of ipsilateral chiasma and optical tract.
Table 1. Initial characteristics of our retinoblastoma patients and autologous HSCT details

In order to successfully collect autologous peripheral stem cells according to local standards, all the patients received granulocyte colony-stimulating factor (G-CSF). Stem cell mobilization started 14 days prior to the next chemotherapy course upon recovery of the blood counts. G-CSF was injected subcutaneously for 4-7 days at 5-10 mcg/kg/day, the last dose applied 2-4 hours prior to apheresis procedure. The median yield of СD34+ cells was 2×106/kg body mass.
Patient 1 is a six-year-old child with left-sided retinoblastoma. In October 2020, eye enucleation was performed, followed by microsurgical removal of the left optical nerve by orbitozygomatic approach (pathological study showed tumor cells at the resection line of optical nerve, thus corresponding to high-risk case), with 6 subsequent chemotherapy courses. No staging was performed at the clinic, where the patient was initially treated.
Patient 2, three-year-old, was diagnosed with left-sided retinoblastoma TхNxMх. In October 2020, left eye enucleation was performed. Subsequent staging showed disease progression with metastatic involvement of cervical lymph nodes. Therefore, 4 chemotherapy courses according to NB 2004 protocol and 2 СVC courses were performed. The patient was re-staged as TxN1.
Patient 3, three-year-old, manifested with bilateral RB: OD – group Е, stage T4N0M1; OS – Group B, stage T1N0M1. He received a complex treatment program consisting of 5 systemic chemotherapy courses and 5 courses of intrathecal chemotherapy (methotrexate + prednisolone/thiotepa), surgical treatment (right-sided bone plastic pterional craniotomy with prechiasmal optical nerve resection and eye enucleation) performed in December 2020.
Pre-transplant consolidation regimen consisted of carboplatin 1250 mg/m2, etoposide 1750 mg/m2, and cyclophosphamide 6000 mg/m2. Patients 1 and 2 have tolerated the high-dose regimen well. In patient 3, some complications were registered, i.e., anorexia, nausea, vomiting, and an episode of seizures in presence of arterial hypertension and hyponatremia, the most likely causes of this neurological disorder. The seizures were canceled by anticonvulsants, antihypertensive therapy and infusion of electrolytes. No signs of hemorrhage or ischemia were seen on the brain CT scan.
The HSCT procedure was well tolerated in all cases. During early post-transplant period, all patients received standard supportive therapy (decontamination, prophylaxis of herpesvirus infection, pneumocistic and fungal infections). The leukocyte engraftment was registered on day 11, 14, and 17; in all the cases, G-CSF was injected subcutaneously (5 µg/kg/day). All the patients became transfusion-independent since 14 days post-transplant. There were complaints for nausea and vomiting over the early post-transplant period. In all the cases, distinct infectious and toxic complications were developed, i.e., grade 1-3 oral mucositis, grade 2 neutropenic enterocolitis, and febrile neutropenias. Central line-associated bloodstream infection (CLABSI) was registered in one case. All these complications were controlled by standard therapies. All the patients were subsequently discharged in good clinical condition. The median follow-up is currently 6 (4-10) months. The clinical outcomes of the transplants are shown in Table 2.
Table 2. Results of autologous HSCT in the patients included in the study

Discussion
High-dose consolidation chemotherapy was performed in 3 children with high-risk RB admitted to N. N. Blokhin National Medical Research Center of Oncology. All the patients have well tolerated the treatment. The blood counts recovered relatively early. All complications were successfully treated with standard antibacterial therapy within 14 days post-transplant. Then the patients were discharged from the BMT unit to the Somatic Department for further follow-up. The third patient developed a progressive CNS disease 6 months after auto-HSCT and subsequently died. Patients 1 and 2 have currently no signs of disease progression at the median follow-up of 6 (4-10) months.
Since the dose-intensive therapy is recommended in disseminated RB [9], we used a conditioning regimen including carboplatin, etoposide and cyclophosphamide. This schedule has already been successfully used in international cohorts and proved to be effective in cases of disseminated disease [14, 16-19]. The patients included in our series have also well tolerated the high-dose regimen which corresponds to the published data [20, 23, 26] and may confirm safety of HDCT procedure, even in heavily pretreated children with lower performance score.
Unfortunately, there is lack of effective and curative treatment methods for the patients with CNS involvement despite multiple options used by different centers, with HDCST with auto-HSCT included [9, 20]. We must search for new approaches, or modify the existing methods in order to improve our results in high-risk RB. Our experience shows that concentration of several RB patients with high-risk disease at a single center provides the necessary experience allowing most effective treatment [12, 20-23, 25].
During the last decade, some major shifts occur in the complex treatment of children with RB. Auto-HSCT became an integral part of the overall treatment strategy. Our case series demonstrate acceptable toxicity of this treatment mode, with side effects observed, mostly, in the form of gastrointestinal toxicity. No transplant-related mortality was registered. Therefore, this approach may be considered relatively safe. We should, however, keep in mind that clinical results in patients with CNS metastases are still unsatisfactory. Hence, we should perform more strict selection of the candidates for auto-HSCT. Of course, in order to obtain more reliable results, much larger groups should be studied, which is more likely in context of multicenter studies coordinated on national level.
Conclusion
Auto-HSCT may be considered a feasible, effective and well-tolerated consolidation option for patients with high-risk RB. A larger cohort study with longer follow-up is required to accurately evaluate its effectiveness. This may be achieved in multicenter cooperation.
Conflicts of interest
None reported.
References
- Sun J, Xi H, Shao Q, Liu Q. Biomarkers in retinoblastoma. Int J Ophthalmol. 2019; 13(2): 325-341. doi: 10.18240/ijo.2020.02.18
- Saakyan SV. Retinoblastoma (clinics, diagnostics, treatment). Moscow, Meditsina Publishers. 2005; 200 p. (In Russian).
- Gurney JG, Severson RK, Davis S, Robison LL. Incidence of cancer in children in the United States. Sex-, race-, and 1-year age-specific rates by histologic type. Cancer. 1995; 75(8): 2186-2195. doi: 10.1002/1097-0142(19950415)75:8<2186::AID-CNCR2820750825>3.0.CO;2-F
- Kaewkhaw R, Rojanaporn D. Retinoblastoma: Etiology, modeling, and treatment. Cancers. 2020; 12(8)8. doi: 10.3390/cancers12082304
- Berry JL, Biegel JA, Slavotinek A, Tirnauer JS, Armsby C, Shah S. Gene test interpretation: RB1. Up to date. Oct 2021. https://www.wolterskluwer.com/en/solutions/uptodate/
- Shields J, Shields C. Retinoblastoma: introduction, genetics, clinical features, classification. In: Shields J, Shields C, Eds. Atlas of Intraocular Tumors, 3rd ed., Philadelphia: Lippinocott, Wolters Kluwer; 2016. p. 311-314.
- Ushakova TL, Тrofimov IA, Gorovtsova OV, Yarovoy AA, Saakyan SV, Letyagin IA, et al. A new era of organ-preserving treatment in pediatric intraocular retinoblastoma in Russia: a multicenter cohort study. Oncopediatrics 2018;5(1):51-69. (In Russian).
doi: 10.15690/onco.v5i1.1866 - Dimaras H, Corson TW, Cobrinik D, White A, Zhao J, Munier FL, Abramson DH, Shields CL, Chantada GL, Njuguna F, Gallie BL. Retinoblastoma. Nat Rev Dis Primers. 2015 Aug 27;1:15021. doi: 10.1038/nrdp.2015.21
- Retinoblastoma: Clinical Guidelines (Russian Society of Pediatric Oncologists, Assocoation of Ophtalmologists). 2017; ID: КР71 (In Russian).
- Shields CL, Shields JA. Recent developments in the management of retinoblastoma. J Pediat Ophthalmol Strabismus. 1999; 36(1): 8-18. PMID: 9972509X
- Lee S, Yoo K, Sung K Kim J, Cho E, Koo H, Chung S, Kang S, Oh S, Ham D, Kim Y. Tandem high-dose chemotherapy and autologous stem cell rescue in children with bilateral advanced retinoblastoma. Bone Marrow Transplant. 2008; 42(6): 385-391.
doi: 10.1038/bmt.2008.181 - Matsubara H, Makimoto A, Higa T, Kawamoto H, Sakiyama S, Hosono A, Takayama J, Takaue Y, Murayama S, Sumi M, Kaneko A, Ohira M. A multidisciplinary treatment strategy that includes high-dose chemotherapy for metastatic retinoblastoma without CNS involvement. Bone Marrow Transplant. 2005; 35 (8): 763-766. doi: 10.1038/sj.bmt.1704882
- Ancona-Lezama D, Dalvin L, Shields C. Modern treatment of retinoblastoma: A 2020 review. Ind J Ophthalmol. 2020; 68(11):2356-2365. doi: 10.4103/ijo.IJO_721_20
- White L. Chemotherapy for retinoblastoma: where do we go from here?: a review of published literature and meeting abstracts, including discussions during the Vth International Symposium on Retinoblastoma, Oct 1991. Ophthalmic Paediatr Genet. 1991; 12(3): 115-130. doi: 10.3109/13816819109029393
- Seeger RC, Reynolds CP. Treatment of high-risk solid tumors of childhood with intensive therapy and autologous bone marrow transplantation. Pediat Clin North Amer. 1991; 38: 393-424. doi: 10.1016/S0031-3955(16)38084-1
- Palma J, Sasso D, Dufort G, Koop K, Sampor C, Diez B, Richard L, Castillo L, Chantada G. Successful treatment of metastatic retinoblastoma with high-dose chemotherapy and autologous stem cell rescue in South America. Bone Marrow Transplant. 2012; 47(4): 522-527. doi: 10.1038/bmt.2011.108
- Stepanyan NG, Sidorova NV, Rubanskaya MV, Tupitsyn NN, Matinyan NV, Kirgizov KI, Varfolomeeva SR. Optimization of methods for collecting peripheral hematopoietic stem cells in children with cancer: literature review. Russian Journal of Pediatric Hematology аnd Oncology 2020;7(2):78-85. (In Russian.). doi: 10.21682/2311-1267-2020-7-2-78-85
- Mohty M, Hübel K, Kröger N, Aljurf M, Apperley J, Basak GW, Bazarbachi A, Douglas K, Gabriel I, Garderet L, et al. Autologous haematopoietic stem cell mobilisation in multiple myeloma and lymphoma patients: a position statement from the European Group for Blood and Marrow Transplantation. Вone Marrow Transplant. 2014; 49(7): 865-872. doi: 10.1038/bmt.2014.39
- Zhernyakova AA, Chubukina ZhV, Zapreeva IM, Tiranova SA, Sel’tser AV, Semenova NYu, Bessmel’tsev SS, Chechetkin AV, Gritsaev SV, Kostroma II. Hematopoietic stem cell collection in multiple myeloma patients: influence of the lenalidomide-based therapy and mobilization regimen prior to auto-HSCT II, Klinicheskaya Onkogematologiya/Clinical Oncohematology. 2018; 11(2): 192-197 (In Russian.). doi: 10.21320/2500-2139-2018-11-2-192-197
- Namouni F, Doz F, Tanguy ML, Quintana E, J Michon, Pacquement H, Bouffet E, Gentet JC, Plantaz D, Lutz P, Vannier JP, Validire P, Neuenschwander S, Desjardins L, Zucker JM. High-dose chemotherapy with carboplatin, etoposide and cyclophosphamide followed by a haematopoietic stem cell rescue in patients with high-risk retinoblastoma: a SFOP and SFGM study. Eur J Cancer. 1997; 33(14): 2368-2375. doi: 10.1016/s0959-8049(97)10019-3
- Kremens B, Wieland R, Reinhard H, Neubert D, Beck JD, Klingebiel T, Bornfeld N, Havers W. Retinoblastoma: High-dose chemotherapy with autologous stem cell rescue in children with retinoblastoma; Bone Marrow Transplant. 2003; 31, 281-284.
doi: 10.1038/sj.bmt.1703832 - Clarissa A, Sutandi N, Abdul Fath A. Stem-cell therapy following high-dose chemotherapy in advanced retinoblastoma: A systematic review. Asia-Pacific J Ophthalmol. 2021; 10(4): 397-407. doi: 10.1097/APO.0000000000000372
- Jaradat I, Mubiden R, Salem A, Abdel-Rahman F, Al-Ahmad I, Almousa A. High-dose chemotherapy followed by stem cell transplantation in the management of retinoblastoma: a systematic review. Hematol Oncol Stem Cell Ther. 2012; 5:107-117.
doi: 10.5144/1658-3876.2012.107 - Ushakova TL, Dolgopolov IS, Gorovtsova OV, Matveeva II, Pavlovskaya AI, Glekov IV, Pimenov RI, Boyarshinov VK, Mentkevich GL, Polyakov VG. Analysis of treatment outcomes for high-risk retinoblastoma. Pediatric Oncology. 2009; 3-4: 61-67. (In Russian).
- Yamanaka R, Hayano A, Takashima Y. Trilateral retinoblastoma: A systematic review of 211 cases. Neurosurg Rev. 2019; 42(1):39-48. doi: 10.1007/s10143-017-0890-4
- Carreras E, Dufour C, Mohty M, Kroger N. Hematopoietic stem cell transplantation and cellular therapies. EBMT Handbook, 2019:117-130.
" ["~DETAIL_TEXT"]=> string(27638) "
Introduction
General issues
Retinoblastoma (RB) is the most common pediatric eye cancer developing from immature cells of the retina [1-3]. In infants it is most commonly associated with biallelic mutation of RB1 gene [4]. In these cases the tumor may involve one, as well as both, eyes and also may produce synchronous or metachronous ectopic lesions in the pineal gland (pineoblastoma). Based on extent of involvement these forms are classified as uni- bi- and trilateral [5]. The RB incidence is 1 in 15000-18000 newborn and about 5000 new cases are registered each year [6].
Most treatment programs in patients with RB combine different treatment modalities, which are chosen based in risk group and extent of tumor involvement [7, 8]. In high-risk patients the tumor spreads beyond the eye often developing ectopic metastatic lesions, which may become lethal if no systemic method is applied in addition to local control measures [9]. During the last few decades a number of methods were used to control the disease including systemic polychemotherapy (CT), external beam radiation therapy (EBRT) and other local treatment methods. However, these standard measures may still be ineffective in some cases, so we are ever in need of new global strategies aimed at survival improvement in high-risk RB.
High-dose chemotherapy with autologous hemopoietic stem cell transplantation in patients with RB
In developed countries most children with RB are referred to pediatric oncologist in early stages. Most advanced cases with extraocular and metastatic RB are therefore treated in developing countries. Most deaths in RB patients are due to metastatic disease, pineoblastoma development or secondary cancers, which are most often seen in patients with hereditary forms of disease. The treatment schedule is always personalized in accordance to individual tumor characteristics. Up to this moment the main therapeutic modalities are systemic polychemotherapy (PCT) and local one, which may be delivered as inraarterial chemotherapy (IAC) or intravitreal one (IVitC). There are also additional local control methods such as transpupillary thermotherapy (TTT), cryotherapy, and brachytherapy or enucleation, which may be performed in cases with optical nerve or choroidal invasion [10, 11].
Each of these methods has certain disadvantages and unwanted sequelae. Most clinics limit the use of external beam radiation therapy (EBRT) due to the risk of secondary cancers, facial bones growth disturbance and subsequent deformations. Enucleation is a radical surgical technique based on entire eye removal [12]. While chemoreduction (tumor shrinking in response to systemic chemotherapy) and local control measures are effective in patients with intraocular RB and have fewer adverse effects, they are less effective in patients high-risk disease characterized by initial extraocualr disease, tumor relapse involving extra- or intraocular structures (including distant metastases), tumor invasion of the optic nerve resection line, trilateral RB. As a result, high-risk patients may need more aggressive treatment modalities [10-13]. Therefore, there is still an ongoing search for more effective strategies able to improve long-term survival and quality of life in this cohort.
RB is a highly chemosensitive tumor with exponential log kill curve in tumor cell cultures, so dose-intensive consolidation regimens are expected to increase the overall treatment effectiveness. High-dose chemotherapy (HDCT) is being considered a viable option [14-17]. However, this method is associated with some drawbacks due to its toxic effects, primarily profound myelosuppression, which may lead to serious or even fatal complications if no attempts for bone marrow reconstitution via cryopreserved autologous hemopoietic stem cells (bone marrow or peripheral blood precursors) reinfusion are taken. Autologous hemopoietic stem cells transplantation (auto-HSCT) is the most effective measure to limit secondary myelotoxicity and allows using much higher peak doses of cytostatics potentially increasing RB treatment effectiveness [16].
A number of researchers have demonstrated different high-dose regimens effectiveness in auto-HSCT settings. These regimens are used as consolidation in patients with high-risk pediatric solid tumors as part of a multidisciplinary approach incorporating also surgical treatment and standard dose chemotherapy [12], in some cases they may also help to avoid bilateral enucleation preserving the vision in RB patients.
There is currently no consensus on optimal treatment regimen in late stage RB, although most experts agree on the use of several drugs in combination. These drugs, which may be potentially effective in RB patients, include platinum agents (carboplatin and cisplatin), etoposide, vincristine, cyclophosphamide and anthracyclines [18, 19]. Vincristine, etoposide and carboplatin are characterized by better eye penetration and are therefore most often used in conditioning regimens prior to auto-HSCT.
World experience with auto-HSCT in the RB patients
The HDCT with auto-HSCT is now being used in patients with high-risk RB for more than 20 years. The first patient cohort was described in 1997 by French researchers from Institut Curie (Paris). The HDCT was performed as consolidation for high-risk patients (initially extraocular disease, relapse or tumor invasion of optical nerve resection line). A total of 25 patents received a regimen consisting of carboplatin (250 mg/m2/day from day 1 day 5 in 6 initially high-risk patients after enucleation and standard-dose CT and 250 mg/m2/day in 19 patients with chemosensitive relapse), etoposide (350 mg/m2/day from day 1 to day 5), and cyclophosphamide (1.6 g/m2/day from day 2 to day 5) with subsequent autologous stem cells reinfusion. The 3-year disease-free survival was 67.1%. In 7 of 19 patients with relapse it developed in central nervous system. All patients with CNS relapse except one died of disease progression. The main toxic complications were hematological toxicity and gastrointestinal mucositis (oral mucositis, enterocolitis). Also, 2 of 13 patients developed grade III-IV ototoxicity. In one case a grade I acute re-versible cardiotoxicity was registered. Therefore, while high-dose regimen consisting of carboplatin, etoposide and cyclophosphamide seemed a feasible strategy in high-risk RB patients, especially those with bones and bone marrow involvement, it did not improve the results in cases with CNS involvement [20].
In 2003, a group of German researchers published their data on auto-HSCT outcome in 5 RB patients, 4 of them with bone marrow metastases and one with extraorbital involvement. All patients have achieved response after previous enucleation and standard-dose chemotherapy, a child with extraorbital tumor also received EBRT. In 4 cases the conditioning regimen consisted of thiotepa (900 mg/m2), etoposide (40 mg/kg), and carboplatin (1.5 g/m2), and in 1 case it included carmustine (300 mg/m2), cyclophosphamide (6.8 g/m2), and etoposide (1.6 g/m2). A rapid hemopoiesis reconstitution was observed in all 5 cases. Main toxic complications were mucositis and cytopenia with consequent infections. None of the patients died due to regimen toxicity or experienced any long-term sequelae. A patient with initial extrorbital disease developed a relapse with meningheal involvement 10 months after auto-HSCT, but was salvaged by surgery and standard-dose chemotherapy and remained in remission after 105 months follow-up. Four other patients were still in remission 107, 57, 9, and 8 months after auto-HSCT. The conditioning regimen with thiotepa, etoposide and carboplatin may be a good option for children with extrabulbar or disseminated chemosensitive RB [21].
In 2021, a group of authors from the Faculty of Medicine, University of Indonesia published a review on available data in auto-HSCT for high-risk RB patients [22]. A total of 35 publications describing 160 patients were included. After auto-HSCT 108 of 160 (67.5%) patients are alive and disease free at the last follow-up. The secondary cancer developed in 16 of 160 (10%) patients, which is a comparably low rate. The most common side effects were hematological and gastrointestinal toxicity. As a whole, 41 of 160 (25.6%) died with signs of active disease due to primary CNS involvement (in 25 of 41; 60.9%), disease relapse (12 of 41; 29.3%), or secondary cancer (3 of 41; 7.3%). Only in 1 of 41 (2.4%) cases there was evident metastatic involvement outside CNS. Only 11 of 160 (6.7%) were alive, but not disease-free, at the last fol-low-up. According to this review, the use of HDCT with subsequent auto-HSCT is effective in patients with disseminated RB as 108 of 160 (67.5%) of auto-HSCT recipients stayed alive and disease-free. It corresponds to the data published in previous review by Jaradat I. et al. (2012) [23].
Russian experience with auto-HSCT in children with retinoblastoma
There are several large Russian centers treating most children with RB, i.e., the Helmholtz National Medical Ophthalmology Research Center, S. N. Fedorov National Medical Research Center for Eye Microsurgery, and Research Institute of Pediatric Oncology and Hematology at the N. N. Blokhin National Medical Research Center of Oncology. However, only the latter institution performed HDCT with auto-HSCT in these patients.
There is a description of earlier (2001-2008) experience of auto-HSCT performed in a cohort of 15 RB patients in the Institute of Pediatric Oncology and Hematology at the N. N.Blokhin National Medical Research Center of Oncology. The treatment program included IVitC, EBRT, and high-dose consolidation with busulfan and melphalan followed by auto-HSCT. During the follow-up 1 of 15 patients died of sepsis and 7 of disease progression with CNS involvement. Seven patients are currently alive (5 children with stage II, one with stage IIIа, one with stage IIIb). The new strategy allowed to double the disease- and event-free survival rate of RB patients. The overall survival in high-risk group (optical nerve resection line invasion, extrascleral spread of the tumor) reached 71.4%. The researchers concluded that HDCT with auto-HSCT is an effective method in patients with stage II and III, although more effective options are still warranted for children with disseminated RB [24].
Clinical cases
We present a series of 3 clinical cases of children (aged 3-6 years) with high-risk RB receiving HDCT with auto-HSCT treated at the Pediatric Hematology and Oncology Department (BMT unit) at N. N. Blokhin National Medical Research Center of Oncology (February to October 2021). All the patients achieved remission prior to HSCT after surgery and standard-dose systemic polychemotherapy. The patients’ characteristics are listed in Table 1. Patient 1 had initially demonstrated extraocular tumor growth by the optical nerve, there were also tumor cells in resected margin; patient 2 had initially disseminated disease with cervical lymph nodes involvement, and patient 3 had bilateral disease with extrabulbar and intracranial penetration of the right eye tumor via optical nerve with involvement of ipsilateral chiasma and optical tract.
Table 1. Initial characteristics of our retinoblastoma patients and autologous HSCT details

In order to successfully collect autologous peripheral stem cells according to local standards, all the patients received granulocyte colony-stimulating factor (G-CSF). Stem cell mobilization started 14 days prior to the next chemotherapy course upon recovery of the blood counts. G-CSF was injected subcutaneously for 4-7 days at 5-10 mcg/kg/day, the last dose applied 2-4 hours prior to apheresis procedure. The median yield of СD34+ cells was 2×106/kg body mass.
Patient 1 is a six-year-old child with left-sided retinoblastoma. In October 2020, eye enucleation was performed, followed by microsurgical removal of the left optical nerve by orbitozygomatic approach (pathological study showed tumor cells at the resection line of optical nerve, thus corresponding to high-risk case), with 6 subsequent chemotherapy courses. No staging was performed at the clinic, where the patient was initially treated.
Patient 2, three-year-old, was diagnosed with left-sided retinoblastoma TхNxMх. In October 2020, left eye enucleation was performed. Subsequent staging showed disease progression with metastatic involvement of cervical lymph nodes. Therefore, 4 chemotherapy courses according to NB 2004 protocol and 2 СVC courses were performed. The patient was re-staged as TxN1.
Patient 3, three-year-old, manifested with bilateral RB: OD – group Е, stage T4N0M1; OS – Group B, stage T1N0M1. He received a complex treatment program consisting of 5 systemic chemotherapy courses and 5 courses of intrathecal chemotherapy (methotrexate + prednisolone/thiotepa), surgical treatment (right-sided bone plastic pterional craniotomy with prechiasmal optical nerve resection and eye enucleation) performed in December 2020.
Pre-transplant consolidation regimen consisted of carboplatin 1250 mg/m2, etoposide 1750 mg/m2, and cyclophosphamide 6000 mg/m2. Patients 1 and 2 have tolerated the high-dose regimen well. In patient 3, some complications were registered, i.e., anorexia, nausea, vomiting, and an episode of seizures in presence of arterial hypertension and hyponatremia, the most likely causes of this neurological disorder. The seizures were canceled by anticonvulsants, antihypertensive therapy and infusion of electrolytes. No signs of hemorrhage or ischemia were seen on the brain CT scan.
The HSCT procedure was well tolerated in all cases. During early post-transplant period, all patients received standard supportive therapy (decontamination, prophylaxis of herpesvirus infection, pneumocistic and fungal infections). The leukocyte engraftment was registered on day 11, 14, and 17; in all the cases, G-CSF was injected subcutaneously (5 µg/kg/day). All the patients became transfusion-independent since 14 days post-transplant. There were complaints for nausea and vomiting over the early post-transplant period. In all the cases, distinct infectious and toxic complications were developed, i.e., grade 1-3 oral mucositis, grade 2 neutropenic enterocolitis, and febrile neutropenias. Central line-associated bloodstream infection (CLABSI) was registered in one case. All these complications were controlled by standard therapies. All the patients were subsequently discharged in good clinical condition. The median follow-up is currently 6 (4-10) months. The clinical outcomes of the transplants are shown in Table 2.
Table 2. Results of autologous HSCT in the patients included in the study

Discussion
High-dose consolidation chemotherapy was performed in 3 children with high-risk RB admitted to N. N. Blokhin National Medical Research Center of Oncology. All the patients have well tolerated the treatment. The blood counts recovered relatively early. All complications were successfully treated with standard antibacterial therapy within 14 days post-transplant. Then the patients were discharged from the BMT unit to the Somatic Department for further follow-up. The third patient developed a progressive CNS disease 6 months after auto-HSCT and subsequently died. Patients 1 and 2 have currently no signs of disease progression at the median follow-up of 6 (4-10) months.
Since the dose-intensive therapy is recommended in disseminated RB [9], we used a conditioning regimen including carboplatin, etoposide and cyclophosphamide. This schedule has already been successfully used in international cohorts and proved to be effective in cases of disseminated disease [14, 16-19]. The patients included in our series have also well tolerated the high-dose regimen which corresponds to the published data [20, 23, 26] and may confirm safety of HDCT procedure, even in heavily pretreated children with lower performance score.
Unfortunately, there is lack of effective and curative treatment methods for the patients with CNS involvement despite multiple options used by different centers, with HDCST with auto-HSCT included [9, 20]. We must search for new approaches, or modify the existing methods in order to improve our results in high-risk RB. Our experience shows that concentration of several RB patients with high-risk disease at a single center provides the necessary experience allowing most effective treatment [12, 20-23, 25].
During the last decade, some major shifts occur in the complex treatment of children with RB. Auto-HSCT became an integral part of the overall treatment strategy. Our case series demonstrate acceptable toxicity of this treatment mode, with side effects observed, mostly, in the form of gastrointestinal toxicity. No transplant-related mortality was registered. Therefore, this approach may be considered relatively safe. We should, however, keep in mind that clinical results in patients with CNS metastases are still unsatisfactory. Hence, we should perform more strict selection of the candidates for auto-HSCT. Of course, in order to obtain more reliable results, much larger groups should be studied, which is more likely in context of multicenter studies coordinated on national level.
Conclusion
Auto-HSCT may be considered a feasible, effective and well-tolerated consolidation option for patients with high-risk RB. A larger cohort study with longer follow-up is required to accurately evaluate its effectiveness. This may be achieved in multicenter cooperation.
Conflicts of interest
None reported.
References
- Sun J, Xi H, Shao Q, Liu Q. Biomarkers in retinoblastoma. Int J Ophthalmol. 2019; 13(2): 325-341. doi: 10.18240/ijo.2020.02.18
- Saakyan SV. Retinoblastoma (clinics, diagnostics, treatment). Moscow, Meditsina Publishers. 2005; 200 p. (In Russian).
- Gurney JG, Severson RK, Davis S, Robison LL. Incidence of cancer in children in the United States. Sex-, race-, and 1-year age-specific rates by histologic type. Cancer. 1995; 75(8): 2186-2195. doi: 10.1002/1097-0142(19950415)75:8<2186::AID-CNCR2820750825>3.0.CO;2-F
- Kaewkhaw R, Rojanaporn D. Retinoblastoma: Etiology, modeling, and treatment. Cancers. 2020; 12(8)8. doi: 10.3390/cancers12082304
- Berry JL, Biegel JA, Slavotinek A, Tirnauer JS, Armsby C, Shah S. Gene test interpretation: RB1. Up to date. Oct 2021. https://www.wolterskluwer.com/en/solutions/uptodate/
- Shields J, Shields C. Retinoblastoma: introduction, genetics, clinical features, classification. In: Shields J, Shields C, Eds. Atlas of Intraocular Tumors, 3rd ed., Philadelphia: Lippinocott, Wolters Kluwer; 2016. p. 311-314.
- Ushakova TL, Тrofimov IA, Gorovtsova OV, Yarovoy AA, Saakyan SV, Letyagin IA, et al. A new era of organ-preserving treatment in pediatric intraocular retinoblastoma in Russia: a multicenter cohort study. Oncopediatrics 2018;5(1):51-69. (In Russian).
doi: 10.15690/onco.v5i1.1866 - Dimaras H, Corson TW, Cobrinik D, White A, Zhao J, Munier FL, Abramson DH, Shields CL, Chantada GL, Njuguna F, Gallie BL. Retinoblastoma. Nat Rev Dis Primers. 2015 Aug 27;1:15021. doi: 10.1038/nrdp.2015.21
- Retinoblastoma: Clinical Guidelines (Russian Society of Pediatric Oncologists, Assocoation of Ophtalmologists). 2017; ID: КР71 (In Russian).
- Shields CL, Shields JA. Recent developments in the management of retinoblastoma. J Pediat Ophthalmol Strabismus. 1999; 36(1): 8-18. PMID: 9972509X
- Lee S, Yoo K, Sung K Kim J, Cho E, Koo H, Chung S, Kang S, Oh S, Ham D, Kim Y. Tandem high-dose chemotherapy and autologous stem cell rescue in children with bilateral advanced retinoblastoma. Bone Marrow Transplant. 2008; 42(6): 385-391.
doi: 10.1038/bmt.2008.181 - Matsubara H, Makimoto A, Higa T, Kawamoto H, Sakiyama S, Hosono A, Takayama J, Takaue Y, Murayama S, Sumi M, Kaneko A, Ohira M. A multidisciplinary treatment strategy that includes high-dose chemotherapy for metastatic retinoblastoma without CNS involvement. Bone Marrow Transplant. 2005; 35 (8): 763-766. doi: 10.1038/sj.bmt.1704882
- Ancona-Lezama D, Dalvin L, Shields C. Modern treatment of retinoblastoma: A 2020 review. Ind J Ophthalmol. 2020; 68(11):2356-2365. doi: 10.4103/ijo.IJO_721_20
- White L. Chemotherapy for retinoblastoma: where do we go from here?: a review of published literature and meeting abstracts, including discussions during the Vth International Symposium on Retinoblastoma, Oct 1991. Ophthalmic Paediatr Genet. 1991; 12(3): 115-130. doi: 10.3109/13816819109029393
- Seeger RC, Reynolds CP. Treatment of high-risk solid tumors of childhood with intensive therapy and autologous bone marrow transplantation. Pediat Clin North Amer. 1991; 38: 393-424. doi: 10.1016/S0031-3955(16)38084-1
- Palma J, Sasso D, Dufort G, Koop K, Sampor C, Diez B, Richard L, Castillo L, Chantada G. Successful treatment of metastatic retinoblastoma with high-dose chemotherapy and autologous stem cell rescue in South America. Bone Marrow Transplant. 2012; 47(4): 522-527. doi: 10.1038/bmt.2011.108
- Stepanyan NG, Sidorova NV, Rubanskaya MV, Tupitsyn NN, Matinyan NV, Kirgizov KI, Varfolomeeva SR. Optimization of methods for collecting peripheral hematopoietic stem cells in children with cancer: literature review. Russian Journal of Pediatric Hematology аnd Oncology 2020;7(2):78-85. (In Russian.). doi: 10.21682/2311-1267-2020-7-2-78-85
- Mohty M, Hübel K, Kröger N, Aljurf M, Apperley J, Basak GW, Bazarbachi A, Douglas K, Gabriel I, Garderet L, et al. Autologous haematopoietic stem cell mobilisation in multiple myeloma and lymphoma patients: a position statement from the European Group for Blood and Marrow Transplantation. Вone Marrow Transplant. 2014; 49(7): 865-872. doi: 10.1038/bmt.2014.39
- Zhernyakova AA, Chubukina ZhV, Zapreeva IM, Tiranova SA, Sel’tser AV, Semenova NYu, Bessmel’tsev SS, Chechetkin AV, Gritsaev SV, Kostroma II. Hematopoietic stem cell collection in multiple myeloma patients: influence of the lenalidomide-based therapy and mobilization regimen prior to auto-HSCT II, Klinicheskaya Onkogematologiya/Clinical Oncohematology. 2018; 11(2): 192-197 (In Russian.). doi: 10.21320/2500-2139-2018-11-2-192-197
- Namouni F, Doz F, Tanguy ML, Quintana E, J Michon, Pacquement H, Bouffet E, Gentet JC, Plantaz D, Lutz P, Vannier JP, Validire P, Neuenschwander S, Desjardins L, Zucker JM. High-dose chemotherapy with carboplatin, etoposide and cyclophosphamide followed by a haematopoietic stem cell rescue in patients with high-risk retinoblastoma: a SFOP and SFGM study. Eur J Cancer. 1997; 33(14): 2368-2375. doi: 10.1016/s0959-8049(97)10019-3
- Kremens B, Wieland R, Reinhard H, Neubert D, Beck JD, Klingebiel T, Bornfeld N, Havers W. Retinoblastoma: High-dose chemotherapy with autologous stem cell rescue in children with retinoblastoma; Bone Marrow Transplant. 2003; 31, 281-284.
doi: 10.1038/sj.bmt.1703832 - Clarissa A, Sutandi N, Abdul Fath A. Stem-cell therapy following high-dose chemotherapy in advanced retinoblastoma: A systematic review. Asia-Pacific J Ophthalmol. 2021; 10(4): 397-407. doi: 10.1097/APO.0000000000000372
- Jaradat I, Mubiden R, Salem A, Abdel-Rahman F, Al-Ahmad I, Almousa A. High-dose chemotherapy followed by stem cell transplantation in the management of retinoblastoma: a systematic review. Hematol Oncol Stem Cell Ther. 2012; 5:107-117.
doi: 10.5144/1658-3876.2012.107 - Ushakova TL, Dolgopolov IS, Gorovtsova OV, Matveeva II, Pavlovskaya AI, Glekov IV, Pimenov RI, Boyarshinov VK, Mentkevich GL, Polyakov VG. Analysis of treatment outcomes for high-risk retinoblastoma. Pediatric Oncology. 2009; 3-4: 61-67. (In Russian).
- Yamanaka R, Hayano A, Takashima Y. Trilateral retinoblastoma: A systematic review of 211 cases. Neurosurg Rev. 2019; 42(1):39-48. doi: 10.1007/s10143-017-0890-4
- Carreras E, Dufour C, Mohty M, Kroger N. Hematopoietic stem cell transplantation and cellular therapies. EBMT Handbook, 2019:117-130.
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "10" ["~SORT"]=> string(2) "10" ["CODE"]=> string(100) "vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr" ["~CODE"]=> string(100) "vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr" ["EXTERNAL_ID"]=> string(4) "2050" ["~EXTERNAL_ID"]=> string(4) "2050" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(463) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаевHigh-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(3815) "<p style="text-align: justify;">Ретинобластома (РБ) – самое частое злокачественное новообразование (ЗНО) органа зрения у детей, составляет 10-15% от всех ЗНО детей первого года жизни. Несмотря на наличие стандартных подходов к лечению детей с РБ, в ряде случаев стандартные методы могут оказаться неэффективными, что требует поиска новых стратегий для улучшения выживаемости у детей группы высокого риска. В качестве интенсификации может использоваться высокодозная химиотерапия с последующей аутологичной трансплантацией гемопоэтических стволовых клеток (ауто-ТГСК). Цель нашей работы – демонстрация опыта НМИЦ онкологии им. Н. Н. Блохина на примере случаев ауто-ТГСК у пациентов с РБ.</p> <h3>Материалы и методы</h3> <p style="text-align: justify;">В 2021 г. в НИИ детской онкологии и гематологии НМИЦ онкологии им. Н. Н. Блохина 3 пациента с РБ высокой группы риска получили в режиме кондиционирования: Карбоплатин 1250 мг/кв.м., Этопозид 1750 мг/кв.м., Циклофосфамид 6 гр/кв.м. с последующей ауто-ТГСК.</p> <h3>Результаты</h3> <p style="text-align: justify;">Восстановление гемопоэза произошло на 11, 14 и 17 сутки после ауто-ТГСК. Осложнения раннего посттрансплантационного периода: орофарингеальный мукозит, нейтропенический энтероколит, фебрильная нейтропения. В периоде кондиционирования у одного пациента зафискирован эпизод тонико-клонических судорог на фоне гипонатриемии, эпизод купирован, более не повторялся. У одного пациента констатирована прогрессия заболевания, что привело к летальному исходу. Два пациента – без признаков рецидива. Медиана наблюдения 6 ( 4-10) месяцев.</p> <h3>Выводы</h3> <p style="text-align: justify;">Ауто-ТГСК для пациентов с РБ группы высокого риска может рассматриваться как консолидация, в виду хорошей переносимости и эффективности. Требуется включение в исследование большего числа пациентов, длительное наблюдение, а также обмен опытом между трансплантационными центрами.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Аутологичная трансплантация гемопоэтических стволовых клеток, ретинобластома, дети, высокодозная химиотерапия.</p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_META_TITLE"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_META_KEYWORDS"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_META_DESCRIPTION"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_PICTURE_FILE_ALT"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_PICTURE_FILE_TITLE"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_PICTURE_FILE_NAME"]=> string(100) "vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(320) "Высокодозная химиотерапия с аутологичной трансплантацией гемопоэтических стволовых клеток при ретинобластоме у детей. Обзор литературы и демонстрация клинических случаев" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(100) "vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(100) "vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(100) "vysokodoznaya-khimioterapiya-s-autologichnoy-transplantatsiey-gemopoeticheskikh-stvolovykh-kletok-pr" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "206" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28503" ["VALUE"]=> string(22) "01/15/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/15/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28504" ["VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28505" ["VALUE"]=> array(2) { ["TEXT"]=> string(919) "<p>Карина А. Сергеенко<sup>1,3</sup>, Яна Ю. Докучаева<sup>1</sup>, Ирина О. Костарева<sup>1</sup>, Тим З. Алиев<sup>1</sup>, Анна Ю. Елфимова<sup>1</sup>, Николай Г. Степанян<sup>1</sup>, Юрий В. Лозован<sup>1</sup>, Наталья А. Бурлака<sup>1</sup>, Наталья В. Сидорова<sup>2</sup>, Елена Б. Мачнева<sup>1,2</sup>, Татьяна В. Горбунова<sup>1,5</sup>, Татьяна Л. Ушакова<sup>1,3</sup>, Владимир Г. Поляков<sup>1,3,4,5</sup>, Кирилл И. Киргизов<sup>1,5</sup>, Светлана Р. Варфоломеева<sup>1,2,5</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(727) "
Карина А. Сергеенко1,3, Яна Ю. Докучаева1, Ирина О. Костарева1, Тим З. Алиев1, Анна Ю. Елфимова1, Николай Г. Степанян1, Юрий В. Лозован1, Наталья А. Бурлака1, Наталья В. Сидорова2, Елена Б. Мачнева1,2, Татьяна В. Горбунова1,5, Татьяна Л. Ушакова1,3, Владимир Г. Поляков1,3,4,5, Кирилл И. Киргизов1,5, Светлана Р. Варфоломеева1,2,5
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28506" ["VALUE"]=> array(2) { ["TEXT"]=> string(1283) "<p><sup>1</sup> ФГБУ «Национальный медицинский исследовательский центр онкологии им. Н. Н. Блохина» Минздрава России, Москва, Россия<br> <sup>2</sup> Обособленное структурное подразделение Российская детская клиническая больница ФГАОУ ВО «РНИМУ им. Н. И. Пирогова» Минздрава России, Москва, Россия<br> <sup>3</sup> ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования», Москва, Россия<br> <sup>4</sup> ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н. И. Пирогова» Минздрава России, Москва, Россия<br> <sup>5</sup> Кафедра последипломного образования врачей НМИЦ онкологии им. Н. Н. Блохина, Москва, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1187) "1 ФГБУ «Национальный медицинский исследовательский центр онкологии им. Н. Н. Блохина» Минздрава России, Москва, Россия
2 Обособленное структурное подразделение Российская детская клиническая больница ФГАОУ ВО
«РНИМУ им. Н. И. Пирогова» Минздрава России, Москва, Россия
3 ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования», Москва, Россия
4 ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н. И. Пирогова» Минздрава России, Москва, Россия
5 Кафедра последипломного образования врачей НМИЦ онкологии им. Н. Н. Блохина, Москва, Россия
Ретинобластома (РБ) – самое частое злокачественное новообразование (ЗНО) органа зрения у детей, составляет 10-15% от всех ЗНО детей первого года жизни. Несмотря на наличие стандартных подходов к лечению детей с РБ, в ряде случаев стандартные методы могут оказаться неэффективными, что требует поиска новых стратегий для улучшения выживаемости у детей группы высокого риска. В качестве интенсификации может использоваться высокодозная химиотерапия с последующей аутологичной трансплантацией гемопоэтических стволовых клеток (ауто-ТГСК). Цель нашей работы – демонстрация опыта НМИЦ онкологии им. Н. Н. Блохина на примере случаев ауто-ТГСК у пациентов с РБ.
Материалы и методы
В 2021 г. в НИИ детской онкологии и гематологии НМИЦ онкологии им. Н. Н. Блохина 3 пациента с РБ высокой группы риска получили в режиме кондиционирования: Карбоплатин 1250 мг/кв.м., Этопозид 1750 мг/кв.м., Циклофосфамид 6 гр/кв.м. с последующей ауто-ТГСК.
Результаты
Восстановление гемопоэза произошло на 11, 14 и 17 сутки после ауто-ТГСК. Осложнения раннего посттрансплантационного периода: орофарингеальный мукозит, нейтропенический энтероколит, фебрильная нейтропения. В периоде кондиционирования у одного пациента зафискирован эпизод тонико-клонических судорог на фоне гипонатриемии, эпизод купирован, более не повторялся. У одного пациента констатирована прогрессия заболевания, что привело к летальному исходу. Два пациента – без признаков рецидива. Медиана наблюдения 6 ( 4-10) месяцев.
Выводы
Ауто-ТГСК для пациентов с РБ группы высокого риска может рассматриваться как консолидация, в виду хорошей переносимости и эффективности. Требуется включение в исследование большего числа пациентов, длительное наблюдение, а также обмен опытом между трансплантационными центрами.
Ключевые слова
Аутологичная трансплантация гемопоэтических стволовых клеток, ретинобластома, дети, высокодозная химиотерапия.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28508" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2022-11-1-6-12" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2022-11-1-6-12" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28511" ["VALUE"]=> array(2) { ["TEXT"]=> string(705) "<p>Karina A. Sergeenko<sup>1,3</sup>, Yana Yu. Dokuchaeva<sup>1</sup>, Irina O. Kostareva<sup>1</sup>, Tim Z. Aliev<sup>1</sup>, Anna Yu. Elfimova<sup>1</sup>, Nikolay G. Stepanian<sup>1</sup>, Yury V. Lozovan<sup>1</sup>, Natalya A. Burlaka<sup>1</sup>, Natalya V. Sidorova<sup>2</sup>, Elena B. Machneva<sup>1,2</sup>, Tatyana V. Gorbunova<sup>1,5</sup>, Tatyana L. Ushakova<sup>1,3</sup>, Vladimir G. Polyakov<sup>1,3,4,5</sup>, Kirill I. Kirgizov<sup>1,5</sup>, Svetlana R. Varfolomeeva<sup>1,2,5</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(513) "Karina A. Sergeenko1,3, Yana Yu. Dokuchaeva1, Irina O. Kostareva1, Tim Z. Aliev1, Anna Yu. Elfimova1, Nikolay G. Stepanian1, Yury V. Lozovan1, Natalya A. Burlaka1, Natalya V. Sidorova2, Elena B. Machneva1,2, Tatyana V. Gorbunova1,5, Tatyana L. Ushakova1,3, Vladimir G. Polyakov1,3,4,5, Kirill I. Kirgizov1,5, Svetlana R. Varfolomeeva1,2,5
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28512" ["VALUE"]=> array(2) { ["TEXT"]=> string(1198) "<p><sup>1</sup> N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia<br> <sup>2</sup> Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia<br> <sup>3</sup> Russian Medical Academy for Continuous Professional Education, Moscow, Russia <br> <sup>4</sup> N. I. Pirogov Russian National Medical University, Moscow, Russia <br> <sup>5</sup> Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia<br> E-mail: karina_s19@mail.ru</p><br> <p><b>Citation:</b> Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1030) "1 N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
2 Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia
3 Russian Medical Academy for Continuous Professional Education, Moscow, Russia
4 N. I. Pirogov Russian National Medical University, Moscow, Russia
5 Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
Correspondence:
Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia
E-mail: karina_s19@mail.ru
Citation: Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28513" ["VALUE"]=> array(2) { ["TEXT"]=> string(2198) "<p style="text-align: justify;">Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.</p> <h3>Materials and methods</h3> <p style="text-align: justify;">In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m<sup>2</sup>), etoposide (1750 mg/m<sup>2</sup>), and cyclophosphamide (6000 mg/m<sup>2</sup>) with subsequent auto-HSCT. </p> <h3>Results</h3> <p style="text-align: justify;">All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.</p> <h3>Conclusions</h3> <p style="text-align: justify;">The high-dose consolidation with subsequent auto- HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.</p> <h2>Keywords</h2> <p style="text-align: justify;">Autologous hematopoietic stem cell transplantation, retinoblastoma, children, high-dose chemotherapy.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2004) "Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.
Materials and methods
In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m2), etoposide (1750 mg/m2), and cyclophosphamide (6000 mg/m2) with subsequent auto-HSCT.
Results
All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.
Conclusions
The high-dose consolidation with subsequent auto- HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.
Keywords
Autologous hematopoietic stem cell transplantation, retinoblastoma, children, high-dose chemotherapy.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28509" ["VALUE"]=> string(143) "High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(143) "High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28510" ["VALUE"]=> string(4) "2761" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2761" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28514" ["VALUE"]=> string(4) "2764" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2764" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(10) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28511" ["VALUE"]=> array(2) { ["TEXT"]=> string(705) "<p>Karina A. Sergeenko<sup>1,3</sup>, Yana Yu. Dokuchaeva<sup>1</sup>, Irina O. Kostareva<sup>1</sup>, Tim Z. Aliev<sup>1</sup>, Anna Yu. Elfimova<sup>1</sup>, Nikolay G. Stepanian<sup>1</sup>, Yury V. Lozovan<sup>1</sup>, Natalya A. Burlaka<sup>1</sup>, Natalya V. Sidorova<sup>2</sup>, Elena B. Machneva<sup>1,2</sup>, Tatyana V. Gorbunova<sup>1,5</sup>, Tatyana L. Ushakova<sup>1,3</sup>, Vladimir G. Polyakov<sup>1,3,4,5</sup>, Kirill I. Kirgizov<sup>1,5</sup>, Svetlana R. Varfolomeeva<sup>1,2,5</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(513) "Karina A. Sergeenko1,3, Yana Yu. Dokuchaeva1, Irina O. Kostareva1, Tim Z. Aliev1, Anna Yu. Elfimova1, Nikolay G. Stepanian1, Yury V. Lozovan1, Natalya A. Burlaka1, Natalya V. Sidorova2, Elena B. Machneva1,2, Tatyana V. Gorbunova1,5, Tatyana L. Ushakova1,3, Vladimir G. Polyakov1,3,4,5, Kirill I. Kirgizov1,5, Svetlana R. Varfolomeeva1,2,5
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(513) "Karina A. Sergeenko1,3, Yana Yu. Dokuchaeva1, Irina O. Kostareva1, Tim Z. Aliev1, Anna Yu. Elfimova1, Nikolay G. Stepanian1, Yury V. Lozovan1, Natalya A. Burlaka1, Natalya V. Sidorova2, Elena B. Machneva1,2, Tatyana V. Gorbunova1,5, Tatyana L. Ushakova1,3, Vladimir G. Polyakov1,3,4,5, Kirill I. Kirgizov1,5, Svetlana R. Varfolomeeva1,2,5
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28513" ["VALUE"]=> array(2) { ["TEXT"]=> string(2198) "<p style="text-align: justify;">Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.</p> <h3>Materials and methods</h3> <p style="text-align: justify;">In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m<sup>2</sup>), etoposide (1750 mg/m<sup>2</sup>), and cyclophosphamide (6000 mg/m<sup>2</sup>) with subsequent auto-HSCT. </p> <h3>Results</h3> <p style="text-align: justify;">All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.</p> <h3>Conclusions</h3> <p style="text-align: justify;">The high-dose consolidation with subsequent auto- HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.</p> <h2>Keywords</h2> <p style="text-align: justify;">Autologous hematopoietic stem cell transplantation, retinoblastoma, children, high-dose chemotherapy.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2004) "Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.
Materials and methods
In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m2), etoposide (1750 mg/m2), and cyclophosphamide (6000 mg/m2) with subsequent auto-HSCT.
Results
All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.
Conclusions
The high-dose consolidation with subsequent auto- HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.
Keywords
Autologous hematopoietic stem cell transplantation, retinoblastoma, children, high-dose chemotherapy.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(2004) "Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.
Materials and methods
In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m2), etoposide (1750 mg/m2), and cyclophosphamide (6000 mg/m2) with subsequent auto-HSCT.
Results
All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.
Conclusions
The high-dose consolidation with subsequent auto- HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.
Keywords
Autologous hematopoietic stem cell transplantation, retinoblastoma, children, high-dose chemotherapy.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28508" ["VALUE"]=> string(37) "10.18620/ctt-1866-8836-2022-11-1-6-12" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(37) "10.18620/ctt-1866-8836-2022-11-1-6-12" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(37) "10.18620/ctt-1866-8836-2022-11-1-6-12" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28509" ["VALUE"]=> string(143) "High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(143) "High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(143) "High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28512" ["VALUE"]=> array(2) { ["TEXT"]=> string(1198) "<p><sup>1</sup> N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia<br> <sup>2</sup> Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia<br> <sup>3</sup> Russian Medical Academy for Continuous Professional Education, Moscow, Russia <br> <sup>4</sup> N. I. Pirogov Russian National Medical University, Moscow, Russia <br> <sup>5</sup> Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia<br> E-mail: karina_s19@mail.ru</p><br> <p><b>Citation:</b> Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1030) "1 N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
2 Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia
3 Russian Medical Academy for Continuous Professional Education, Moscow, Russia
4 N. I. Pirogov Russian National Medical University, Moscow, Russia
5 Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
Correspondence:
Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia
E-mail: karina_s19@mail.ru
Citation: Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(1030) "1 N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
2 Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia
3 Russian Medical Academy for Continuous Professional Education, Moscow, Russia
4 N. I. Pirogov Russian National Medical University, Moscow, Russia
5 Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
Correspondence:
Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia
E-mail: karina_s19@mail.ru
Citation: Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28505" ["VALUE"]=> array(2) { ["TEXT"]=> string(919) "<p>Карина А. Сергеенко<sup>1,3</sup>, Яна Ю. Докучаева<sup>1</sup>, Ирина О. Костарева<sup>1</sup>, Тим З. Алиев<sup>1</sup>, Анна Ю. Елфимова<sup>1</sup>, Николай Г. Степанян<sup>1</sup>, Юрий В. Лозован<sup>1</sup>, Наталья А. Бурлака<sup>1</sup>, Наталья В. Сидорова<sup>2</sup>, Елена Б. Мачнева<sup>1,2</sup>, Татьяна В. Горбунова<sup>1,5</sup>, Татьяна Л. Ушакова<sup>1,3</sup>, Владимир Г. Поляков<sup>1,3,4,5</sup>, Кирилл И. Киргизов<sup>1,5</sup>, Светлана Р. Варфоломеева<sup>1,2,5</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(727) "Карина А. Сергеенко1,3, Яна Ю. Докучаева1, Ирина О. Костарева1, Тим З. Алиев1, Анна Ю. Елфимова1, Николай Г. Степанян1, Юрий В. Лозован1, Наталья А. Бурлака1, Наталья В. Сидорова2, Елена Б. Мачнева1,2, Татьяна В. Горбунова1,5, Татьяна Л. Ушакова1,3, Владимир Г. Поляков1,3,4,5, Кирилл И. Киргизов1,5, Светлана Р. Варфоломеева1,2,5
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(727) "Карина А. Сергеенко1,3, Яна Ю. Докучаева1, Ирина О. Костарева1, Тим З. Алиев1, Анна Ю. Елфимова1, Николай Г. Степанян1, Юрий В. Лозован1, Наталья А. Бурлака1, Наталья В. Сидорова2, Елена Б. Мачнева1,2, Татьяна В. Горбунова1,5, Татьяна Л. Ушакова1,3, Владимир Г. Поляков1,3,4,5, Кирилл И. Киргизов1,5, Светлана Р. Варфоломеева1,2,5
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28503" ["VALUE"]=> string(22) "01/15/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/15/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "01/15/2022 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28504" ["VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "02/18/2022 12:00:00 am" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28507" ["VALUE"]=> array(2) { ["TEXT"]=> string(3815) "<p style="text-align: justify;">Ретинобластома (РБ) – самое частое злокачественное новообразование (ЗНО) органа зрения у детей, составляет 10-15% от всех ЗНО детей первого года жизни. Несмотря на наличие стандартных подходов к лечению детей с РБ, в ряде случаев стандартные методы могут оказаться неэффективными, что требует поиска новых стратегий для улучшения выживаемости у детей группы высокого риска. В качестве интенсификации может использоваться высокодозная химиотерапия с последующей аутологичной трансплантацией гемопоэтических стволовых клеток (ауто-ТГСК). Цель нашей работы – демонстрация опыта НМИЦ онкологии им. Н. Н. Блохина на примере случаев ауто-ТГСК у пациентов с РБ.</p> <h3>Материалы и методы</h3> <p style="text-align: justify;">В 2021 г. в НИИ детской онкологии и гематологии НМИЦ онкологии им. Н. Н. Блохина 3 пациента с РБ высокой группы риска получили в режиме кондиционирования: Карбоплатин 1250 мг/кв.м., Этопозид 1750 мг/кв.м., Циклофосфамид 6 гр/кв.м. с последующей ауто-ТГСК.</p> <h3>Результаты</h3> <p style="text-align: justify;">Восстановление гемопоэза произошло на 11, 14 и 17 сутки после ауто-ТГСК. Осложнения раннего посттрансплантационного периода: орофарингеальный мукозит, нейтропенический энтероколит, фебрильная нейтропения. В периоде кондиционирования у одного пациента зафискирован эпизод тонико-клонических судорог на фоне гипонатриемии, эпизод купирован, более не повторялся. У одного пациента констатирована прогрессия заболевания, что привело к летальному исходу. Два пациента – без признаков рецидива. Медиана наблюдения 6 ( 4-10) месяцев.</p> <h3>Выводы</h3> <p style="text-align: justify;">Ауто-ТГСК для пациентов с РБ группы высокого риска может рассматриваться как консолидация, в виду хорошей переносимости и эффективности. Требуется включение в исследование большего числа пациентов, длительное наблюдение, а также обмен опытом между трансплантационными центрами.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Аутологичная трансплантация гемопоэтических стволовых клеток, ретинобластома, дети, высокодозная химиотерапия.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3657) "Ретинобластома (РБ) – самое частое злокачественное новообразование (ЗНО) органа зрения у детей, составляет 10-15% от всех ЗНО детей первого года жизни. Несмотря на наличие стандартных подходов к лечению детей с РБ, в ряде случаев стандартные методы могут оказаться неэффективными, что требует поиска новых стратегий для улучшения выживаемости у детей группы высокого риска. В качестве интенсификации может использоваться высокодозная химиотерапия с последующей аутологичной трансплантацией гемопоэтических стволовых клеток (ауто-ТГСК). Цель нашей работы – демонстрация опыта НМИЦ онкологии им. Н. Н. Блохина на примере случаев ауто-ТГСК у пациентов с РБ.
Материалы и методы
В 2021 г. в НИИ детской онкологии и гематологии НМИЦ онкологии им. Н. Н. Блохина 3 пациента с РБ высокой группы риска получили в режиме кондиционирования: Карбоплатин 1250 мг/кв.м., Этопозид 1750 мг/кв.м., Циклофосфамид 6 гр/кв.м. с последующей ауто-ТГСК.
Результаты
Восстановление гемопоэза произошло на 11, 14 и 17 сутки после ауто-ТГСК. Осложнения раннего посттрансплантационного периода: орофарингеальный мукозит, нейтропенический энтероколит, фебрильная нейтропения. В периоде кондиционирования у одного пациента зафискирован эпизод тонико-клонических судорог на фоне гипонатриемии, эпизод купирован, более не повторялся. У одного пациента констатирована прогрессия заболевания, что привело к летальному исходу. Два пациента – без признаков рецидива. Медиана наблюдения 6 ( 4-10) месяцев.
Выводы
Ауто-ТГСК для пациентов с РБ группы высокого риска может рассматриваться как консолидация, в виду хорошей переносимости и эффективности. Требуется включение в исследование большего числа пациентов, длительное наблюдение, а также обмен опытом между трансплантационными центрами.
Ключевые слова
Аутологичная трансплантация гемопоэтических стволовых клеток, ретинобластома, дети, высокодозная химиотерапия.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(3657) "Ретинобластома (РБ) – самое частое злокачественное новообразование (ЗНО) органа зрения у детей, составляет 10-15% от всех ЗНО детей первого года жизни. Несмотря на наличие стандартных подходов к лечению детей с РБ, в ряде случаев стандартные методы могут оказаться неэффективными, что требует поиска новых стратегий для улучшения выживаемости у детей группы высокого риска. В качестве интенсификации может использоваться высокодозная химиотерапия с последующей аутологичной трансплантацией гемопоэтических стволовых клеток (ауто-ТГСК). Цель нашей работы – демонстрация опыта НМИЦ онкологии им. Н. Н. Блохина на примере случаев ауто-ТГСК у пациентов с РБ.
Материалы и методы
В 2021 г. в НИИ детской онкологии и гематологии НМИЦ онкологии им. Н. Н. Блохина 3 пациента с РБ высокой группы риска получили в режиме кондиционирования: Карбоплатин 1250 мг/кв.м., Этопозид 1750 мг/кв.м., Циклофосфамид 6 гр/кв.м. с последующей ауто-ТГСК.
Результаты
Восстановление гемопоэза произошло на 11, 14 и 17 сутки после ауто-ТГСК. Осложнения раннего посттрансплантационного периода: орофарингеальный мукозит, нейтропенический энтероколит, фебрильная нейтропения. В периоде кондиционирования у одного пациента зафискирован эпизод тонико-клонических судорог на фоне гипонатриемии, эпизод купирован, более не повторялся. У одного пациента констатирована прогрессия заболевания, что привело к летальному исходу. Два пациента – без признаков рецидива. Медиана наблюдения 6 ( 4-10) месяцев.
Выводы
Ауто-ТГСК для пациентов с РБ группы высокого риска может рассматриваться как консолидация, в виду хорошей переносимости и эффективности. Требуется включение в исследование большего числа пациентов, длительное наблюдение, а также обмен опытом между трансплантационными центрами.
Ключевые слова
Аутологичная трансплантация гемопоэтических стволовых клеток, ретинобластома, дети, высокодозная химиотерапия.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28506" ["VALUE"]=> array(2) { ["TEXT"]=> string(1283) "<p><sup>1</sup> ФГБУ «Национальный медицинский исследовательский центр онкологии им. Н. Н. Блохина» Минздрава России, Москва, Россия<br> <sup>2</sup> Обособленное структурное подразделение Российская детская клиническая больница ФГАОУ ВО «РНИМУ им. Н. И. Пирогова» Минздрава России, Москва, Россия<br> <sup>3</sup> ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования», Москва, Россия<br> <sup>4</sup> ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н. И. Пирогова» Минздрава России, Москва, Россия<br> <sup>5</sup> Кафедра последипломного образования врачей НМИЦ онкологии им. Н. Н. Блохина, Москва, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1187) "1 ФГБУ «Национальный медицинский исследовательский центр онкологии им. Н. Н. Блохина» Минздрава России, Москва, Россия
2 Обособленное структурное подразделение Российская детская клиническая больница ФГАОУ ВО
«РНИМУ им. Н. И. Пирогова» Минздрава России, Москва, Россия
3 ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования», Москва, Россия
4 ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н. И. Пирогова» Минздрава России, Москва, Россия
5 Кафедра последипломного образования врачей НМИЦ онкологии им. Н. Н. Блохина, Москва, Россия
1 ФГБУ «Национальный медицинский исследовательский центр онкологии им. Н. Н. Блохина» Минздрава России, Москва, Россия
2 Обособленное структурное подразделение Российская детская клиническая больница ФГАОУ ВО
«РНИМУ им. Н. И. Пирогова» Минздрава России, Москва, Россия
3 ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования», Москва, Россия
4 ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н. И. Пирогова» Минздрава России, Москва, Россия
5 Кафедра последипломного образования врачей НМИЦ онкологии им. Н. Н. Блохина, Москва, Россия
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is the only available curative option for acute leukemia nowadays. Many different parameters have significant impact on the final results of HSCT, especially on the more recently defined graft-versus-host disease (GvHD)-free/relapse-free survival (GFRFS) rate, including the pre-HSCT characteristics, such as disease profile at diagnosis and the disease status at the time of transplant, as well as the peri-HSCT factors, i.e. donor type, stem cell source, implemented conditioning regimen and potential post-transplant complications. Aiming to reduce the relapse rates after HSCT, myeloablative conditioning (MAC) regimens at higher dose intensity using busulfan or total body irradiation (TBI) has shown promising results [1]. However, due to higher vulnerability of younger patients to adverse effects of therapeutic irradiation, MAC regimens without TBI are preferred [2, 3]. Moreover, in view of relative complexity for bone marrow collection procedure, along with potentially enhanced graft-versus-leukemia (GvL) effect, peripheral blood (PB) is the preferred source of stem cells for allogeneic HSCT ever more. On the other hand, the increasing number of transplants from human leukocyte antigen (HLA)-haploidentical donors in the patients with acute leukemia is performed due to the absence of suitable related or unrelated HLA-matched donors, thus raising the necessity of understanding, whether HSCT outcomes with this approach are similar to those of more common modes. Over last years, several reports have shown comparable outcomes between HSCT from haploidentical donors and historical HLA-matched related or unrelated donors [4-6]. Hence, additional reports regarding the comparison of different donor types could be a guide to the upcoming therapeutic strategies. To address this issue, we carried out a single-center study, using HSCT with radiation-free MAC regimen, in order to evaluate the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) performed from matched and mismatched related and unrelated donors compared with haploidentical donors in children, adolescents and young adults (CAYA) affected by acute leukemia.
Patients and methods
Patient characteristics
Our study included 180 patients who underwent first allogeneic HSCT for acute leukemia in the CAYA HSCT Department of the Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Tehran, Iran, between January 2014 and January 2021. All data were retrieved retrospectively from clinical records according to the policy approved by the Committee for Medical Ethics of Tehran University of Medical Sciences (TUMS) and after obtaining informed consent from the patients, or their legal guardians.
HSCT parameters
In all patients and their donors, high-resolution HLA molecular typing for HLA-A, -B, -C, -DRB1, and -DQB1 loci was performed. The first donor preference was a 10/10 HLA-matched related donor (MRD), or a 9/10 HLA-mismatched related donor (MMRD). In absence of related donors, an alternative donor including 10/10 HLA-matched unrelated donors (MUD), or 9/10 HLA-mismatched unrelated donors (MMUD), or a related haploidentical donor (Haplo) was chosen, depending on their availability and accessibility.
We proceeded to HSCT if the result of a pre-HSCT bone marrow examination pointed to morphologically complete remission (CR), regardless of the minimal residual disease status. The HSCT procedure was based on irradiation-free MAC regimen including busulfan (a total dose of 3.2-4.8 mg/kg/day, according to patients' ideal body weight, from day -6 to -3), and cyclophosphamide (60 mg/kg/day, day -2 to -1). The GvHD prophylaxis was based on administration of cyclosporine A (CsA) in all the patients, and a short course of methotrexate (10 mg/m2 on day +1, 6 mg/m2 on day +3, +6, and +11) in HSCT from matched and mismatched related and unrelated donors, plus rabbit anti-human thymocytes globulins (ATG-Thymoglobuline, Sanofi, 2.5 mg/kg/day from days -3 to -1) in MMRD, MUD/MMUD and haplo-HSCT groups, and high-dose Pt-Cy treatment (40 mg/kg/day on days +3 and +4) in the Haplo group. We only included patients who received unmanipulated peripheral blood hematopoietic stem cells as graft source.
Considering hazards of CMV reactivation after HSCT, the patients were classified, according to their serological status, into low-risk (donor [D]-/recipient [R]-), intermediate-risk (D+/R-), or high-risk groups (D-/R+ or D+/R+) [7].
Definitions and endpoints
The main purpose of this study was to compare the survival rates of acute leukemia patients who had undergone allogeneic HSCT from different donor types. Overall survival (OS) was defined as the probability of survival, irrespective of the disease state at any point in time. GvHD-free/relapse-free survival (GFRFS) which is regarded as an endpoint more precisely reflective of health status and quality of life post-transplant, was defined as the probability of survival at complete remission of the disease, with sustained donor cell engraftment and absence of either grade III–IV acute GvHD, or chronic GvHD requiring immunosuppressive treatment [8]. Non-relapse mortality (NRM) was defined as probability of death without a relapse after HSCT. The relapse incidence (RI) was defined as the probability to develop a disease relapse.
Donor chimerism was determined on day +15, +30, +60 and +90 after HSCT, and then, if clinically indicated, in whole bone marrow mononuclear cells by means of quantitative PCR of informative short tandem repeats in the donor and recipient [9]. Sustained donor cell engraftment was defined at >0.5×109/L neutrophils and >20×109/L platelets for three consecutive days without blood transfusion support. Graft rejection was defined as a lack of initial engraftment of donor cells (primary), or loss of donor cell engraftment (secondary graft failure), regardless of peripheral cell blood counts. Acute GvHD (aGvHD) and chronic GvHD (cGvHD) were diagnosed and graded according to the published criteria [10, 11]. The mentioned HSCT outcomes were compared between the three categorized groups of different donor types, i.e., the patients transplanted from HLA-matched related (10/10), HLA-mismatched related (9/10) donors (MRD/MMRD), HLA-matched unrelated (10/10), HLA-mismatched (9/10) unrelated donors (MUD/MMUD), and HLA-haploidentical (Haplo) donors.
Statistical evaluation
The patients followed-up beyond 36 months were censored, for better comparison between the groups because some sub-groups had shorter follow-up periods than the other sub-groups. Homogeneity within treatment pairs was evaluated using the Chi-square test or Fisher exact test for qualitative variables and Student's T-test, or Wilcoxon rank-sum test for continuous variables. The endpoints were as follows: OS, GFRFS, relapse-associated, and non-relapse mortality incidence. Kaplan-Meier curves were derived to determine OS and GFRFS, having been compared with log-rank test.
Median follow-up time was established by means of reverse Kaplan-Meier method. After selection of baseline characteristics and clinical variables based on univariable Cox proportional hazards models, multivariable Cox proportional hazards models were fitted.
Variables in the multivariable OS and GFRFS were determined, as based on the P-values of <0.2 in the univariable Cox proportional hazards models. The proportionality of hazards assumption was checked using the global proportionality of hazard test based on Schoenfeld residuals in each of the three multivariable models. There were no deviations from the proportionality of hazards assumption in all multivariable models (results not shown). To account for informative censoring in presence of multiple endpoints, the competing risks in survival analysis were evaluated with nonparametric methods using the cumulative incidence competing risk method. CI for relapses and NRM were calculated by Gray's method. Death beyond relapses was considered a competing event for relapse, and the relapse was considered a competing event for NRM. The Fine-Gray proportional hazard regression model was used to assess the effects of covariates on the relapse frequency and NRM incidence. Like multivariate Cox proportional hazard regression, all the variables at P values of <0.2 in the univariate Fine-Gray proportional hazard regression were included in appropriate multivariate analyses. A two-sided P-value of <0.05 was considered to be statistically significant. The data evaluation was done with STATA version 16 and the packages "survival" and "cmprsk" in R software version 3.3.1.
Results
Patients
The study included 180 patients (120 males and 60 females) at a median age of 12 years (4 months to 24 years) at the time of HSCT, and 123 patients (68.3%) were transplanted at the age of ≤15 years. The donor types were as follows: matched (n=103) and mismatched (n=2) relatives including siblings (n=94) and other relatives (n=11) for a total of 105 cases (58.3%); matched (n=20) and mismatched (n=10) unrelated donors (a total of 30 patients, 16.7%), and haploidentical donors for 45 patients (25%). The patients’ characteristics are summarized in Table 1.
Table 1. Characteristics of the patients and transplant procedure

Notes: ALL: acute lymphoblastic leukemia, AML: acute myeloblastic leukemia, BM: bone marrow, BM+: involvement of bone marrow together with other sites, CR: complete remission, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUD/MMUD: HLA-matched unrelated and HLA-mismatched unrelated donors, R/D: recipient/donor, WBC: white blood cell.
The median follow-up time was 28.7 months for the patients enrolled into the study who were still alive at the end of the study (range: 21.9-34.9). A total of 96 patients presented with B-cell lineage acute lymphoblastic leukemia (ALL); 22 cases, with T-lineage ALL, and 62 patients had acute myeloblastic leukemia (AML). A total of 12 patients suffered from Ph chromosome-positive ALL. All the patients were in complete hematological remission before HSCT, including 93 patients (51.7%) transplanted in their first complete remission (CR1), 67 patients (37.2%) in the second complete remission (CR2), and 20 patients (11.1%) had experienced more than 2 relapses before HSCT. A pre-HSCT cytomegalovirus (CMV) serology showed that more than 90% of the patients were at high risk (recipient [R]+, donor [D]+) for CMV reactivation after HSCT.
Donor cell engraftment
All the patients (180/180) achieved neutrophil counts over 0.5×109/L at a median time of 11 days (range: 7-16). A total of 178 patients achieved platelet counts above 20×109/L, with a median time of 11 days (range: 0-130), and 4 patients died before the platelet engraftment (Table 2). The median time for neutrophil and platelet engraftment in Haplo vs MUD/MMUD vs MRD/MMRD was 12.20 and 14.67 days vs 12.17 and 16.21 days vs 10.73 and 14.30 days, respectively. Two patients from the Haplo group experienced secondary graft failure following CMV reactivation with high viral load after HSCT; one patient was successfully rescued by the second haploidentical HSCT from the same sibling donor, whereas other patient received a second allograft from other parent followed by sustained engraftment and hematopoietic recovery.
Table 2. Engraftment terms and GVHD incidence for the different donor types
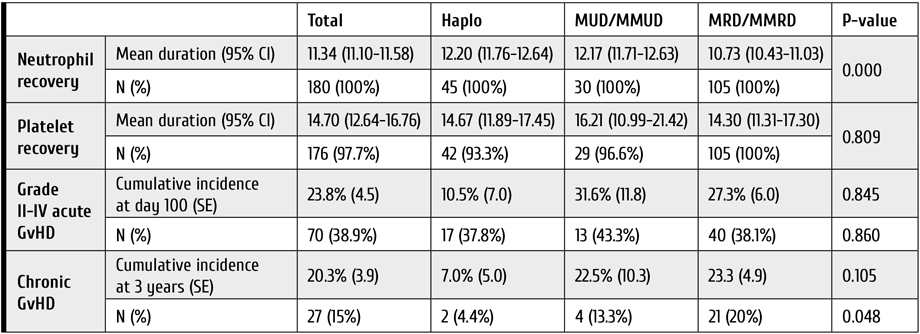
Notes: GvHD: graft-versus-host disease, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUD/MMUD: HLA-matched unrelated and HLA-mismatched unrelated donors.
Acute and chronic GVHD
Grade II to IV of aGvHD was diagnosed in 70 patients (38.9%), being developed at the median term of 15 days after HSCT. Cumulative aGVHD incidence at day 100 was highest in the MUD/MMUD group compared to Haplo and MRD/MMRD, but this difference was not statistically significant [31.6% (±11.8) versus 10.5% (±7.0) versus 27.3% (±6.0), respectively (P=0.845)].
Among 165 patients who survived more than 100 days after HSCT, 27 patients (15%) developed cGvHD, and we observed lower incidence of 3-year cGVHD in the haploidentical group compared to the MUD/MMUD group [7.0% (±5.0) versus 22.5% (±10.3), respectively]. Table 2 represents the comparison for GvHD incidence in the 3 donor types.
Relapse incidence (RI)
The 1-year and 3-year RI of the entire study population was 20.47% (95% CI 14.66-26.97) and 33.85% (95% CI 25.81-41.98), respectively. The 3-year RI in patients of the Haplo group was higher when compared to MUD/MMUD and MRD/MMRD: 40.95% (95% CI 18.41-62.44) versus 32.94% (95% CI 11.92-56.01) versus 33.17% (95% CI 23.64-42.99), respectively (Table 3). This difference was not statistically significant (P=0.902). In the Cox analysis, using both univariate and multivariate approaches, RI was not significantly different among the three donor type groups. In adjusted multivariable RI modeling, the hazard of relapse in the patients from MUD/MMUD group was only 10% lower than for the patients from Haplo group [HR=0.90 (95% CI 0.37-2.19), P=0.826].
Table 3. One- and three-year relapse incidence (RI) and non-relapse mortality (NRM) following HSCT
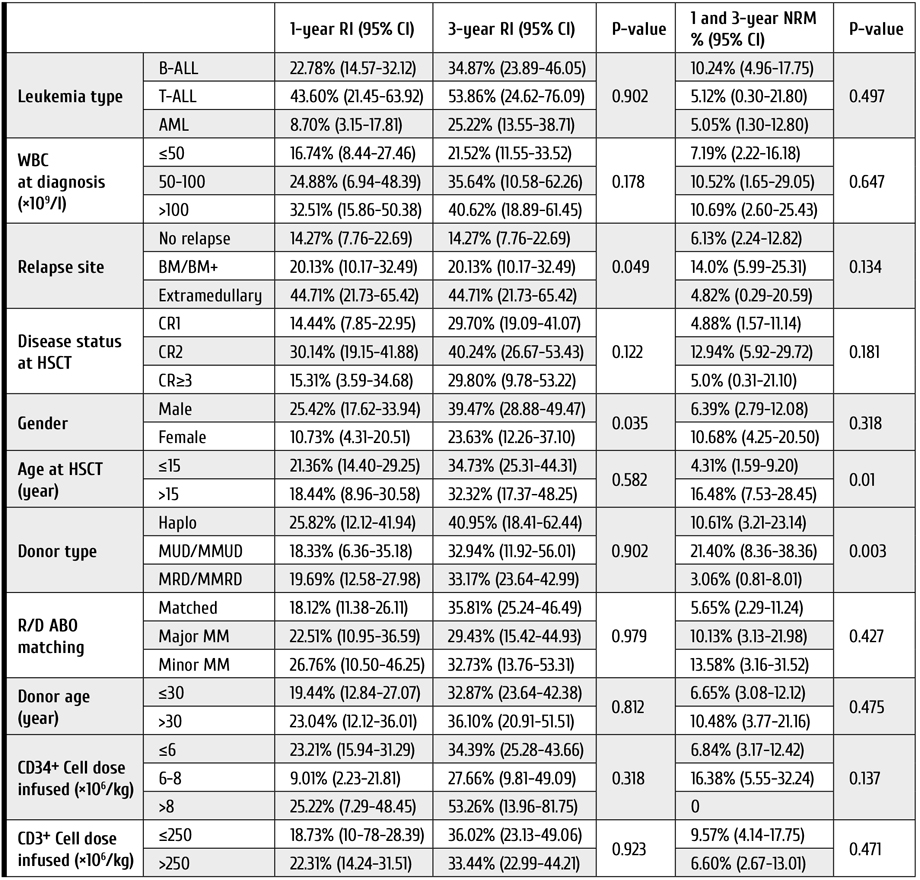
Notes: ALL: acute lymphoblastic leukemia, AML: acute myeloblastic leukemia, BM: bone marrow, BM+: involvement of bone marrow together with other sites, CR: complete remission, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUDMMUD: HLA-matched unrelated and HLA-mismatched unrelated donors, NRM: non-relapse mortality, R/D: recipient/donor, RI: relapse incidence, WBC: white blood cell.
Survival rates and post-HSCT complications
The 3-year OS and GFRFS rates for the entire study cohort were 68.81% (95% CI 60.08-76.01), and 44.19% (95% CI 35.52-54.49), respectively (Fig. 1). Patients in the MUD/MMUD group had the lowest OS and GFRFS compared to other donor types (Table 4).

Figure 1. Clinical outcomes in the cohort of young patients subjected to HSCT from different types of donors. A. Overall survival, B. GvHD-free, relapse-free survival, C. Relapse incidence, D. Non-relapse mortality of patients included in the study. Abscissa, observation terms
Note: Haplo: HLA-haploidentical donors, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUDMMUD: HLA-matched unrelated and HLA-mismatched unrelated donors.
Table 4. One- and three-year overall survival (OS) and GFRFS rates following HSCT in young patients
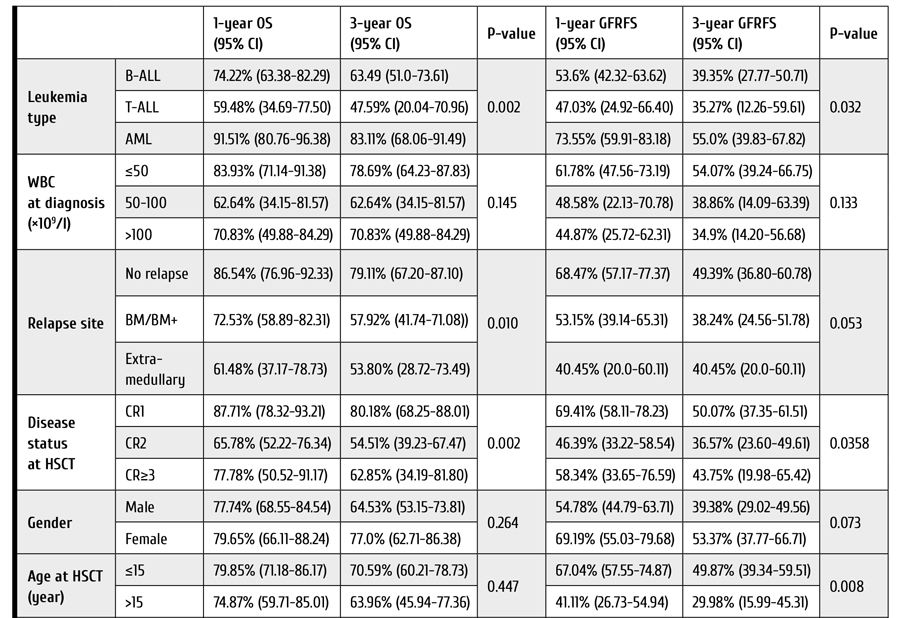

Notes: ALL: acute lymphoblastic leukemia, AML: acute myeloblastic leukemia, BM: bone marrow, BM+: involvement of bone marrow together with other sites, CR: complete remission, GFRFS: GvHD-free/relapse-free survival, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUD/MMUD: HLA-matched unrelated and HLA-mismatched.
The 3-year OS rates were 73.58% (95% CI 62.98-81.59), 54.21% (95% CI 29.61-73.49), and 64.18% (95% CI 39.76-80.79) for MRD/MMRD, MUD/MMUD, and Haplo groups, respectively (P=0.08); The 3-year GFRFS rates were 47.11% (95% CI 36.48-57.02), 30.89% (95% CI 10.70-53.80), and 42.46% (95% CI 20.41-63.01) for MRD/MMRD, MUD/MMUD, and Haplo groups, respectively (P=0.26). In the Cox analysis, using both univariate and multivariate approaches, OS and GFRFS were not significantly different among the 3 donor type groups. Adjusted multivariable modeling of OS based on the variables selected in unadjusted univariate models (see Patients and methods) showed that hazard of death in the patients who received HSCT from MUD/MMUD was about 3.6 times higher than in cases of HSCT from haploidentical donors, and this difference was statistically significant (P=0.05). Moreover, in those patients who received HSCT from MRD/MMRD, the hazard of death was 12 percent higher than for those who received HSCT from haploidentical donors [HR=1.12, (95% CI 0.34-3.67), P=0.84].
The 3-year NRM in all patients was 7.84% (95% CI 4.36-12.62). The patients who underwent MUD/MMUD HSCT showed significantly higher NRM compared to the patients who received Haplo and MRD/MMRD transplants (Table 3): 21.40% (95% CI 8.36-38.36) versus 10.61% (95% CI 3.21-23.14) versus 3.06% (95% CI 0.81-8.01), respectively (P=0.003).
Considering the causes of NRM among patients from MUD/MMUD group who died in the disease remission, we observed six cases of infection and one case of heart failure. In the Haplo group, one patient deceased from NRM had aGvHD, and four others developed infection. In the MRD/MMRD group, one patient was lost due to aGvHD, three patients died with infectious complications, and one case, due to unknown reason.
Adjusted multivariable modeling of NRM showed that hazard of death in the patients who received HSCT from MUD/MMUD was 6 times higher than the hazard of death for the patients who received HSCT from haploidentical donors. This difference was statistically significant (P=0.002). In those patients who received HSCT from MRD/MMRD, the hazard of death was not higher than in those who received HSCT from haploidentical donors (P=0.23).
Although the estimated risk of CMV reactivation prior to HSCT was high in most patients, CMV reactivation after HSCT was detected in a total of 61 cases (33.9%). CMV reactivation after HSCT occurred significantly more often in Haplo and MUD/MMUD group compared with the MRD/MMRD group (55.6% and 43.3% versus 21.9%, respectively, P=0.001). Worth of note, the CMV reactivation post-HSCT was associated with decreased OS and GFRFS in all three groups, being, however, statistically non-significant (P=0.09).
Hemorrhagic cystitis (HC) was another documented complication post-HSCT which occurred in 36 patients (20%), and it mostly affected the patients from Haplo and MUD/MMUD groups compared with MRD/MMRD group (35.6% and 33.3% versus 9.5%, respectively, P=0.000). Sinusoidal obstruction syndrome (SOS) was documented in only 5 patients, i.e. one case from Haplo group, two patients transplanted with MUD/MMUD grafts, and two, from the MRD/MMRD group.
Discussion
Allogeneic HSCT has augmented the potential of cure in patients with acute leukemia [12-15]. Although HLA-compatible related and unrelated donors have been traditionally used for treating acute leukemia patients requiring an allograft, there remains a significant proportion of patients for whom HLA-identical acceptable donor is not available. For these patients, the use of a haploidentical donor combined with alloreactive T cell elimination by Pt-Cy is the most widely adopted strategy [16]. Our study has shown that, for children, adolescents and young adults (CAYA) affected by acute leukemia, haploidentical HSCT followed by Pt-Cy may offer a better and more accessible chance of cure in terms of NRM and survival rates when compared with HSCT from unrelated donors who are hardly available, especially in the COVID-19 pandemic era.
Different studies reported that haploidentical HSCT could provide similar results to those of MUD and MMUD [17-19]. Several reports have shown, at least, comparable outcomes between Haplo and historical MRD, MUD, and MMUD series [20-23]. In our work, in consistence with most studies, the MRD/MMRD group had the best survival rates within the three donor types. Nevertheless, surprisingly, the survival rates were higher in the Haplo group compared to MUD/MMUD group.
Saglio et al., using a TBI-based conditioning regimen, have reported similar OS rates for Haplo and MUD/MMUD in CAYA patients [24]. In our study, OS rates were much higher in Haplo group compared to the MUD/MMUD group. Likewise, in our patients who had undergone haploidentical HSCT, GFRFS was higher and NRM was much lower than the results attained after HSCT from MUD/MMUD.
In terms of GvHD, it has been emphasized that Pt-Cy is able to significantly eliminate alloreactive T cells and, therefore, to reduce the incidence of GvHD, especially its acute form [25]. In addition, ATG has been shown to reduce the rates of severe acute and chronic GvHD in cases of matched or mismatched, unrelated allogeneic HSCT [26, 27]. Chronic GvHD is the leading cause of late complications and death after allogeneic HSCT. Usage of peripheral blood stem cells as a graft source presents a sufficient risk factor for its development, since the T-cell levels in allografts are higher than those in bone marrow [28-30]. Low incidence of GvHD, particularly chronic GvHD, in our patients, as compared to other reports in the literature, despite application of MAC regimen, along with usage of peripheral blood stem cells, could be attributed to high doses of ATG in the conditioning regimen for HSCT in the patients undergoing Haplo and MUD/MMUD HSCT. In our study, the rates of acute and chronic GvHD were even lower in the Haplo group than among the patients in MUD/MMUD group. This could be ascribed to dual in vivo T-cell depletion caused by ATG and Pt-Cy in the Haplo group. However, adoption of the highly effective GvHD prophylaxis may potentially lead to increased risk of relapse. It seems to be true in our study, as we had the highest relapse incidence (RI) in the Haplo group. However, one should note that the difference in RI among our three donor types was not statistically significant. It is presumed that HLA disparity could be considered a contributing factor to allo-reactivity and GvL [31]. In the matched donor transplant setting, the frequency of donor T-cell precursors directed against leukemia-specific antigens mediating GvL may be more limited [32]. Other studies with less rigorous GvHD prophylaxis strategies compared to our approaches, have reported similar RI in Haplo and MUD/MMUD HSCT [24, 34].
With respect to transplant toxicity, our data confirm that the patients undergoing Haplo HSCT have much lower NRM rates compared to patients undergoing MUD/MMUD HSCT, and the rates of complications, such as hemorrhagic cystitis and sinusoidal obstruction syndrome, seem to be comparable within the two groups. Previous studies comparing NRM rates in Haplo (with Pt-Cy) with MRD and MUD transplants (with standard GvHD prophylaxis) have reported inconsistent results. Meanwhile, some studies reported a higher NRM rates in Haplo HSCT [17, 35, 36].
This study was limited by its retrospective design, inability to adjust for unknown factors, the heterogeneity for conditioning regimens and supportive therapy that could affect the study outcomes.
Conclusions
Our study shows that inclusion of ATG into the myeloablative conditioning regimen before transplantation of peripheral blood stem cells from MUD/MMUD and Haplo donors is associated with reduced rates of chronic GvHD and graft failure, concomitantly. The rates of OS and GFRFS were higher in the Haplo group compared to MUD/MMUD, hence, our data supports the view that haploidentical HSCT with peripheral blood stem cells is a practical and valuable clinical option that offers CAYA patients with acute leukemia requiring HSCT and lacking matched available donors, a reasonable opportunity for the disease control. However, further progress is necessary to decrease the relapse rate in these patients.
Declarations
The study was approved by the Committee on Medical Ethics of Tehran University of Medical Sciences (TUMS) and informed consent was obtained from patients or their legal guardians. Authors provide a consent for publication. Primary data and materials are available on request.
Authors' contributions: TR designed and coordinated the study, and managed the patients. AK, MR and NA participated in the management of patients. AK carried out statistical evaluation. SA conceived of the study. All the authors read and approved the final manuscript.
Acknowledgements
We would like to thank Ashraf Sadat Hoseini and other nursing staff for their undeniable assistance in care for our patients.
Competing Interests
None of the authors have any relevant conflict of interest to disclaim about the present article. No funding support for the study is declared.
References
- Solomon SR, Sizemore CA, Sanacore M, Zhang X, Brown S, Holland HK, et al. Total body irradiation-based myeloablative haploidentical stem cell transplantation is a safe and effective alternative to unrelated donor transplantation in patients without matched sibling donors. Biol Blood Marrow Transplant. 2015; 21(7):1299-1307. doi: 10.1016/j.bbmt.2015.03.003
- Friebert SE, Shepardson LB, Shurin SB, Rosenthal GE, Rosenthal NS. Pediatric bone marrow cellularity: are we expecting too much?
J Pediat Hematol/Oncol. 1998; 20(5):439-43. doi: 10.1097/00043426-199809000-00006 - Muschler GF, Nitto H, Boehm CA, Easley KA. Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors. J Orthop Res. 2001; 19(1):117-125. doi: 10.1016/S0736-0266(00)00010-3
- Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant. 2014; 20(10):1573-1579.
doi: 10.1016/j.bbmt.2014.05.029 - Bashey A, Zhang XU, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013; 31(10):1310-1316. doi: 10.1200/JCO.2012.44.3523
- Di Stasi A, Milton DR, Poon LM, Hamdi A, Rondon G, Chen J, et al. Similar transplantation outcomes for acute myeloid leukemia and myelodysplastic syndrome patients with haploidentical versus 10/10 human leukocyte antigen-matched unrelated and related donors. Biol Blood Marrow Transplant. 2014; 20(12):1975-1981. doi: 10.1016/j.bbmt.2014.08.013
- George B, Pati N, Gilroy N, Ratnamohan M, Huang G, Kerridge I, Hertzberg M, Gottlieb D, Bradstock K. Pre-transplant cytomegalovirus (CMV) serostatus remains the most important determinant of CMV reactivation after allogeneic hematopoietic stem cell transplantation in the era of surveillance and preemptive therapy. Transplant Infect Dis. 2010; 12(4):322-9.
doi: 10.1111/j.1399-3062.2010.00504.x - Balavarca Y, Pearce K, Norden J, Collin M, Jackson G, Holler E, et al. Predicting survival using clinical risk scores and non-HLA immunogenetics. Bone Marrow Transpl. 2015; 50(11):1445-1452. doi: 10.1038/bmt.2015.305
- Thiede C, Florek M, Bornhäuser M, Ritter M, Mohr B, Brendel C, et al. Rapid quantification of mixed chimerism using multiplex amplification of short tandem repeat markers and fluorescence detection. Bone Marrow Transpl. 1999; 23:1055-1060.
doi: 10.1038/sj.bmt.1701779 - Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the disease risk index for allogeneic stem cell transplantation. Blood. 2014; 123:3664-3671. doi: 10.1182/blood-2014-01-552984
- Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974; 18:295-304.
- Afify Z, Hunt L, Green A, Guttridge M, Cornish J, Oakhill A. Factors affecting the outcome of stem cell transplantation from unrelated donors for childhood acute lymphoblastic leukemia in third remission. Bone Marrow Transpl. 2005; 35:1041-1047.
doi: 10.1038/sj.bmt.1704958 - Balduzzi A, Valsecchi MG, Uderzo C, De Lorenzo P, Klingebiel T, Peters C, et al. Chemotherapy versus allogeneic transplantation for very-high-risk childhood acute lymphoblastic leukaemia in first complete remission: comparison by genetic randomisation in an international prospective study. Lancet. 2005; 366:635-642. doi: 10.1016/S0140-6736(05)66998-X
- Cornish J, Oakhill A. The management of relapsed acute lymphoblastic leukaemia. Bone Marrow Transpl. 2001; 28(1):S9. https://doi.org/10.1038/sj.bmt.1703167
- Klingebiel T, Cornish J, Labopin M, Locatelli F, Darbyshire P, Handgretinger R, et al. Results and factors influencing outcome after fully haploidentical hematopoietic stem cell transplantation in children with very high-risk acute lymphoblastic leukemia: impact of center size: an analysis on behalf of the Acute Leukemia and Pediatric Disease Working Parties of the European Blood and Marrow Transplant group. Blood. 2010; 115:3437-3446. doi: 10.1182/blood-2009-03-207001
- Nagler A, Ruggeri A. Haploidentical stem cell transplantation (HaploSCT) for patients with acute leukemia – an update on behalf of the ALWP of the EBMT. Bone Marrow Transplant. 2019; 54(2): 713-718. doi: 10.1038/s41409-019-0610-5
- Piemontese S, Ciceri F, Labopin M, Arcese W, Kyrcz-Krzemien S, Santarone S, et al. A comparison between allogeneic stem cell transplantation from unmanipulated haploidentical and unrelated donors in acute leukemia. J Hematol Oncol. 2017; 10(1):1-8.
doi: 10.1186/s13045-017-0394-2 - Sun Y, Beohou E, Labopin M, Volin L, Milpied N, Yakoub-Agha I, et al. Unmanipulated haploidentical versus matched unrelated donor allogeneic stem cell transplantation in adult patients with acute myelogenous leukemia in first remission: a retrospective pair-matched comparative study of the Beijing approach with the EBMT database. Haematologica. 2016; 101:e352-4.
doi: 10.3324/haematol.2015.140509 - Lorentino F, Labopin M, Bernardi M, Ciceri F, Socié G, Cornelissen JJ, et al. Comparable outcomes of haploidentical, 10/10 and 9/10unrelated donor transplantation in adverse karyotype AML in first complete remission. Am J Hematol. 2018; 93:1236-1244.
doi: 10.1002/ajh.25231 - Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant. 2014; 20(10):1573-1579.
doi: 10.1016/j.bbmt.2014.05.029 - Bashey A, Zhang XU, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013; 31(10):1310-1316.
doi: 10.1200/JCO.2012.44.3523 - Di Stasi A, Milton DR, Poon LM, Hamdi A, Rondon G, Chen J, et al. Similar transplantation outcomes for acute myeloid leukemia and myelodysplastic syndrome patients with haploidentical versus 10/10 human leukocyte antigen-matched unrelated and related donors. Biol Blood Marrow Transplant. 2014; 20(12):1975-1981. doi: 10.1016/j.bbmt.2014.08.013
- Luo Y, Xiao H, Lai X, Shi J, Tan Y, He J, et al. T-cell-replete haploidentical HSCT with low-dose anti-T-lymphocyte globulin compared with matched sibling HSCT and unrelated HSCT. Blood. 2014; 124(17):2735-2743. doi: 10.1182/blood-2014-04-571570
- Saglio F, Berger M, Spadea M, Pessolano R, Carraro F, Barone M, et al. Haploidentical HSCT with post transplantation cyclophosphamide versus unrelated donor HSCT in pediatric patients affected by acute leukemia. Bone Marrow Transpl. 2021; 56(3): 586-595. doi: 10.1038/s41409-020-01063-2
- Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Gress RE, Kanakry CG. Posttransplantation cyclophosphamide prevents graft-versus-host disease by inducing alloreactive T cell dysfunction and suppression. J Clin Invest. 2019; 129:2357–2373.
doi: 10.1172/JCI124218 - Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR, et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol. 2009; 10(9): 855-864. doi: 10.1016/S1470-2045(09)70225-6
- Bacigalupo A, Lamparelli T, Bruzzi P, Guidi S, Alessandrino PE, Di Bartolomeo P, et al. Antithymocyte globulin for graft-versus-host disease prophylaxis in transplants from unrelated donors: 2 randomized studies from Gruppo Italiano Trapianti Midollo Osseo (GITMO). Blood. 2001; 98(10):2942-2947. doi: 10.1182/blood.V98.10.2942
- Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011; 29(16):2230. doi: 10.1200/JCO.2010.33.7212
- Martin PJ, Counts Jr GW, Appelbaum FR, Lee SJ, Sanders JE, Deeg HJ, et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. J Clin Oncol. 2010; 28(6):1011. doi: 10.1200/JCO.2009.25.6693
- Arai S, Arora M, Wang T, Spellman SR, He W, Couriel DR, et al. Increasing incidence of chronic graft-versus-host disease in allogeneic transplantation: a report from the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2015; 21(2):266-274. doi: 10.1016/j.bbmt.2014.10.021
- Shimoni A, Labopin M, Finke J, Ciceri F, Deconinck E, Kröger N, et al. Donor selection for a second allogeneic stem cell transplantation in AML patients relapsing after a first transplant: a study of the Acute Leukemia Working Party of EBMT. Blood Cancer Journal. 2019 ; 9(12):1-9. doi: 10.1038/s41408-019-0251-3
- Distler E, Bloetz A, Albrecht J, Asdufan S, Hohberger A, Frey M, et al. Alloreactive and leukemia-reactive T cells are preferentially derived from naive precursors in healthy donors: implications for immunotherapy with memory T cells. Haematologica. 2011; 96(7):1024. doi: 10.3324/haematol.2010.037481
- Bertaina A, Zecca M, Buldini B, Sacchi N, Algeri M, Saglio F, et al. Unrelated donor vs HLA-haploidentical α/β T-cell- and Bcell-depleted HSCT in children with acute leukemia. Blood. 2018; 132:2594-2607. doi: 10.1182/blood-2018-07-861575
- Versluis J, Labopin M, Ruggeri A, Socie G, Wu D, Volin L, et al. Alternative donors for allogeneic hematopoietic stem cell transplantation in poor-risk AML in CR1. Blood Adv. 2017; 1(7):477-485. doi: 10.1182/bloodadvances.2016002386
- Baron F, Labopin M, Ruggeri A, Cornelissen JJ, Meijer E, Sengeloev H, et al. Impact of donor type in patients with AML given allogeneic hematopoietic cell transplantation after low-dose TBI-based regimen. Clin Cancer Res. 2018; 24(12):2794-2803.
doi: 10.1158/1078-0432.CCR-17-3622 - Rashidi A, Hamadani M, Zhang MJ, Wang HL, Abdel-Azim H, Aljurf M, et al. Outcomes of haploidentical vs matched sibling transplantation for acute myeloid leukemia in first complete remission. Blood Adv. 2019; 3(12):1826-1836.
https://doi.org/10.1182/bloodadvances.2019000050
" ["~DETAIL_TEXT"]=> string(40906) "
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is the only available curative option for acute leukemia nowadays. Many different parameters have significant impact on the final results of HSCT, especially on the more recently defined graft-versus-host disease (GvHD)-free/relapse-free survival (GFRFS) rate, including the pre-HSCT characteristics, such as disease profile at diagnosis and the disease status at the time of transplant, as well as the peri-HSCT factors, i.e. donor type, stem cell source, implemented conditioning regimen and potential post-transplant complications. Aiming to reduce the relapse rates after HSCT, myeloablative conditioning (MAC) regimens at higher dose intensity using busulfan or total body irradiation (TBI) has shown promising results [1]. However, due to higher vulnerability of younger patients to adverse effects of therapeutic irradiation, MAC regimens without TBI are preferred [2, 3]. Moreover, in view of relative complexity for bone marrow collection procedure, along with potentially enhanced graft-versus-leukemia (GvL) effect, peripheral blood (PB) is the preferred source of stem cells for allogeneic HSCT ever more. On the other hand, the increasing number of transplants from human leukocyte antigen (HLA)-haploidentical donors in the patients with acute leukemia is performed due to the absence of suitable related or unrelated HLA-matched donors, thus raising the necessity of understanding, whether HSCT outcomes with this approach are similar to those of more common modes. Over last years, several reports have shown comparable outcomes between HSCT from haploidentical donors and historical HLA-matched related or unrelated donors [4-6]. Hence, additional reports regarding the comparison of different donor types could be a guide to the upcoming therapeutic strategies. To address this issue, we carried out a single-center study, using HSCT with radiation-free MAC regimen, in order to evaluate the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) performed from matched and mismatched related and unrelated donors compared with haploidentical donors in children, adolescents and young adults (CAYA) affected by acute leukemia.
Patients and methods
Patient characteristics
Our study included 180 patients who underwent first allogeneic HSCT for acute leukemia in the CAYA HSCT Department of the Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Tehran, Iran, between January 2014 and January 2021. All data were retrieved retrospectively from clinical records according to the policy approved by the Committee for Medical Ethics of Tehran University of Medical Sciences (TUMS) and after obtaining informed consent from the patients, or their legal guardians.
HSCT parameters
In all patients and their donors, high-resolution HLA molecular typing for HLA-A, -B, -C, -DRB1, and -DQB1 loci was performed. The first donor preference was a 10/10 HLA-matched related donor (MRD), or a 9/10 HLA-mismatched related donor (MMRD). In absence of related donors, an alternative donor including 10/10 HLA-matched unrelated donors (MUD), or 9/10 HLA-mismatched unrelated donors (MMUD), or a related haploidentical donor (Haplo) was chosen, depending on their availability and accessibility.
We proceeded to HSCT if the result of a pre-HSCT bone marrow examination pointed to morphologically complete remission (CR), regardless of the minimal residual disease status. The HSCT procedure was based on irradiation-free MAC regimen including busulfan (a total dose of 3.2-4.8 mg/kg/day, according to patients' ideal body weight, from day -6 to -3), and cyclophosphamide (60 mg/kg/day, day -2 to -1). The GvHD prophylaxis was based on administration of cyclosporine A (CsA) in all the patients, and a short course of methotrexate (10 mg/m2 on day +1, 6 mg/m2 on day +3, +6, and +11) in HSCT from matched and mismatched related and unrelated donors, plus rabbit anti-human thymocytes globulins (ATG-Thymoglobuline, Sanofi, 2.5 mg/kg/day from days -3 to -1) in MMRD, MUD/MMUD and haplo-HSCT groups, and high-dose Pt-Cy treatment (40 mg/kg/day on days +3 and +4) in the Haplo group. We only included patients who received unmanipulated peripheral blood hematopoietic stem cells as graft source.
Considering hazards of CMV reactivation after HSCT, the patients were classified, according to their serological status, into low-risk (donor [D]-/recipient [R]-), intermediate-risk (D+/R-), or high-risk groups (D-/R+ or D+/R+) [7].
Definitions and endpoints
The main purpose of this study was to compare the survival rates of acute leukemia patients who had undergone allogeneic HSCT from different donor types. Overall survival (OS) was defined as the probability of survival, irrespective of the disease state at any point in time. GvHD-free/relapse-free survival (GFRFS) which is regarded as an endpoint more precisely reflective of health status and quality of life post-transplant, was defined as the probability of survival at complete remission of the disease, with sustained donor cell engraftment and absence of either grade III–IV acute GvHD, or chronic GvHD requiring immunosuppressive treatment [8]. Non-relapse mortality (NRM) was defined as probability of death without a relapse after HSCT. The relapse incidence (RI) was defined as the probability to develop a disease relapse.
Donor chimerism was determined on day +15, +30, +60 and +90 after HSCT, and then, if clinically indicated, in whole bone marrow mononuclear cells by means of quantitative PCR of informative short tandem repeats in the donor and recipient [9]. Sustained donor cell engraftment was defined at >0.5×109/L neutrophils and >20×109/L platelets for three consecutive days without blood transfusion support. Graft rejection was defined as a lack of initial engraftment of donor cells (primary), or loss of donor cell engraftment (secondary graft failure), regardless of peripheral cell blood counts. Acute GvHD (aGvHD) and chronic GvHD (cGvHD) were diagnosed and graded according to the published criteria [10, 11]. The mentioned HSCT outcomes were compared between the three categorized groups of different donor types, i.e., the patients transplanted from HLA-matched related (10/10), HLA-mismatched related (9/10) donors (MRD/MMRD), HLA-matched unrelated (10/10), HLA-mismatched (9/10) unrelated donors (MUD/MMUD), and HLA-haploidentical (Haplo) donors.
Statistical evaluation
The patients followed-up beyond 36 months were censored, for better comparison between the groups because some sub-groups had shorter follow-up periods than the other sub-groups. Homogeneity within treatment pairs was evaluated using the Chi-square test or Fisher exact test for qualitative variables and Student's T-test, or Wilcoxon rank-sum test for continuous variables. The endpoints were as follows: OS, GFRFS, relapse-associated, and non-relapse mortality incidence. Kaplan-Meier curves were derived to determine OS and GFRFS, having been compared with log-rank test.
Median follow-up time was established by means of reverse Kaplan-Meier method. After selection of baseline characteristics and clinical variables based on univariable Cox proportional hazards models, multivariable Cox proportional hazards models were fitted.
Variables in the multivariable OS and GFRFS were determined, as based on the P-values of <0.2 in the univariable Cox proportional hazards models. The proportionality of hazards assumption was checked using the global proportionality of hazard test based on Schoenfeld residuals in each of the three multivariable models. There were no deviations from the proportionality of hazards assumption in all multivariable models (results not shown). To account for informative censoring in presence of multiple endpoints, the competing risks in survival analysis were evaluated with nonparametric methods using the cumulative incidence competing risk method. CI for relapses and NRM were calculated by Gray's method. Death beyond relapses was considered a competing event for relapse, and the relapse was considered a competing event for NRM. The Fine-Gray proportional hazard regression model was used to assess the effects of covariates on the relapse frequency and NRM incidence. Like multivariate Cox proportional hazard regression, all the variables at P values of <0.2 in the univariate Fine-Gray proportional hazard regression were included in appropriate multivariate analyses. A two-sided P-value of <0.05 was considered to be statistically significant. The data evaluation was done with STATA version 16 and the packages "survival" and "cmprsk" in R software version 3.3.1.
Results
Patients
The study included 180 patients (120 males and 60 females) at a median age of 12 years (4 months to 24 years) at the time of HSCT, and 123 patients (68.3%) were transplanted at the age of ≤15 years. The donor types were as follows: matched (n=103) and mismatched (n=2) relatives including siblings (n=94) and other relatives (n=11) for a total of 105 cases (58.3%); matched (n=20) and mismatched (n=10) unrelated donors (a total of 30 patients, 16.7%), and haploidentical donors for 45 patients (25%). The patients’ characteristics are summarized in Table 1.
Table 1. Characteristics of the patients and transplant procedure

Notes: ALL: acute lymphoblastic leukemia, AML: acute myeloblastic leukemia, BM: bone marrow, BM+: involvement of bone marrow together with other sites, CR: complete remission, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUD/MMUD: HLA-matched unrelated and HLA-mismatched unrelated donors, R/D: recipient/donor, WBC: white blood cell.
The median follow-up time was 28.7 months for the patients enrolled into the study who were still alive at the end of the study (range: 21.9-34.9). A total of 96 patients presented with B-cell lineage acute lymphoblastic leukemia (ALL); 22 cases, with T-lineage ALL, and 62 patients had acute myeloblastic leukemia (AML). A total of 12 patients suffered from Ph chromosome-positive ALL. All the patients were in complete hematological remission before HSCT, including 93 patients (51.7%) transplanted in their first complete remission (CR1), 67 patients (37.2%) in the second complete remission (CR2), and 20 patients (11.1%) had experienced more than 2 relapses before HSCT. A pre-HSCT cytomegalovirus (CMV) serology showed that more than 90% of the patients were at high risk (recipient [R]+, donor [D]+) for CMV reactivation after HSCT.
Donor cell engraftment
All the patients (180/180) achieved neutrophil counts over 0.5×109/L at a median time of 11 days (range: 7-16). A total of 178 patients achieved platelet counts above 20×109/L, with a median time of 11 days (range: 0-130), and 4 patients died before the platelet engraftment (Table 2). The median time for neutrophil and platelet engraftment in Haplo vs MUD/MMUD vs MRD/MMRD was 12.20 and 14.67 days vs 12.17 and 16.21 days vs 10.73 and 14.30 days, respectively. Two patients from the Haplo group experienced secondary graft failure following CMV reactivation with high viral load after HSCT; one patient was successfully rescued by the second haploidentical HSCT from the same sibling donor, whereas other patient received a second allograft from other parent followed by sustained engraftment and hematopoietic recovery.
Table 2. Engraftment terms and GVHD incidence for the different donor types
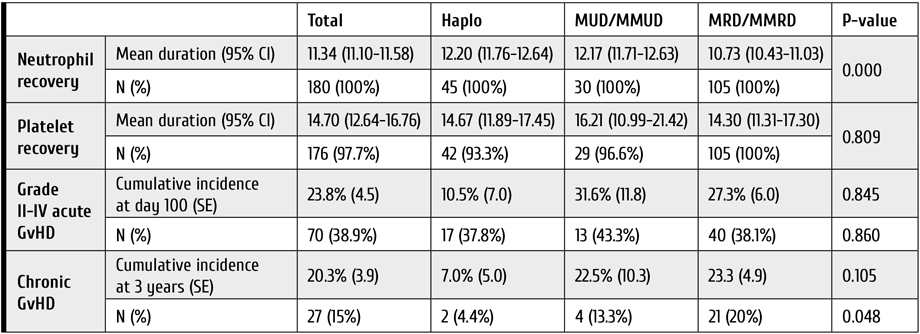
Notes: GvHD: graft-versus-host disease, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUD/MMUD: HLA-matched unrelated and HLA-mismatched unrelated donors.
Acute and chronic GVHD
Grade II to IV of aGvHD was diagnosed in 70 patients (38.9%), being developed at the median term of 15 days after HSCT. Cumulative aGVHD incidence at day 100 was highest in the MUD/MMUD group compared to Haplo and MRD/MMRD, but this difference was not statistically significant [31.6% (±11.8) versus 10.5% (±7.0) versus 27.3% (±6.0), respectively (P=0.845)].
Among 165 patients who survived more than 100 days after HSCT, 27 patients (15%) developed cGvHD, and we observed lower incidence of 3-year cGVHD in the haploidentical group compared to the MUD/MMUD group [7.0% (±5.0) versus 22.5% (±10.3), respectively]. Table 2 represents the comparison for GvHD incidence in the 3 donor types.
Relapse incidence (RI)
The 1-year and 3-year RI of the entire study population was 20.47% (95% CI 14.66-26.97) and 33.85% (95% CI 25.81-41.98), respectively. The 3-year RI in patients of the Haplo group was higher when compared to MUD/MMUD and MRD/MMRD: 40.95% (95% CI 18.41-62.44) versus 32.94% (95% CI 11.92-56.01) versus 33.17% (95% CI 23.64-42.99), respectively (Table 3). This difference was not statistically significant (P=0.902). In the Cox analysis, using both univariate and multivariate approaches, RI was not significantly different among the three donor type groups. In adjusted multivariable RI modeling, the hazard of relapse in the patients from MUD/MMUD group was only 10% lower than for the patients from Haplo group [HR=0.90 (95% CI 0.37-2.19), P=0.826].
Table 3. One- and three-year relapse incidence (RI) and non-relapse mortality (NRM) following HSCT
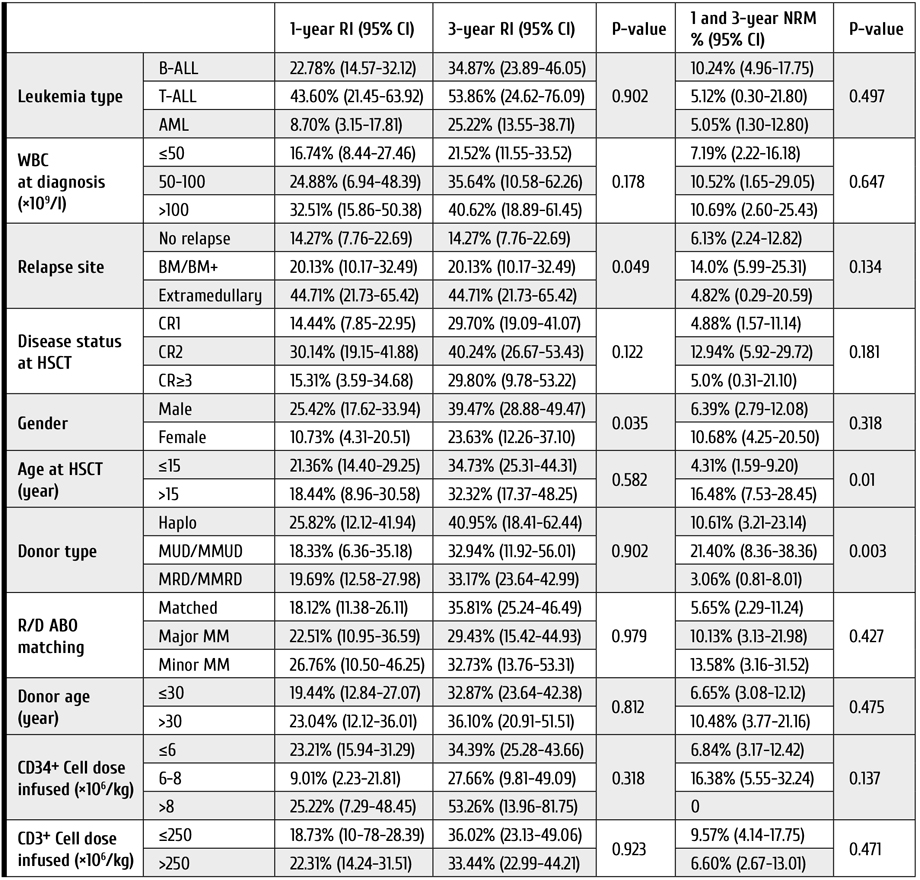
Notes: ALL: acute lymphoblastic leukemia, AML: acute myeloblastic leukemia, BM: bone marrow, BM+: involvement of bone marrow together with other sites, CR: complete remission, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUDMMUD: HLA-matched unrelated and HLA-mismatched unrelated donors, NRM: non-relapse mortality, R/D: recipient/donor, RI: relapse incidence, WBC: white blood cell.
Survival rates and post-HSCT complications
The 3-year OS and GFRFS rates for the entire study cohort were 68.81% (95% CI 60.08-76.01), and 44.19% (95% CI 35.52-54.49), respectively (Fig. 1). Patients in the MUD/MMUD group had the lowest OS and GFRFS compared to other donor types (Table 4).

Figure 1. Clinical outcomes in the cohort of young patients subjected to HSCT from different types of donors. A. Overall survival, B. GvHD-free, relapse-free survival, C. Relapse incidence, D. Non-relapse mortality of patients included in the study. Abscissa, observation terms
Note: Haplo: HLA-haploidentical donors, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUDMMUD: HLA-matched unrelated and HLA-mismatched unrelated donors.
Table 4. One- and three-year overall survival (OS) and GFRFS rates following HSCT in young patients
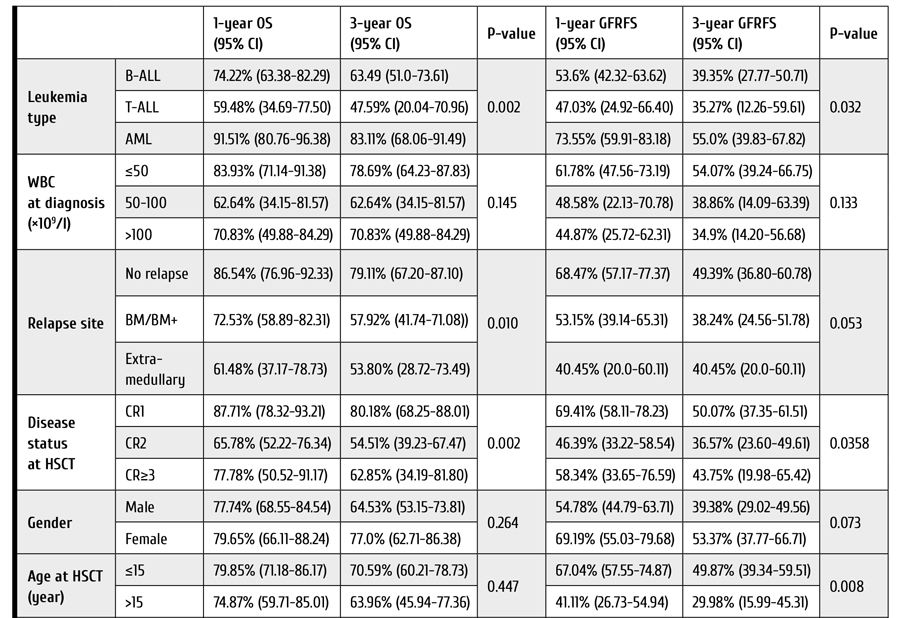

Notes: ALL: acute lymphoblastic leukemia, AML: acute myeloblastic leukemia, BM: bone marrow, BM+: involvement of bone marrow together with other sites, CR: complete remission, GFRFS: GvHD-free/relapse-free survival, Haplo: HLA-haploidentical donors, MM: mismatched, MRD/MMRD: HLA-matched related and HLA-mismatched related donors, MUD/MMUD: HLA-matched unrelated and HLA-mismatched.
The 3-year OS rates were 73.58% (95% CI 62.98-81.59), 54.21% (95% CI 29.61-73.49), and 64.18% (95% CI 39.76-80.79) for MRD/MMRD, MUD/MMUD, and Haplo groups, respectively (P=0.08); The 3-year GFRFS rates were 47.11% (95% CI 36.48-57.02), 30.89% (95% CI 10.70-53.80), and 42.46% (95% CI 20.41-63.01) for MRD/MMRD, MUD/MMUD, and Haplo groups, respectively (P=0.26). In the Cox analysis, using both univariate and multivariate approaches, OS and GFRFS were not significantly different among the 3 donor type groups. Adjusted multivariable modeling of OS based on the variables selected in unadjusted univariate models (see Patients and methods) showed that hazard of death in the patients who received HSCT from MUD/MMUD was about 3.6 times higher than in cases of HSCT from haploidentical donors, and this difference was statistically significant (P=0.05). Moreover, in those patients who received HSCT from MRD/MMRD, the hazard of death was 12 percent higher than for those who received HSCT from haploidentical donors [HR=1.12, (95% CI 0.34-3.67), P=0.84].
The 3-year NRM in all patients was 7.84% (95% CI 4.36-12.62). The patients who underwent MUD/MMUD HSCT showed significantly higher NRM compared to the patients who received Haplo and MRD/MMRD transplants (Table 3): 21.40% (95% CI 8.36-38.36) versus 10.61% (95% CI 3.21-23.14) versus 3.06% (95% CI 0.81-8.01), respectively (P=0.003).
Considering the causes of NRM among patients from MUD/MMUD group who died in the disease remission, we observed six cases of infection and one case of heart failure. In the Haplo group, one patient deceased from NRM had aGvHD, and four others developed infection. In the MRD/MMRD group, one patient was lost due to aGvHD, three patients died with infectious complications, and one case, due to unknown reason.
Adjusted multivariable modeling of NRM showed that hazard of death in the patients who received HSCT from MUD/MMUD was 6 times higher than the hazard of death for the patients who received HSCT from haploidentical donors. This difference was statistically significant (P=0.002). In those patients who received HSCT from MRD/MMRD, the hazard of death was not higher than in those who received HSCT from haploidentical donors (P=0.23).
Although the estimated risk of CMV reactivation prior to HSCT was high in most patients, CMV reactivation after HSCT was detected in a total of 61 cases (33.9%). CMV reactivation after HSCT occurred significantly more often in Haplo and MUD/MMUD group compared with the MRD/MMRD group (55.6% and 43.3% versus 21.9%, respectively, P=0.001). Worth of note, the CMV reactivation post-HSCT was associated with decreased OS and GFRFS in all three groups, being, however, statistically non-significant (P=0.09).
Hemorrhagic cystitis (HC) was another documented complication post-HSCT which occurred in 36 patients (20%), and it mostly affected the patients from Haplo and MUD/MMUD groups compared with MRD/MMRD group (35.6% and 33.3% versus 9.5%, respectively, P=0.000). Sinusoidal obstruction syndrome (SOS) was documented in only 5 patients, i.e. one case from Haplo group, two patients transplanted with MUD/MMUD grafts, and two, from the MRD/MMRD group.
Discussion
Allogeneic HSCT has augmented the potential of cure in patients with acute leukemia [12-15]. Although HLA-compatible related and unrelated donors have been traditionally used for treating acute leukemia patients requiring an allograft, there remains a significant proportion of patients for whom HLA-identical acceptable donor is not available. For these patients, the use of a haploidentical donor combined with alloreactive T cell elimination by Pt-Cy is the most widely adopted strategy [16]. Our study has shown that, for children, adolescents and young adults (CAYA) affected by acute leukemia, haploidentical HSCT followed by Pt-Cy may offer a better and more accessible chance of cure in terms of NRM and survival rates when compared with HSCT from unrelated donors who are hardly available, especially in the COVID-19 pandemic era.
Different studies reported that haploidentical HSCT could provide similar results to those of MUD and MMUD [17-19]. Several reports have shown, at least, comparable outcomes between Haplo and historical MRD, MUD, and MMUD series [20-23]. In our work, in consistence with most studies, the MRD/MMRD group had the best survival rates within the three donor types. Nevertheless, surprisingly, the survival rates were higher in the Haplo group compared to MUD/MMUD group.
Saglio et al., using a TBI-based conditioning regimen, have reported similar OS rates for Haplo and MUD/MMUD in CAYA patients [24]. In our study, OS rates were much higher in Haplo group compared to the MUD/MMUD group. Likewise, in our patients who had undergone haploidentical HSCT, GFRFS was higher and NRM was much lower than the results attained after HSCT from MUD/MMUD.
In terms of GvHD, it has been emphasized that Pt-Cy is able to significantly eliminate alloreactive T cells and, therefore, to reduce the incidence of GvHD, especially its acute form [25]. In addition, ATG has been shown to reduce the rates of severe acute and chronic GvHD in cases of matched or mismatched, unrelated allogeneic HSCT [26, 27]. Chronic GvHD is the leading cause of late complications and death after allogeneic HSCT. Usage of peripheral blood stem cells as a graft source presents a sufficient risk factor for its development, since the T-cell levels in allografts are higher than those in bone marrow [28-30]. Low incidence of GvHD, particularly chronic GvHD, in our patients, as compared to other reports in the literature, despite application of MAC regimen, along with usage of peripheral blood stem cells, could be attributed to high doses of ATG in the conditioning regimen for HSCT in the patients undergoing Haplo and MUD/MMUD HSCT. In our study, the rates of acute and chronic GvHD were even lower in the Haplo group than among the patients in MUD/MMUD group. This could be ascribed to dual in vivo T-cell depletion caused by ATG and Pt-Cy in the Haplo group. However, adoption of the highly effective GvHD prophylaxis may potentially lead to increased risk of relapse. It seems to be true in our study, as we had the highest relapse incidence (RI) in the Haplo group. However, one should note that the difference in RI among our three donor types was not statistically significant. It is presumed that HLA disparity could be considered a contributing factor to allo-reactivity and GvL [31]. In the matched donor transplant setting, the frequency of donor T-cell precursors directed against leukemia-specific antigens mediating GvL may be more limited [32]. Other studies with less rigorous GvHD prophylaxis strategies compared to our approaches, have reported similar RI in Haplo and MUD/MMUD HSCT [24, 34].
With respect to transplant toxicity, our data confirm that the patients undergoing Haplo HSCT have much lower NRM rates compared to patients undergoing MUD/MMUD HSCT, and the rates of complications, such as hemorrhagic cystitis and sinusoidal obstruction syndrome, seem to be comparable within the two groups. Previous studies comparing NRM rates in Haplo (with Pt-Cy) with MRD and MUD transplants (with standard GvHD prophylaxis) have reported inconsistent results. Meanwhile, some studies reported a higher NRM rates in Haplo HSCT [17, 35, 36].
This study was limited by its retrospective design, inability to adjust for unknown factors, the heterogeneity for conditioning regimens and supportive therapy that could affect the study outcomes.
Conclusions
Our study shows that inclusion of ATG into the myeloablative conditioning regimen before transplantation of peripheral blood stem cells from MUD/MMUD and Haplo donors is associated with reduced rates of chronic GvHD and graft failure, concomitantly. The rates of OS and GFRFS were higher in the Haplo group compared to MUD/MMUD, hence, our data supports the view that haploidentical HSCT with peripheral blood stem cells is a practical and valuable clinical option that offers CAYA patients with acute leukemia requiring HSCT and lacking matched available donors, a reasonable opportunity for the disease control. However, further progress is necessary to decrease the relapse rate in these patients.
Declarations
The study was approved by the Committee on Medical Ethics of Tehran University of Medical Sciences (TUMS) and informed consent was obtained from patients or their legal guardians. Authors provide a consent for publication. Primary data and materials are available on request.
Authors' contributions: TR designed and coordinated the study, and managed the patients. AK, MR and NA participated in the management of patients. AK carried out statistical evaluation. SA conceived of the study. All the authors read and approved the final manuscript.
Acknowledgements
We would like to thank Ashraf Sadat Hoseini and other nursing staff for their undeniable assistance in care for our patients.
Competing Interests
None of the authors have any relevant conflict of interest to disclaim about the present article. No funding support for the study is declared.
References
- Solomon SR, Sizemore CA, Sanacore M, Zhang X, Brown S, Holland HK, et al. Total body irradiation-based myeloablative haploidentical stem cell transplantation is a safe and effective alternative to unrelated donor transplantation in patients without matched sibling donors. Biol Blood Marrow Transplant. 2015; 21(7):1299-1307. doi: 10.1016/j.bbmt.2015.03.003
- Friebert SE, Shepardson LB, Shurin SB, Rosenthal GE, Rosenthal NS. Pediatric bone marrow cellularity: are we expecting too much?
J Pediat Hematol/Oncol. 1998; 20(5):439-43. doi: 10.1097/00043426-199809000-00006 - Muschler GF, Nitto H, Boehm CA, Easley KA. Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors. J Orthop Res. 2001; 19(1):117-125. doi: 10.1016/S0736-0266(00)00010-3
- Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant. 2014; 20(10):1573-1579.
doi: 10.1016/j.bbmt.2014.05.029 - Bashey A, Zhang XU, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013; 31(10):1310-1316. doi: 10.1200/JCO.2012.44.3523
- Di Stasi A, Milton DR, Poon LM, Hamdi A, Rondon G, Chen J, et al. Similar transplantation outcomes for acute myeloid leukemia and myelodysplastic syndrome patients with haploidentical versus 10/10 human leukocyte antigen-matched unrelated and related donors. Biol Blood Marrow Transplant. 2014; 20(12):1975-1981. doi: 10.1016/j.bbmt.2014.08.013
- George B, Pati N, Gilroy N, Ratnamohan M, Huang G, Kerridge I, Hertzberg M, Gottlieb D, Bradstock K. Pre-transplant cytomegalovirus (CMV) serostatus remains the most important determinant of CMV reactivation after allogeneic hematopoietic stem cell transplantation in the era of surveillance and preemptive therapy. Transplant Infect Dis. 2010; 12(4):322-9.
doi: 10.1111/j.1399-3062.2010.00504.x - Balavarca Y, Pearce K, Norden J, Collin M, Jackson G, Holler E, et al. Predicting survival using clinical risk scores and non-HLA immunogenetics. Bone Marrow Transpl. 2015; 50(11):1445-1452. doi: 10.1038/bmt.2015.305
- Thiede C, Florek M, Bornhäuser M, Ritter M, Mohr B, Brendel C, et al. Rapid quantification of mixed chimerism using multiplex amplification of short tandem repeat markers and fluorescence detection. Bone Marrow Transpl. 1999; 23:1055-1060.
doi: 10.1038/sj.bmt.1701779 - Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the disease risk index for allogeneic stem cell transplantation. Blood. 2014; 123:3664-3671. doi: 10.1182/blood-2014-01-552984
- Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974; 18:295-304.
- Afify Z, Hunt L, Green A, Guttridge M, Cornish J, Oakhill A. Factors affecting the outcome of stem cell transplantation from unrelated donors for childhood acute lymphoblastic leukemia in third remission. Bone Marrow Transpl. 2005; 35:1041-1047.
doi: 10.1038/sj.bmt.1704958 - Balduzzi A, Valsecchi MG, Uderzo C, De Lorenzo P, Klingebiel T, Peters C, et al. Chemotherapy versus allogeneic transplantation for very-high-risk childhood acute lymphoblastic leukaemia in first complete remission: comparison by genetic randomisation in an international prospective study. Lancet. 2005; 366:635-642. doi: 10.1016/S0140-6736(05)66998-X
- Cornish J, Oakhill A. The management of relapsed acute lymphoblastic leukaemia. Bone Marrow Transpl. 2001; 28(1):S9. https://doi.org/10.1038/sj.bmt.1703167
- Klingebiel T, Cornish J, Labopin M, Locatelli F, Darbyshire P, Handgretinger R, et al. Results and factors influencing outcome after fully haploidentical hematopoietic stem cell transplantation in children with very high-risk acute lymphoblastic leukemia: impact of center size: an analysis on behalf of the Acute Leukemia and Pediatric Disease Working Parties of the European Blood and Marrow Transplant group. Blood. 2010; 115:3437-3446. doi: 10.1182/blood-2009-03-207001
- Nagler A, Ruggeri A. Haploidentical stem cell transplantation (HaploSCT) for patients with acute leukemia – an update on behalf of the ALWP of the EBMT. Bone Marrow Transplant. 2019; 54(2): 713-718. doi: 10.1038/s41409-019-0610-5
- Piemontese S, Ciceri F, Labopin M, Arcese W, Kyrcz-Krzemien S, Santarone S, et al. A comparison between allogeneic stem cell transplantation from unmanipulated haploidentical and unrelated donors in acute leukemia. J Hematol Oncol. 2017; 10(1):1-8.
doi: 10.1186/s13045-017-0394-2 - Sun Y, Beohou E, Labopin M, Volin L, Milpied N, Yakoub-Agha I, et al. Unmanipulated haploidentical versus matched unrelated donor allogeneic stem cell transplantation in adult patients with acute myelogenous leukemia in first remission: a retrospective pair-matched comparative study of the Beijing approach with the EBMT database. Haematologica. 2016; 101:e352-4.
doi: 10.3324/haematol.2015.140509 - Lorentino F, Labopin M, Bernardi M, Ciceri F, Socié G, Cornelissen JJ, et al. Comparable outcomes of haploidentical, 10/10 and 9/10unrelated donor transplantation in adverse karyotype AML in first complete remission. Am J Hematol. 2018; 93:1236-1244.
doi: 10.1002/ajh.25231 - Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A, et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant. 2014; 20(10):1573-1579.
doi: 10.1016/j.bbmt.2014.05.029 - Bashey A, Zhang XU, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013; 31(10):1310-1316.
doi: 10.1200/JCO.2012.44.3523 - Di Stasi A, Milton DR, Poon LM, Hamdi A, Rondon G, Chen J, et al. Similar transplantation outcomes for acute myeloid leukemia and myelodysplastic syndrome patients with haploidentical versus 10/10 human leukocyte antigen-matched unrelated and related donors. Biol Blood Marrow Transplant. 2014; 20(12):1975-1981. doi: 10.1016/j.bbmt.2014.08.013
- Luo Y, Xiao H, Lai X, Shi J, Tan Y, He J, et al. T-cell-replete haploidentical HSCT with low-dose anti-T-lymphocyte globulin compared with matched sibling HSCT and unrelated HSCT. Blood. 2014; 124(17):2735-2743. doi: 10.1182/blood-2014-04-571570
- Saglio F, Berger M, Spadea M, Pessolano R, Carraro F, Barone M, et al. Haploidentical HSCT with post transplantation cyclophosphamide versus unrelated donor HSCT in pediatric patients affected by acute leukemia. Bone Marrow Transpl. 2021; 56(3): 586-595. doi: 10.1038/s41409-020-01063-2
- Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Gress RE, Kanakry CG. Posttransplantation cyclophosphamide prevents graft-versus-host disease by inducing alloreactive T cell dysfunction and suppression. J Clin Invest. 2019; 129:2357–2373.
doi: 10.1172/JCI124218 - Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR, et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol. 2009; 10(9): 855-864. doi: 10.1016/S1470-2045(09)70225-6
- Bacigalupo A, Lamparelli T, Bruzzi P, Guidi S, Alessandrino PE, Di Bartolomeo P, et al. Antithymocyte globulin for graft-versus-host disease prophylaxis in transplants from unrelated donors: 2 randomized studies from Gruppo Italiano Trapianti Midollo Osseo (GITMO). Blood. 2001; 98(10):2942-2947. doi: 10.1182/blood.V98.10.2942
- Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011; 29(16):2230. doi: 10.1200/JCO.2010.33.7212
- Martin PJ, Counts Jr GW, Appelbaum FR, Lee SJ, Sanders JE, Deeg HJ, et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. J Clin Oncol. 2010; 28(6):1011. doi: 10.1200/JCO.2009.25.6693
- Arai S, Arora M, Wang T, Spellman SR, He W, Couriel DR, et al. Increasing incidence of chronic graft-versus-host disease in allogeneic transplantation: a report from the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2015; 21(2):266-274. doi: 10.1016/j.bbmt.2014.10.021
- Shimoni A, Labopin M, Finke J, Ciceri F, Deconinck E, Kröger N, et al. Donor selection for a second allogeneic stem cell transplantation in AML patients relapsing after a first transplant: a study of the Acute Leukemia Working Party of EBMT. Blood Cancer Journal. 2019 ; 9(12):1-9. doi: 10.1038/s41408-019-0251-3
- Distler E, Bloetz A, Albrecht J, Asdufan S, Hohberger A, Frey M, et al. Alloreactive and leukemia-reactive T cells are preferentially derived from naive precursors in healthy donors: implications for immunotherapy with memory T cells. Haematologica. 2011; 96(7):1024. doi: 10.3324/haematol.2010.037481
- Bertaina A, Zecca M, Buldini B, Sacchi N, Algeri M, Saglio F, et al. Unrelated donor vs HLA-haploidentical α/β T-cell- and Bcell-depleted HSCT in children with acute leukemia. Blood. 2018; 132:2594-2607. doi: 10.1182/blood-2018-07-861575
- Versluis J, Labopin M, Ruggeri A, Socie G, Wu D, Volin L, et al. Alternative donors for allogeneic hematopoietic stem cell transplantation in poor-risk AML in CR1. Blood Adv. 2017; 1(7):477-485. doi: 10.1182/bloodadvances.2016002386
- Baron F, Labopin M, Ruggeri A, Cornelissen JJ, Meijer E, Sengeloev H, et al. Impact of donor type in patients with AML given allogeneic hematopoietic cell transplantation after low-dose TBI-based regimen. Clin Cancer Res. 2018; 24(12):2794-2803.
doi: 10.1158/1078-0432.CCR-17-3622 - Rashidi A, Hamadani M, Zhang MJ, Wang HL, Abdel-Azim H, Aljurf M, et al. Outcomes of haploidentical vs matched sibling transplantation for acute myeloid leukemia in first complete remission. Blood Adv. 2019; 3(12):1826-1836.
https://doi.org/10.1182/bloodadvances.2019000050
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "20" ["~SORT"]=> string(2) "20" ["CODE"]=> string(101) "transplantatsiya-gemopoeticheskikh-kletok-perifericheskoy-krovi-ot-gaploidentichnykh-i-nerodstvennykh" ["~CODE"]=> string(101) "transplantatsiya-gemopoeticheskikh-kletok-perifericheskoy-krovi-ot-gaploidentichnykh-i-nerodstvennykh" ["EXTERNAL_ID"]=> string(4) "2052" ["~EXTERNAL_ID"]=> string(4) "2052" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(546) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного рискаPeripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(6200) "<p style="text-align: justify;">Трансплантация аллогенных гематопоэтических клеток (алло-ТГСК) является единственной потенциальной возможностью излечения острого лейкоза. Многие параметры существенно влияют на конечный исход ТГСК, в т.ч. тип донора, источник стволовых клеток и применяемый режим кондиционирования. При отсутствии HLA-совместимого родственного донора, возможными кандидатами могут быть неродственные совместимые или гаплоидентичные доноры для пациентов с показаниями к ТГСК. Для того, чтобы сопоставить исходы ТГСК от доноров различного типа с кондиционированием без облучения, мы сравнили в рамках одноцентрового исследования результаты трансплантации интактных ГСК периферической крови от совместимых и несовместимых, родственных и неродственных доноров, и гаплоидентичных доноров реципиентам детского, подросткового возрастов и молодым взрослым с острыми лейкозами.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">В данном ретроспективном исследовании, проводившемся с 2014 по 2021 г., мы оценивали исходы ТГСК с реплецией Т-лимфоцитов от гаплоидентичных доноров или неродственных доноров (совместимость – 10/10 или 9/10), а также в сравнении с неродственными донорами у пациентов с острыми лейкозами этих возрастных групп. Кондиционирование при ТГСК проводили с применением миелоаблативного режима с бусульфаном и циклофосфамидом и без ионизирующего облучения. Профилактика РТПХ включала назначение циклоспорина А всем пациентам, кроличий антитимоцитарный глобулин для неродственных и гаплоидентичных доноров, и циклофосфамид при ТГСК от гаплоидентичных доноров. Статистическую обработку проводили с помощью многовариантного пропорционального анализа рисков по Коксу и анализ конкурирующих рисков.</p> <h3>Результаты</h3> <p style="text-align: justify;">Средний срок наблюдения составлял 28,7 мес. (95% CI: 21,9-34,9). Трехлетняя общая выживаемость (ОВ) и выживаемости без РТПХ и рецидивов были, соответственно, 68,81% (95% CI: 60,08%-76,01%) и 44.19% (95% CI: 35,52%-52,49%). Пациенты после ТГСК от неродственных совместимых доноров имели более низкие уровни ОВ и выживаемости без РТПХ и рецидивов по сравнению с другими типами доноров. Трехлетние показатели безрецидивной летальности (NRM) среди всех пациентов составляли 7,84% (95% CI 4,36-12,62). Адаптированное многовариантное моделирование общей выживаемости показало, что риск гибели пациентов после ТГСК от неродственного донора был в 3,6 раза выше, чем у пациентов, получивших ТГСК от гаплоидентичных доноров (P=0.05). Аналогично, риск безрецидивной смертности (NRM) после ТГСК от неродственных доноров был в 6 раз выше, чем при ТГСК от гаплоидентичных доноров (P=0.002). Однако частота рецидивов не различалась существенно между двумя указанными группами.</p> <h3>Выводы</h3> <p style="text-align: justify;">В данном исследовании показано, что ТГСК от гаплоидентичных доноров была ассоциирована с более высокими уровнями выживаемости, по сравнению с ТГСК от неродственных совместимых доноров. Таким образом, ТГСК от гаплоидентичных доноров может быть предложена в качестве практичной и ценной клинической опции, для пациентов молодых возрастов с острыми лейкозами в случае отсутствия совместимых доноров.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Острый лейкоз, аллогенная трансплантация гемопоэтических клеток, совместимые родственные доноры, неродственные доноры, гаплоидентичные доноры, клинические исходы.</p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_META_TITLE"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_META_KEYWORDS"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_META_DESCRIPTION"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_PICTURE_FILE_ALT"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_PICTURE_FILE_TITLE"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_PICTURE_FILE_NAME"]=> string(101) "transplantatsiya-gemopoeticheskikh-kletok-perifericheskoy-krovi-ot-gaploidentichnykh-i-nerodstvennykh" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(353) "Трансплантация гемопоэтических клеток периферической крови от гаплоидентичных и неродственных доноров при острых лейкозах у детей, подростков и молодых взрослых: анализ конкурентного риска" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(101) "transplantatsiya-gemopoeticheskikh-kletok-perifericheskoy-krovi-ot-gaploidentichnykh-i-nerodstvennykh" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(101) "transplantatsiya-gemopoeticheskikh-kletok-perifericheskoy-krovi-ot-gaploidentichnykh-i-nerodstvennykh" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(101) "transplantatsiya-gemopoeticheskikh-kletok-perifericheskoy-krovi-ot-gaploidentichnykh-i-nerodstvennykh" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "207" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28530" ["VALUE"]=> string(22) "01/24/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/24/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28531" ["VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28532" ["VALUE"]=> array(2) { ["TEXT"]=> string(714) "<p>Тахерех Ростами<sup>1</sup>, Мохамад Р. Ростами<sup>2</sup>, Азадех Кьюмарси<sup>1</sup>, Амир Казаэйян<sup>3</sup>, Неда Алиджани<sup>4</sup>, Хосейн К. Фумани<sup>2</sup>, Соруш Рад<sup>2</sup>, Давуд Бабахани<sup>2</sup>, Таназ Бахри<sup>2</sup>, Мохаммад Ваези<sup>2</sup>, Мариам Бахордар<sup>2</sup>, Сейед А. Мирхоссейни<sup>2</sup>, Сейед А. Моусави<sup>2</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(546) "
Тахерех Ростами1, Мохамад Р. Ростами2, Азадех Кьюмарси1, Амир Казаэйян3, Неда Алиджани4, Хосейн К. Фумани2, Соруш Рад2, Давуд Бабахани2, Таназ Бахри2, Мохаммад Ваези2, Мариам Бахордар2, Сейед А. Мирхоссейни2, Сейед А. Моусави2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28533" ["VALUE"]=> array(2) { ["TEXT"]=> string(1215) "<p><sup>1</sup> Отдел клеточной терапии у детей, НИИ онкологии, гематологии и клеточной терапии (RIOHCT), Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br> <sup>2</sup> НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br> <sup>3</sup> Отдел биостатистики и эпидемиологии, НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br> <sup>4</sup> Отдел инфекционных болезней, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1137) "1 Отдел клеточной терапии у детей, НИИ онкологии, гематологии и клеточной терапии (RIOHCT), Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
2 НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
3 Отдел биостатистики и эпидемиологии, НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
4 Отдел инфекционных болезней, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
Трансплантация аллогенных гематопоэтических клеток (алло-ТГСК) является единственной потенциальной возможностью излечения острого лейкоза. Многие параметры существенно влияют на конечный исход ТГСК, в т.ч. тип донора, источник стволовых клеток и применяемый режим кондиционирования. При отсутствии HLA-совместимого родственного донора, возможными кандидатами могут быть неродственные совместимые или гаплоидентичные доноры для пациентов с показаниями к ТГСК. Для того, чтобы сопоставить исходы ТГСК от доноров различного типа с кондиционированием без облучения, мы сравнили в рамках одноцентрового исследования результаты трансплантации интактных ГСК периферической крови от совместимых и несовместимых, родственных и неродственных доноров, и гаплоидентичных доноров реципиентам детского, подросткового возрастов и молодым взрослым с острыми лейкозами.
Пациенты и методы
В данном ретроспективном исследовании, проводившемся с 2014 по 2021 г., мы оценивали исходы ТГСК с реплецией Т-лимфоцитов от гаплоидентичных доноров или неродственных доноров (совместимость – 10/10 или 9/10), а также в сравнении с неродственными донорами у пациентов с острыми лейкозами этих возрастных групп. Кондиционирование при ТГСК проводили с применением миелоаблативного режима с бусульфаном и циклофосфамидом и без ионизирующего облучения. Профилактика РТПХ включала назначение циклоспорина А всем пациентам, кроличий антитимоцитарный глобулин для неродственных и гаплоидентичных доноров, и циклофосфамид при ТГСК от гаплоидентичных доноров. Статистическую обработку проводили с помощью многовариантного пропорционального анализа рисков по Коксу и анализ конкурирующих рисков.
Результаты
Средний срок наблюдения составлял 28,7 мес. (95% CI: 21,9-34,9). Трехлетняя общая выживаемость (ОВ) и выживаемости без РТПХ и рецидивов были, соответственно, 68,81% (95% CI: 60,08%-76,01%) и 44.19% (95% CI: 35,52%-52,49%). Пациенты после ТГСК от неродственных совместимых доноров имели более низкие уровни ОВ и выживаемости без РТПХ и рецидивов по сравнению с другими типами доноров. Трехлетние показатели безрецидивной летальности (NRM) среди всех пациентов составляли 7,84% (95% CI 4,36-12,62). Адаптированное многовариантное моделирование общей выживаемости показало, что риск гибели пациентов после ТГСК от неродственного донора был в 3,6 раза выше, чем у пациентов, получивших ТГСК от гаплоидентичных доноров (P=0.05). Аналогично, риск безрецидивной смертности (NRM) после ТГСК от неродственных доноров был в 6 раз выше, чем при ТГСК от гаплоидентичных доноров (P=0.002). Однако частота рецидивов не различалась существенно между двумя указанными группами.
Выводы
В данном исследовании показано, что ТГСК от гаплоидентичных доноров была ассоциирована с более высокими уровнями выживаемости, по сравнению с ТГСК от неродственных совместимых доноров. Таким образом, ТГСК от гаплоидентичных доноров может быть предложена в качестве практичной и ценной клинической опции, для пациентов молодых возрастов с острыми лейкозами в случае отсутствия совместимых доноров.
Ключевые слова
Острый лейкоз, аллогенная трансплантация гемопоэтических клеток, совместимые родственные доноры, неродственные доноры, гаплоидентичные доноры, клинические исходы.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28535" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-24-35" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-24-35" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28538" ["VALUE"]=> array(2) { ["TEXT"]=> string(550) "<p>Tahereh Rostami<sup>1</sup>, Mohammad R. Rostami<sup>2</sup>, Azadeh Kiumarsi<sup>1</sup>, Amir Kasaeian<sup>3</sup>, Neda Alijani<sup>4</sup>, Hosein K. Fumani<sup>2</sup>, Soroush Rad<sup>2</sup>, Davood Babakhani<sup>2</sup>, Tanaz Bahri<sup>2</sup>, Mohammad Vaezi<sup>2</sup>, Maryam Barkhordar<sup>2</sup>, Seied A. Mirhosseini<sup>2</sup>, Seied A. Mousavi<sup>2</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(382) "Tahereh Rostami1, Mohammad R. Rostami2, Azadeh Kiumarsi1, Amir Kasaeian3, Neda Alijani4, Hosein K. Fumani2, Soroush Rad2, Davood Babakhani2, Tanaz Bahri2, Mohammad Vaezi2, Maryam Barkhordar2, Seied A. Mirhosseini2, Seied A. Mousavi2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28539" ["VALUE"]=> array(2) { ["TEXT"]=> string(1607) "<p><sup>1</sup> Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br> <sup>2</sup> Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br> <sup>3</sup> Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br> <sup>4</sup> Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran</p><br> <p><b>Correspondence:</b><br> Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran<br> Phone: +98 9121037104<br> Fax: +98 (21) 8802 9397<br> Email: akiumarsi@sina.tums.ac.ir</p><br> <p><b>Citation:</b> Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1445) "1 Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
2 Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3 Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati
Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
4 Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
Correspondence:
Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran
Phone: +98 9121037104
Fax: +98 (21) 8802 9397
Email: akiumarsi@sina.tums.ac.ir
Citation: Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28540" ["VALUE"]=> array(2) { ["TEXT"]=> string(3600) "<p style="text-align: justify;">Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.</p> <h3>Patients and methods</h3> <p style="text-align: justify;">In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors <i>versus</i> unrelated donors (including 10/10 or 9/10 HLA-matched), and <i>versus</i> related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.</p> <h3>Results</h3> <p style="text-align: justify;">Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.</p> <h3>Conclusions</h3> <p style="text-align: justify;">In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.</p> <h2>Keywords</h2> <p style="text-align: justify;">Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3418) "Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.
Patients and methods
In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors versus unrelated donors (including 10/10 or 9/10 HLA-matched), and versus related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.
Results
Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.
Conclusions
In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.
Keywords
Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28536" ["VALUE"]=> string(193) "Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(193) "Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28537" ["VALUE"]=> string(4) "2786" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2786" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28541" ["VALUE"]=> string(4) "2787" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2787" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(10) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28538" ["VALUE"]=> array(2) { ["TEXT"]=> string(550) "<p>Tahereh Rostami<sup>1</sup>, Mohammad R. Rostami<sup>2</sup>, Azadeh Kiumarsi<sup>1</sup>, Amir Kasaeian<sup>3</sup>, Neda Alijani<sup>4</sup>, Hosein K. Fumani<sup>2</sup>, Soroush Rad<sup>2</sup>, Davood Babakhani<sup>2</sup>, Tanaz Bahri<sup>2</sup>, Mohammad Vaezi<sup>2</sup>, Maryam Barkhordar<sup>2</sup>, Seied A. Mirhosseini<sup>2</sup>, Seied A. Mousavi<sup>2</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(382) "Tahereh Rostami1, Mohammad R. Rostami2, Azadeh Kiumarsi1, Amir Kasaeian3, Neda Alijani4, Hosein K. Fumani2, Soroush Rad2, Davood Babakhani2, Tanaz Bahri2, Mohammad Vaezi2, Maryam Barkhordar2, Seied A. Mirhosseini2, Seied A. Mousavi2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(382) "Tahereh Rostami1, Mohammad R. Rostami2, Azadeh Kiumarsi1, Amir Kasaeian3, Neda Alijani4, Hosein K. Fumani2, Soroush Rad2, Davood Babakhani2, Tanaz Bahri2, Mohammad Vaezi2, Maryam Barkhordar2, Seied A. Mirhosseini2, Seied A. Mousavi2
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28540" ["VALUE"]=> array(2) { ["TEXT"]=> string(3600) "<p style="text-align: justify;">Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.</p> <h3>Patients and methods</h3> <p style="text-align: justify;">In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors <i>versus</i> unrelated donors (including 10/10 or 9/10 HLA-matched), and <i>versus</i> related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.</p> <h3>Results</h3> <p style="text-align: justify;">Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.</p> <h3>Conclusions</h3> <p style="text-align: justify;">In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.</p> <h2>Keywords</h2> <p style="text-align: justify;">Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3418) "Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.
Patients and methods
In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors versus unrelated donors (including 10/10 or 9/10 HLA-matched), and versus related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.
Results
Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.
Conclusions
In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.
Keywords
Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(3418) "Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.
Patients and methods
In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors versus unrelated donors (including 10/10 or 9/10 HLA-matched), and versus related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.
Results
Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.
Conclusions
In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.
Keywords
Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28535" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-24-35" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-24-35" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-24-35" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28536" ["VALUE"]=> string(193) "Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(193) "Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(193) "Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28539" ["VALUE"]=> array(2) { ["TEXT"]=> string(1607) "<p><sup>1</sup> Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br> <sup>2</sup> Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br> <sup>3</sup> Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br> <sup>4</sup> Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran</p><br> <p><b>Correspondence:</b><br> Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran<br> Phone: +98 9121037104<br> Fax: +98 (21) 8802 9397<br> Email: akiumarsi@sina.tums.ac.ir</p><br> <p><b>Citation:</b> Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1445) "1 Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
2 Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3 Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati
Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
4 Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
Correspondence:
Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran
Phone: +98 9121037104
Fax: +98 (21) 8802 9397
Email: akiumarsi@sina.tums.ac.ir
Citation: Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(1445) "1 Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
2 Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3 Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati
Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
4 Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
Correspondence:
Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran
Phone: +98 9121037104
Fax: +98 (21) 8802 9397
Email: akiumarsi@sina.tums.ac.ir
Citation: Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35.
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28532" ["VALUE"]=> array(2) { ["TEXT"]=> string(714) "<p>Тахерех Ростами<sup>1</sup>, Мохамад Р. Ростами<sup>2</sup>, Азадех Кьюмарси<sup>1</sup>, Амир Казаэйян<sup>3</sup>, Неда Алиджани<sup>4</sup>, Хосейн К. Фумани<sup>2</sup>, Соруш Рад<sup>2</sup>, Давуд Бабахани<sup>2</sup>, Таназ Бахри<sup>2</sup>, Мохаммад Ваези<sup>2</sup>, Мариам Бахордар<sup>2</sup>, Сейед А. Мирхоссейни<sup>2</sup>, Сейед А. Моусави<sup>2</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(546) "Тахерех Ростами1, Мохамад Р. Ростами2, Азадех Кьюмарси1, Амир Казаэйян3, Неда Алиджани4, Хосейн К. Фумани2, Соруш Рад2, Давуд Бабахани2, Таназ Бахри2, Мохаммад Ваези2, Мариам Бахордар2, Сейед А. Мирхоссейни2, Сейед А. Моусави2
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(546) "Тахерех Ростами1, Мохамад Р. Ростами2, Азадех Кьюмарси1, Амир Казаэйян3, Неда Алиджани4, Хосейн К. Фумани2, Соруш Рад2, Давуд Бабахани2, Таназ Бахри2, Мохаммад Ваези2, Мариам Бахордар2, Сейед А. Мирхоссейни2, Сейед А. Моусави2
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28530" ["VALUE"]=> string(22) "01/24/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/24/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "01/24/2022 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28531" ["VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "02/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "02/18/2022 12:00:00 am" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28534" ["VALUE"]=> array(2) { ["TEXT"]=> string(6200) "<p style="text-align: justify;">Трансплантация аллогенных гематопоэтических клеток (алло-ТГСК) является единственной потенциальной возможностью излечения острого лейкоза. Многие параметры существенно влияют на конечный исход ТГСК, в т.ч. тип донора, источник стволовых клеток и применяемый режим кондиционирования. При отсутствии HLA-совместимого родственного донора, возможными кандидатами могут быть неродственные совместимые или гаплоидентичные доноры для пациентов с показаниями к ТГСК. Для того, чтобы сопоставить исходы ТГСК от доноров различного типа с кондиционированием без облучения, мы сравнили в рамках одноцентрового исследования результаты трансплантации интактных ГСК периферической крови от совместимых и несовместимых, родственных и неродственных доноров, и гаплоидентичных доноров реципиентам детского, подросткового возрастов и молодым взрослым с острыми лейкозами.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">В данном ретроспективном исследовании, проводившемся с 2014 по 2021 г., мы оценивали исходы ТГСК с реплецией Т-лимфоцитов от гаплоидентичных доноров или неродственных доноров (совместимость – 10/10 или 9/10), а также в сравнении с неродственными донорами у пациентов с острыми лейкозами этих возрастных групп. Кондиционирование при ТГСК проводили с применением миелоаблативного режима с бусульфаном и циклофосфамидом и без ионизирующего облучения. Профилактика РТПХ включала назначение циклоспорина А всем пациентам, кроличий антитимоцитарный глобулин для неродственных и гаплоидентичных доноров, и циклофосфамид при ТГСК от гаплоидентичных доноров. Статистическую обработку проводили с помощью многовариантного пропорционального анализа рисков по Коксу и анализ конкурирующих рисков.</p> <h3>Результаты</h3> <p style="text-align: justify;">Средний срок наблюдения составлял 28,7 мес. (95% CI: 21,9-34,9). Трехлетняя общая выживаемость (ОВ) и выживаемости без РТПХ и рецидивов были, соответственно, 68,81% (95% CI: 60,08%-76,01%) и 44.19% (95% CI: 35,52%-52,49%). Пациенты после ТГСК от неродственных совместимых доноров имели более низкие уровни ОВ и выживаемости без РТПХ и рецидивов по сравнению с другими типами доноров. Трехлетние показатели безрецидивной летальности (NRM) среди всех пациентов составляли 7,84% (95% CI 4,36-12,62). Адаптированное многовариантное моделирование общей выживаемости показало, что риск гибели пациентов после ТГСК от неродственного донора был в 3,6 раза выше, чем у пациентов, получивших ТГСК от гаплоидентичных доноров (P=0.05). Аналогично, риск безрецидивной смертности (NRM) после ТГСК от неродственных доноров был в 6 раз выше, чем при ТГСК от гаплоидентичных доноров (P=0.002). Однако частота рецидивов не различалась существенно между двумя указанными группами.</p> <h3>Выводы</h3> <p style="text-align: justify;">В данном исследовании показано, что ТГСК от гаплоидентичных доноров была ассоциирована с более высокими уровнями выживаемости, по сравнению с ТГСК от неродственных совместимых доноров. Таким образом, ТГСК от гаплоидентичных доноров может быть предложена в качестве практичной и ценной клинической опции, для пациентов молодых возрастов с острыми лейкозами в случае отсутствия совместимых доноров.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Острый лейкоз, аллогенная трансплантация гемопоэтических клеток, совместимые родственные доноры, неродственные доноры, гаплоидентичные доноры, клинические исходы.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(6042) "Трансплантация аллогенных гематопоэтических клеток (алло-ТГСК) является единственной потенциальной возможностью излечения острого лейкоза. Многие параметры существенно влияют на конечный исход ТГСК, в т.ч. тип донора, источник стволовых клеток и применяемый режим кондиционирования. При отсутствии HLA-совместимого родственного донора, возможными кандидатами могут быть неродственные совместимые или гаплоидентичные доноры для пациентов с показаниями к ТГСК. Для того, чтобы сопоставить исходы ТГСК от доноров различного типа с кондиционированием без облучения, мы сравнили в рамках одноцентрового исследования результаты трансплантации интактных ГСК периферической крови от совместимых и несовместимых, родственных и неродственных доноров, и гаплоидентичных доноров реципиентам детского, подросткового возрастов и молодым взрослым с острыми лейкозами.
Пациенты и методы
В данном ретроспективном исследовании, проводившемся с 2014 по 2021 г., мы оценивали исходы ТГСК с реплецией Т-лимфоцитов от гаплоидентичных доноров или неродственных доноров (совместимость – 10/10 или 9/10), а также в сравнении с неродственными донорами у пациентов с острыми лейкозами этих возрастных групп. Кондиционирование при ТГСК проводили с применением миелоаблативного режима с бусульфаном и циклофосфамидом и без ионизирующего облучения. Профилактика РТПХ включала назначение циклоспорина А всем пациентам, кроличий антитимоцитарный глобулин для неродственных и гаплоидентичных доноров, и циклофосфамид при ТГСК от гаплоидентичных доноров. Статистическую обработку проводили с помощью многовариантного пропорционального анализа рисков по Коксу и анализ конкурирующих рисков.
Результаты
Средний срок наблюдения составлял 28,7 мес. (95% CI: 21,9-34,9). Трехлетняя общая выживаемость (ОВ) и выживаемости без РТПХ и рецидивов были, соответственно, 68,81% (95% CI: 60,08%-76,01%) и 44.19% (95% CI: 35,52%-52,49%). Пациенты после ТГСК от неродственных совместимых доноров имели более низкие уровни ОВ и выживаемости без РТПХ и рецидивов по сравнению с другими типами доноров. Трехлетние показатели безрецидивной летальности (NRM) среди всех пациентов составляли 7,84% (95% CI 4,36-12,62). Адаптированное многовариантное моделирование общей выживаемости показало, что риск гибели пациентов после ТГСК от неродственного донора был в 3,6 раза выше, чем у пациентов, получивших ТГСК от гаплоидентичных доноров (P=0.05). Аналогично, риск безрецидивной смертности (NRM) после ТГСК от неродственных доноров был в 6 раз выше, чем при ТГСК от гаплоидентичных доноров (P=0.002). Однако частота рецидивов не различалась существенно между двумя указанными группами.
Выводы
В данном исследовании показано, что ТГСК от гаплоидентичных доноров была ассоциирована с более высокими уровнями выживаемости, по сравнению с ТГСК от неродственных совместимых доноров. Таким образом, ТГСК от гаплоидентичных доноров может быть предложена в качестве практичной и ценной клинической опции, для пациентов молодых возрастов с острыми лейкозами в случае отсутствия совместимых доноров.
Ключевые слова
Острый лейкоз, аллогенная трансплантация гемопоэтических клеток, совместимые родственные доноры, неродственные доноры, гаплоидентичные доноры, клинические исходы.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(6042) "Трансплантация аллогенных гематопоэтических клеток (алло-ТГСК) является единственной потенциальной возможностью излечения острого лейкоза. Многие параметры существенно влияют на конечный исход ТГСК, в т.ч. тип донора, источник стволовых клеток и применяемый режим кондиционирования. При отсутствии HLA-совместимого родственного донора, возможными кандидатами могут быть неродственные совместимые или гаплоидентичные доноры для пациентов с показаниями к ТГСК. Для того, чтобы сопоставить исходы ТГСК от доноров различного типа с кондиционированием без облучения, мы сравнили в рамках одноцентрового исследования результаты трансплантации интактных ГСК периферической крови от совместимых и несовместимых, родственных и неродственных доноров, и гаплоидентичных доноров реципиентам детского, подросткового возрастов и молодым взрослым с острыми лейкозами.
Пациенты и методы
В данном ретроспективном исследовании, проводившемся с 2014 по 2021 г., мы оценивали исходы ТГСК с реплецией Т-лимфоцитов от гаплоидентичных доноров или неродственных доноров (совместимость – 10/10 или 9/10), а также в сравнении с неродственными донорами у пациентов с острыми лейкозами этих возрастных групп. Кондиционирование при ТГСК проводили с применением миелоаблативного режима с бусульфаном и циклофосфамидом и без ионизирующего облучения. Профилактика РТПХ включала назначение циклоспорина А всем пациентам, кроличий антитимоцитарный глобулин для неродственных и гаплоидентичных доноров, и циклофосфамид при ТГСК от гаплоидентичных доноров. Статистическую обработку проводили с помощью многовариантного пропорционального анализа рисков по Коксу и анализ конкурирующих рисков.
Результаты
Средний срок наблюдения составлял 28,7 мес. (95% CI: 21,9-34,9). Трехлетняя общая выживаемость (ОВ) и выживаемости без РТПХ и рецидивов были, соответственно, 68,81% (95% CI: 60,08%-76,01%) и 44.19% (95% CI: 35,52%-52,49%). Пациенты после ТГСК от неродственных совместимых доноров имели более низкие уровни ОВ и выживаемости без РТПХ и рецидивов по сравнению с другими типами доноров. Трехлетние показатели безрецидивной летальности (NRM) среди всех пациентов составляли 7,84% (95% CI 4,36-12,62). Адаптированное многовариантное моделирование общей выживаемости показало, что риск гибели пациентов после ТГСК от неродственного донора был в 3,6 раза выше, чем у пациентов, получивших ТГСК от гаплоидентичных доноров (P=0.05). Аналогично, риск безрецидивной смертности (NRM) после ТГСК от неродственных доноров был в 6 раз выше, чем при ТГСК от гаплоидентичных доноров (P=0.002). Однако частота рецидивов не различалась существенно между двумя указанными группами.
Выводы
В данном исследовании показано, что ТГСК от гаплоидентичных доноров была ассоциирована с более высокими уровнями выживаемости, по сравнению с ТГСК от неродственных совместимых доноров. Таким образом, ТГСК от гаплоидентичных доноров может быть предложена в качестве практичной и ценной клинической опции, для пациентов молодых возрастов с острыми лейкозами в случае отсутствия совместимых доноров.
Ключевые слова
Острый лейкоз, аллогенная трансплантация гемопоэтических клеток, совместимые родственные доноры, неродственные доноры, гаплоидентичные доноры, клинические исходы.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28533" ["VALUE"]=> array(2) { ["TEXT"]=> string(1215) "<p><sup>1</sup> Отдел клеточной терапии у детей, НИИ онкологии, гематологии и клеточной терапии (RIOHCT), Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br> <sup>2</sup> НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br> <sup>3</sup> Отдел биостатистики и эпидемиологии, НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br> <sup>4</sup> Отдел инфекционных болезней, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1137) "1 Отдел клеточной терапии у детей, НИИ онкологии, гематологии и клеточной терапии (RIOHCT), Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
2 НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
3 Отдел биостатистики и эпидемиологии, НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
4 Отдел инфекционных болезней, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
1 Отдел клеточной терапии у детей, НИИ онкологии, гематологии и клеточной терапии (RIOHCT), Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
2 НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
3 Отдел биостатистики и эпидемиологии, НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
4 Отдел инфекционных болезней, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
Introduction
Over the past decades, allogeneic stem cell transplantation (allo-HSCT) has been used worldwide as a technology aimed both the long-term management and cure of malignant hematological diseases [1]. Allo-HSCT remains a valuable option for treatment of chronic myeloid leukemia (CML) in era of tyrosine kinase inhibitors (TKI) [2-6]. The transplant-eligible population consists of the CML patients with predicted poor outcome if treated with TKIs alone. Despite the superiority of drug treatment, the development of transplant technology, i.e., usage of reduced intensity conditioning regimens, increased donor availability, led to improvement in the results of allo-HSCT in these patients [7,8]. Thus, transplantation is still a potentially curative therapeutic mode in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with 2 TKIs, and patients with advanced-phase CML.
Unfavorable results are mostly associated with impaired graft function, which is manifested in the lack of control over the underlying disease and subsequent relapse, as well as in primary graft failure (PrGF) and poor graft function (PoGF) [9-12]. Several risk factors of post-transplant graft failure were revealed, e.g., patient’s age, donor-recipient blood mismatch and CMV infection (13]. Treatment options for poor graft functioning are still limited. In addition to reinfusion of stem cell, some recent studies report, e.g., positive effects of Eltrombopag, a thrombopoietin mimetic [14].
The aim of the study was to assess the incidence and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
Materials and methods
Patients and data collection
We carried out retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in R. M. Gorbacheva Research Institute at the Pavlov University between 1995 and 2020. Information on the disease stage at diagnosis, time to allo-HSCT, transplantation procedure, relapse, and treatment following allo-HSCT was gathered via systematic reviews of the patient records. General approaches to evaluation of HSCT patients at our clinic were described elsewhere [15].
Definitions
CML was diagnosed on the basis of clinical and laboratory data, the detection of Philadelphia (Ph) chromosome and/or the chimeric BCR-ABL gene. Disease phase was defined according to the WHO classification [16]. The first chronic phase (CP1) was recognized in the absence of accelerated phase (AP) and/or blast crisis (BC) in the patient’s history, otherwise CP≥2 was registered. Hematological, cytogenetic and molecular response to the treatment prior to allo-HSCT was defined using ELN criteria [17].
Indications for HSCT
Indications for HSCT were as follows: 1) AP/BC at diagnosis or progression to AP/BC; 2) treatment failure in pre-TKI era; 3) treatment failure due to TKI resistance/intolerance; 4) T315I mutation. TKI resistance and TKI intolerance were defined according to ELN criteria [17].
Laboratory studies
For cytogenetic evaluation, conventional synchronized culture was performed for 48 hours with at least 20 metaphases analyzed per a sample (GTG method). Leukemia cell karyotype was evaluated according to International System for Human Cytogenetic Nomenclature (ISCN) [18]. In cases when the standard cytogenetic investigation was not available (i.e., insufficient material), the bone marrow was assessed with fluorescence in situ hybridization (FISH) probes aimed for detection of (9;22) variants (LSI BCR-ABL, Dual Color, Dual Fusion, "Vysis").
Additional chromosomal abnormalities (ACA) were defined as any structural and numerical chromosomal aberrations other than t(9;22)(q34;q11) (detected by cytogenetic or molecular assays for cryptic abnormalities).
Molecular response after allo-HSCT was evaluated according to the National Comprehensive Cancer Network (NCCN) criteria (2021). PCR monitoring of BCR/ABL was carried out according to NCCN Guidelines once in 3 months for 2 years, then once in every 3 to 6 months. The relative BCR-ABL1 expression level was evaluated according to method described by Gabert et al [19]. This technique includes the following stages: 1) total RNA extraction from peripheral blood of patients with CML, 2) reverse transcription with random hexameric primers, 3) real-time PCR with primers and probes specific to р210, р190 control ABL gene sequences.
Assessment of relative expression levels was based on evaluation of BCR-ABL1/ABL1 ratios in the studied cDNA samples. The ABL1 gene was used for normalization of the results. In order to determine copy numbers of the BCR-ABL1 and ABL1 transcripts, and to assess the reaction effectiveness, standard dilution curves were plotted using a plasmid with inserts of known target gene sequences (Invitrogen, USA), at a standard concentration ranges of 102-106 copies/mcl, according to 2020 European LeukemiaNet (ELN) Recommendations [17]. ABL kinase domain mutations were determined by Sanger direct sequencing.
Post-transplant monitoring
Post-transplant engraftment was defined as absolute neutrophil count (ANC) of >0.5×109/L without administration of colony-stimulating factor within 3 days. Primary graft failure (PrGF) was diagnosed in absence of donor cells in recipient’s bone marrow by the day +30. Donor chimerism was checked at the time of myelopoiesis recovery, i.e. ANC> 0.5×109/L, and by the days +30, 60, +100, +200, and in case of any cytopenia, or signs of relapse. Post-transplant relapse was diagnosed in cases of clinical progression to AP/BC, cytogenetic relapse, or molecular relapse defined as two consecutive positive PCR tests, or, at least, 1-log persistent increase of BCR/ABL transcript level.
The criteria for severe poor graft function (sPGF) were as follows: cytopenia in two or more hematopoietic lineages (platelets <20×109/l, ANC <0.5×109/l, hemoglobin <70 g/l) any time after documented engraftment in presence of full or stable mixed donor chimerism >90% without signs of relapse of underlying disease, rejection or acute graft-versus-host disease (GVHD) grade III-IV.
Secondary graft failure was defined as loss of donor hematopoiesis to <5% and/or ANC counts to <0.5×109/L after initial engraftment being not related to relapse, infection, or drug toxicity [20].
Statistical evaluation
Descriptive characteristics of the cohort included number of cases, proportions for discrete factors, medians and range for continuous values. Individual pre-transplant risk for the HSCT patients was evaluated according to Gratwohl [21]. Overall survival (OS) was assessed using the Kaplan-Meier method from the time of allo-HSCT to the date of last contact or the date of death. Death from any cause was considered as an event.
Survival analysis was performed using log-rank test. Relapse and non-relapse mortality (NRM) rates were summarized using cumulative incidence estimates, with NRM as competing risk for relapse, and relapse regarded as competing risk for NRM.
The event-free survival (EFS) was estimated as a period from allo-HSCT until last contact date, death, or any of the following events: any kind of post-transplant relapse, graft-versus-host disease (GVHD) grade III-IV, severe poor graft function, or secondary graft failure. PrGF and sPGF were estimated as a proportion of cases in the total cohort. Cumulative incidence of sPGF was calculated with respect to competing risks (death before day +30, any type of relapse, GVHD grade III-IV).
The differences between groups were assessed using Fisher's exact test, Pearson χ2 test, and Mann-Whitney U-test for categorical and quantitative characteristics respectively, and Gray’s test for cumulative incidences. All the tests were two-sided, and P-values <0.05 were assessed as indicating for significant associations. Statistical analysis was performed using SPSS, IBM Statistics and EZR free statistical environment, version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
General characteristics of the patients and HSCT procedure
A total of 121 patients diagnosed with CML had undergone allo-HSCT. The median patients’ age was 37 years (range: 18-66). Other baseline characteristics for these patients are presented in Table 1.
The median time between CML diagnosis and allo-HSCT was 31 months (4.5-260). A total of 80 (66%) patients were transplanted in chronic phase (CP), the remaining 41 (34%) patients were in the active phase (AP or BC) at the time of HSCT. The median follow-up from allo-HSCT to the time of the last contact was 15 months (0.5-294).
HLA-matched or partially mismatched unrelated donors were used in 78 cases (65%), while matched related donors were employed in 34 cases (28%), and 9 (7%) patients received haploidentical allo-HSCT. The proportion of bone marrow (BM) and peripheral blood stem cells (PBSC) as the graft sources was almost equal: 49% (n=59) versus 51% (n=62).
Conditioning regimen included oral busulfan 8-12 mg/kg or melphalan 140 mg/m2 in combination with fludarabine 180 mg/m2 or cyclophosphamide. GVHD prophylaxis included calcineurin inhibitor (tacrolimus or cyclosporine A) and mycophenolate mofetil (30 mg/kg), or short course of posttransplant metotrexate, with or without antithymocyte globulin (horse, 60 mg/kg, or rabbit preparations, 5 mg/kg on day -3, -2, or high-dose), post-transplant cyclophosphamide (50 mg/kg, day +3 and +4 after allo-HSCT)/Alemtuzumab was used in two cases (Table 2).


Figure 1. Cumulative incidence of poor graft function post-HSCT in CML patients
Survival and relapse rates
Engraftment was documented in 106 (88%) patients, with median time to neutrophil recovery of 22 (8-58) days. Early death with no signs of engraftment before day +30 occurred in two cases. Thirty-one patients developed post-transplant relapse of any type with median time after allo-HSCT of 106 days (range: 15-333), included early CML relapse/progression before day +30 in 5 cases.
PrGF was documented in 8 (7%) cases. Two patients developed secondary graft failure, both in about two months after initial engraftment with lethal outcome due to severe bacterial infection. Severe poor graft function was diagnosed in 11 (9% of engrafted patients) with cumulative incidence of 10% (95% CI, 5-19) within 1 year after allo-HSCT (Fig. 1). Median time from HSCT to sPGF diagnosis was 43 (18-114) days.
The 1-year cumulative incidence rates of relapse and NRM comprised 35% (95% CI, 26-46) and 26% (95% CI, 18-35), respectively (Fig. 2).
A total of 57 (47%) patients died, the 1-year OS was 60% (95% CI, 51-69). Median OS was not reached. One-year EFS was 41% (95% CI, 32-50), median EFS was 271 (95% CI, 96-365) days (Fig. 3).

Figure 2. One-year cumulative incidence of relapses and NRM after allo-HSCT in CML patients

Figure 3. One-year overall and event-free survival after allogeneic HSCT in CML patients
Factors associated with primary graft failure and severe poor graft function
Among various pre-transplant characteristics, the presence of additional chromosomal abnormalities (ACA) was associated with cumulative incidence of PrGF and sPGF after HSCT. Thus, PrGF was 14% in the group with detectable ACA versus 3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% versus 12% in those without ACA, p=0.09. HLA-matched allo-HSCTs were beneficial for engraftment: 96% for HLA-matched transplantations vs 89% for allo-HSCT from HLA-mismatched donors, and 78% for haploidentical donors (p=0.05). Other pre-transplant factors didn’t show any statistical correlation with graft failure syndromes after HSCT (Table 3).
Table 3. Potential risk factors for the graft failure after allo-HSCT in CML patients
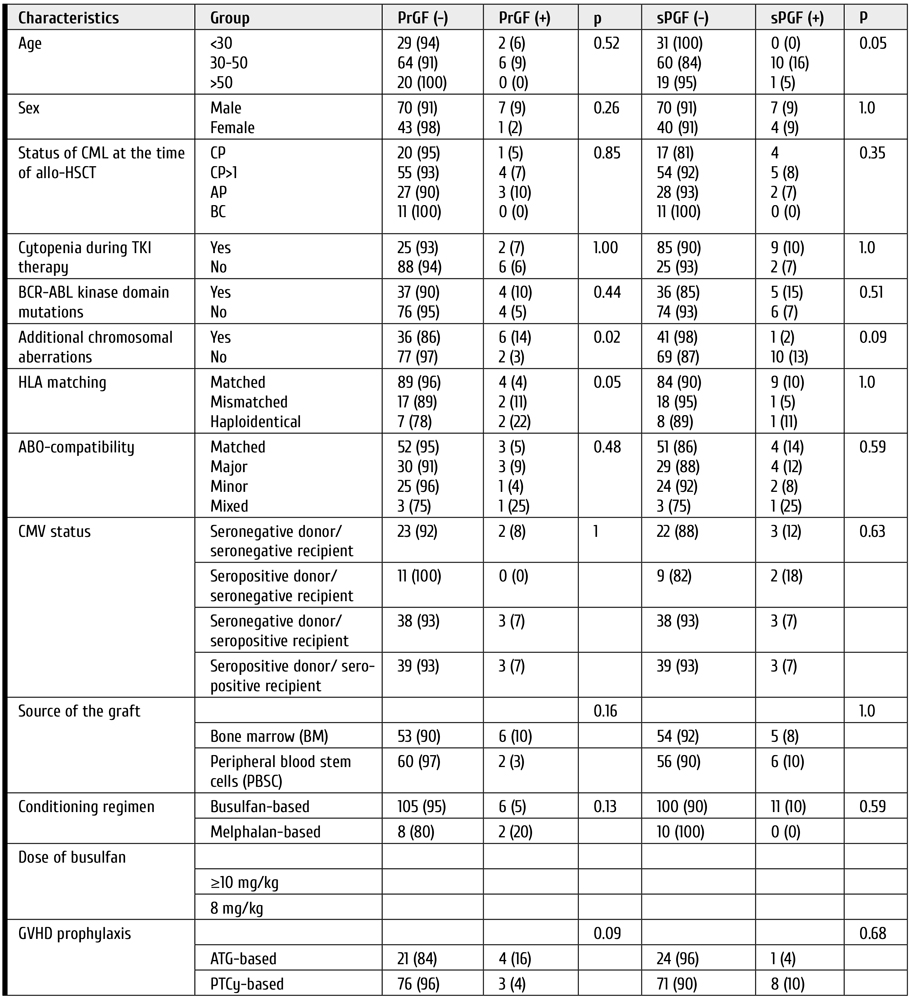
Clinical features and outcomes of graft failure and severe poor graft function
The median follow-up time after allo-HSCT was 68 days (range: 43-1792). All the patients with primary graft failure (PrGF) (n=8) were administered G-CSF, antimicrobial therapy and transfusion support. Two patients received donor lymphocyte infusions without any effect. The second allo-HSCT was performed in 4 cases. A total of 7 patients had lethal outcome (6, of infectious complications; 1, of relapse), whereas one patient is alive after the 2nd allo-HSCT (Fig. 4).

Figure 4. Treatment and outcomes of primary graft failure (PrGF) in CML patients after HSCT
Eleven patients exhibited severe poor graft function (sPGF) within median time of 21 (0-92) days after engraftment. Median length of sPGF was 52 days (range: 14-215). The median time of follow-up after allo-HSCT was 977 days (range: 45-2712).
Early sPGF with criterial cytopenia persisting after engraftment was diagnosed in 4 cases (36%), the remaining patients developed cytopenia after a period of normal graft function. A total of 3 cases of sPGF (27%) developed within 30 days after acute GVHD 2-3 grade (Fig. 5).

Figure 5. Timeline of severe poor graft function (SPGF) in a group of CML patients
All the patients with sPGF received antimicrobial therapy, transfusion support, and G-CSF in case of neutropenia. Other therapeutic options for sPGF therapy were: rituximab (n=4), the second allo-HSCT, or boost stem cell infusion (n=3); eltrombopag (n=1); supportive care (n=5), as seen from Fig. 4. Normal graft function was restored in 8 patients.
A total of 4 patients died. The causes of death were infectious complications (n=3) and late post-transplant relapse (n=1) (Fig. 6).
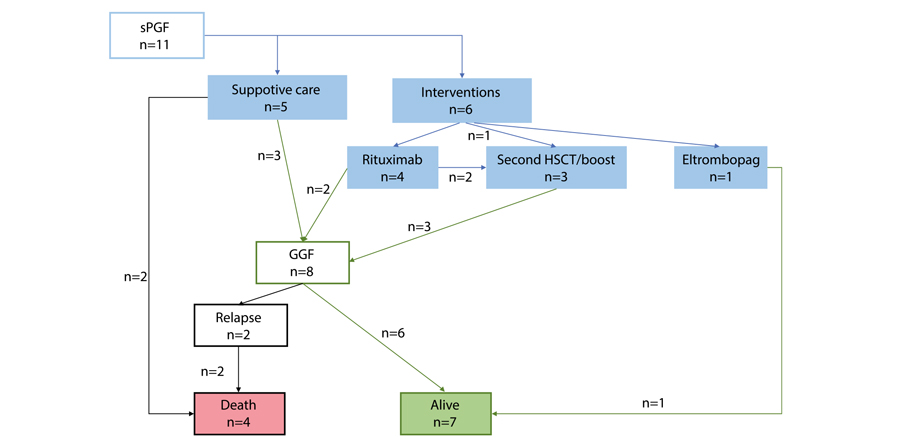
Figure 6. Treatment and outcomes of severe poor graft function (sPGF) in CML patients post-HSCT
Two cases of secondary graft failure occurred in about 3 months after allo-HSCT. Both patients died due to severe infection.
The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF as compared with those, who were free of these complications. Cumulative incidence of leukemia relapses was 31% (95% CI, 23-42), and 25% (95% CI, 4-87) in the patients with PrGF and engraftment (p=0.97), compared with 22% (95% CI, 3-54) and 32% (95% CI, 24-43) in the patients with sPGF and without sPGF (p=0.52), respectively.
Primary graft failure (PrGF) but not severe poor graft failure (sPGF) significantly increased non-relapse mortality during the first year after allo-HSCT. One-year NRM was 23% (95% CI, 15-32) in engrafted patients versus 71% (95% CI, 39-96) in the patients with PrGF (p<0.0001). Patients with and without sPGF had similar NRM: 20% (95% CI, 5-59) versus 26% (95% CI, 18-36) (p=0.74).
One-year OS was significantly lower in patients with PrGF: 13% (95% CI, 0.7-42) versus 64% (95% CI, 54-72) (p<0.0001) (Fig. 7). On the contrary, sPGF had no statistically significant influence on OS: 73% (95% CI, 37-90) versus 59% (95% CI, 49-69) (p=0.47).

Figure 7. Impact of primary graft failure (PrGF, A), and severe poor graft function (sPGF, B) on overall survival post-HSCT in CML patients
Discussion
In context of TKI therapy progress, the indications for allo-HSCT in CML are becoming more stringent, with respect both to selective TKI choice, relapse diagnostics, and improved transplant technologies [22]. In this regard, it becomes relevant to investigate the causes of allo-HSCT failure and to determine the risk factors for PrGF and sPGF in CML patients. While the factor of post-transplant relapse is discussed in most publications, the issues of PrGF and sPGF remain poorly reflected. Only few authors provided clear definitions and data on the incidence of these complications (mostly PrGF) in the patients with CML. At the same time, most studies of posttransplant graft failure syndromes show that the diagnosis of CML may be among risk factors of this complication. However, most previous studies concerned a heterogeneous range of diagnoses, e.g., acute leukemia, chronic myelo- and lymphoproliferative and non-malignant diseases. To our knowledge, the present work evaluates for the first time the incidence of both PrGF and PGF in a homogeneous cohort of CML patients.
According to our results, PrGF occurred in 7% of cases, thus being higher than in patients with acute leukemia as confirmed by other publications [10]. On the contrary, cumulative incidence of sPGF during the first year after allo-HSCT was 10%. This level is less than in general population of patients after allo-HSCT [15]. A prospective non-interventional study from the Chronic Malignancy Working Party of the EBMT also showed increased rate of graft dysfunction in CML patients after allo-HSCT. Impact of pre-transplant treatment with tyrosine kinase inhibitors of second generation on the allograft function due to myelotoxicity is still under discussion [23]. Presumably, the similar factors may contribute to the development of both PrGF and sPoGF.
We analyzed the data associated with characteristics of patients, donors, and the HSCT procedure. Due to small number of cases in the target groups, only univariate analysis was performed. In contrast to many studies, conditioning regimen, the source and cellularity of the graft, CMV status of the donor and the patient, ABO incompatibility did not show any statistical significance of the disease status, although it is proved an important characteristic for the prognosis of primary graft failure and poor graft function [10, 11, 24, 25, 26, 27, 28, 29, 30].
Nevertheless, it was the presence of ACA that showed statistical significance for PrGF. This may suggest insufficient control of the underlying disease to be among the main causes of any type of graft dysfunction. However, no association between post-transplant relapse and sPGF was noted in our study. The disease recurrence after resolution of graft failure remains an important cause of treatment failure. Contribution of the underlying disease to development of PrGF and sPGF needs to be investigated in future.
HLA incompatibility was another factor for PrGF in univariate analysis. The importance of this characteristic for HSC engraftment is well known [13, 15, 30]. Haploidentical HSCTs in this analysis showed larger proportion of PrGF and sPGF, but this result needs further proofs, as our group was small and mostly retrospective.
The question still exists if the intensity of conditioning regimen may contribute to insufficient hematopoietic reconstitution after allo-HSCT. Impairment of bone marrow microenvironment exposed to high doses of alkylating agents may be one of the possible pathogenic pathways [13, 31]. Nevertheless, our study did not show significant influence of conditioning intensity upon the clinical outcomes.
Natural history of the patients who developed graft failure and poor graft function was of particular interest in this retrospective study. Despite various interventions, primary graft failure is still associated with poor outcomes and death, mostly, due to infectious complications.
Survival and NRM analysis showed that, despite the rare occurrence, PrGF and sPGF are life-threatening and resource-consuming problems. Both PrGF and sPGF need aggressive approach in order to improve outcomes of allo- HSCT. Intensive interventions might be a rescue for, at least, a part of the patients and lead to prolonged survival. Stimulation of residual HSCs by TPO agonists using in the setting of persistent cytopenia after HSCT by several groups might be a promising strategy, although influence of TPO agonists on the leukemic stem cells and risk of relapse is debated. Early employment of a CD34+-selected stem cell boost, or a second allogeneic HSCT to restore an effective haematopoiesis might also be a life-saving option. Identification of patients at high risk for these complications and development strategies for early intervention might be in scope of further investigation.
Conclusion
Both PrGF and sPGF are significant life-threatening problems in allo-HSCT. Specifically, PrGF but not severe poor graft failure (sPGF) significantly increased non-relapse mortality during the first year after allo-HSCT. Meanwhile, the incidence of post-transplant relapses did not differ in the CML patients exhibiting primary graft failure or severe poor graft function. Identification of risk factors for these complications can improve the results of this treatment, by planning HSCT technology, to minimize them and modify approaches to post-transplant therapy.
Conflict of interest
None declared.
References
- Afanasyev BV, Zubarovskaya LS. Role of hematopoietic stem cell transplantation in therapy of adult patients with acute leukemias. Oncohematology. 2006;1(1-2): 70-85. (In Russian).
- Lübking A, Dreimane A, Sandin F et al. Allogeneic stem cell transplantation for chronic myeloid leukemia in the TKI era: population-based data from the Swedish CML registry. Bone Marrow Transplant. 2019;54, 1764-1774. doi: 10.1038/s41409-019-0513-5
- Barrett AJ, Ito S. The role of stem cell transplantation for chronic myelogenous leukemia in the 21st century. Blood. 2015;125(21):3230-3235. doi: 10.1182/blood-2014-10-567784
- Lyubimova LS, Kuzmina LA, E.S.Urnova ES, Zhelnova ES, Anukhina MV, Mendeleyeva LP, et al. Early HLA-identical bone marrow transplantation during chronic myeloid leukemia chronic phase vs. long-term tyrosine kinase inhibitor therapy? Gematologyia i Transfusiologiya. 2012; 57 (3): 6-10. (In Russian).
- Morozova EV, Vlasova YI, Barabanshikova MV, Afanaseva KS, Iurovskaia KS, Gindina TL, Barchatov IM, Alyanskiy AL, Bakin EA, Bondarenko SN, Moiseev IS, Zubarovskaya LS, Afanasyev BV. Allogeneic haematopoietic stem cell transplantation with reduced-intensity conditioning in chronic myeloid leukaemia. Russian Journal of Hematology and Transfusiology. 2020; 65(4): 386-402. (In Russian.). doi: 10.35754/0234-5730-2020-65-4-386-402
- Boehm A, Walcherberger B, Sperr WR, Woehrer S, Dieckmann K, Rosenmayr A, et al. Improved outcome in patients with chronic myelogenous leukemia after allogeneic hematopoietic stem cell transplantation over the past 25 years: A single-center experience. Biol Blood Marrow Transplant. 2011; 17: 133-140. doi: 10.1016/j.bbmt.2010.06.019
- Kolb HJ. Graft-versus-leukemia effects of transplantation and donor lymphocytes. Blood 2008; 112 (12): 4371-4383.
doi: 10.1182/blood-2008-03-077974 - Klyuchnikov E, Kröger N, Brummendorf TH et al. Current status and perspectives of tyrosine kinase inhibitor treatment in the posttransplant period in patients with chronic myelogenous leukemia (CML). Biol Blood Marrow Transplant. 2010; 16 (3): 301-310.
doi: 10.1016/j.bbmt.2009.08.019 - Bonifacio M, Stagno F, Scaffidi L, Krampera M, Raimondo FD. Management of chronic myeloid leukemia in advanced phase. Front Oncol. 2019; Oct 25; 9:1132. doi: 10.3389/fonc.2019.01132
- Olsson RF, Logan BR, Chaudhury S, Zhu X, Akpek G, Bolwell BJ, et al. Primary graft failure after myeloablative allogeneic hematopoietic cell transplantation for hematologic malignancies. Leukemia. 2015; 29(8), 1754-1762. doi: 10.1038/leu.2015.75
- Olsson RF, Berggren DM, Ringden O, Mattsson J, Remberger M. Graft failure in reduced intensity conditioning allogeneic hematopoietic stem cell transplantation. Blood. 2013; 122 (21): 4559. doi: 10.1182/blood.V122.21.4559.4559
- Locatelli F, Lucarelli B, Merli P. Current and future approaches to treat graft failure after allogeneic hematopoietic stem cell transplantation. Expert Opinion Pharmacother. 2014;15(1): 23-36. doi: 10.1517/14656566.2014.852537
- Xiao Y, Song J, Jiang Z, Li Y, Gao Y, Xu W, Lu Z, Wang Y, Xiao H. Risk-factor analysis of poor graft function after allogeneic hematopoietic stem cell transplantation. Int J Med Sci. 2014; 11(6):652-657. doi: 10.7150/ijms.6337
- Marotta S, Marano L, Ricci P, Cacace F, Frieri C, Simeone L, Trastulli F, Vitiello S, Cardano F, Pane F, Risitano AM. Eltrombopag for post-transplant cytopenias due to poor graft function. Bone Marrow Transplant. 2019; 54(8):1346-1353. doi: 10.1038/s41409-019-0442-3
- Rudakova TA, Kulagin AD, Klimova OU, Golubovskaya IK, Darskaya EI, Bykova TA, Smirnova AG, Morozova EV, Bondarenko SN, Moiseev IS, et al. Severe poor graft function after allogeneic hematopoietic stem cell transplantation in adult patients: Incidence, risk factors, and outcomes. Clinical Oncohematology. 2019;12(3):309-318 (In Russ). doi: 10.21320/2500-2139-2019-12-3-309-318
- Turkina AG, Zaritsky AYu, Chelysheva EYu. et al. Clinical recommendations for the diagnosis and treatment of chronic myelogenous leukemia. Clinical Oncohematology. 2017;10(3):294-316. (In Russian). doi: 10.21320/2500-2139-2017-10-3-294-316
- Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, Cervantes F, Clark RE, Cortes JE, Guilhot F, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122:872-884.
doi: 10.1182/blood-2013-05-501569 - McGowan-Jordan J, Simons A, Schmid M. International Standing Committee on Human Cytogenomic Nomenclature, 2016.
doi: 10.1159/isbn.978-3-318-06861-0 - Gabert J, Beillard E, van der Velden V., et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia- A Europe Against Cancer Program. Leukemia. 2003.17: 2318-2357. doi: 10.1038/sj.leu.2403135
- Valcárcel D, Sureda A. Graft Failure. In: Carreras E, Dufour C, Mohty M, Kröger N, editors. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies [Internet]. 7th ed. Cham (CH): Springer; 2019. Chapter 41. PMID: 32091792. https://www.ncbi.nlm.nih.gov/books/NBK553942/. doi: 10.1007/978-3-030-02278-5
- Gratwohl A. The EBMT risk score. Bone Marrow Transplantation. 2012;47:749-56. doi: 10.1038/bmt.2011.110
- Craddock CF. We do still transplant CML, don’t we? Hematology Am Soc Hematol Educ Program. 2018 (1): 177-184.
https://doi.org/10.1182/asheducation-2018.1.177 - Masouridi-Levrat S, Olavarria E, Iacobelli S, Aljurf M, Morozova E, Niittyvuopio R, Sengeloev H, Reményi P, Helbig G, Browne P, et al. Outcomes and toxicity of allogeneic hematopoietic cell transplantation in chronic myeloid leukemia patients previously treated with second-generation tyrosine kinase inhibitors: a prospective non-interventional study from the Chronic Malignancy Working Party of the EBMT. Bone Marrow Transplant. 2022; 57(1):23-30. doi: 10.1038/s41409-021-01472-x
- Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, Ringden O. Graft failure in the modern era of allogeneic hematopoietic SCT [published correction appears in Bone Marrow Transplant. 2013 Apr; 48(4):616]. Bone Marrow Transplant. 2013;48(4):537-543. doi: 10.1038/bmt.2012.239
- Moiseev IS, Morozova EV, Vlasova YY, et al. Interim results of the randomized trial of post-transplanation cyclophosphamide versus rabbit ATG for graft-versus-host disease prophylaxis in chronic myeloproliferative neoplasms and myelodysplastic syndrome. Cell Ther Transplant. 2016; 5(3):62-63. doi: 10.18620/ctt-1866-8836-2016-5-3-49-50
- Hallemeier C. Letter to the editor. Re: High rate of graft failure in 25 patients with chronic myelogenous leukemia conditioned with a reduced-intensity regimen of 550 cGy total body irradiation and cyclophosphamide for unrelated donor transplantation. Biol Blood Marrow Transplant. 2004; 10:726-727. doi: 10.1016/j.bbmt.2004.07.001
- Khoury H, Adkins, Brown RH, Pence, Vij R, Goodnough LT, et al. Low incidence of transplantation-related acute complications in patients with chronic myeloid leukemia undergoing aiiogeneic stem cell transplantation with a low-dose (550 cGy) total body irradiation conditioning regimen. Biol Blood Marrow Transplant. 2001; 7(6):352-358. doi: 10.1016/S1083-8791(01)80006-9
- Khoury HJ, Kukreja M, Goldman JM, Wang T, Halter J, Arora M, et al. Prognostic factors for outcomes in allogeneic transplantation for CML in the imatinib era: a CIBMTR analysis. Bone Marrow Transplant. 2012; 47, 810-816. doi: 10.1038/bmt.2011.194
- Radujkovic A, Dietrich S, Blok HJ, Nagler A, Ayuk F, Finke J, et al. Allogeneic stem cell transplantation for blast crisis chronic myeloid leukemia in the era of tyrosine kinase inhibitors: A retrospective study by the EBMT Chronic Malignancies Working Party. Biol Blood Marrow Transplant. 2019; 25(10): 2008-2016. doi: 10.1016/j.bbmt.2019.06.028
- Kuzmich YV, Alyanskiy AI, Ivanova NY, Vitrischak AA, Vladovskaya MD, Morozova YV, Bondarenko SN, Semenova YV, Zubarovskaya LS, Afanasyev BV. Analysis of the results of allogeneic hematopoietic stem cell transplantation depending on HLA matching of the unrelated donor/recipient pair. Oncohematology. 2014; 9(3):25-31. (In Russian). doi: 10.17650/1818-8346-2014-9-3-25-31
- Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, et al. CD34 selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014; 20(9): 1440-1443. doi: 10.1016/j.bbmt.2014.05.016
" ["~DETAIL_TEXT"]=> string(35387) "
Introduction
Over the past decades, allogeneic stem cell transplantation (allo-HSCT) has been used worldwide as a technology aimed both the long-term management and cure of malignant hematological diseases [1]. Allo-HSCT remains a valuable option for treatment of chronic myeloid leukemia (CML) in era of tyrosine kinase inhibitors (TKI) [2-6]. The transplant-eligible population consists of the CML patients with predicted poor outcome if treated with TKIs alone. Despite the superiority of drug treatment, the development of transplant technology, i.e., usage of reduced intensity conditioning regimens, increased donor availability, led to improvement in the results of allo-HSCT in these patients [7,8]. Thus, transplantation is still a potentially curative therapeutic mode in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with 2 TKIs, and patients with advanced-phase CML.
Unfavorable results are mostly associated with impaired graft function, which is manifested in the lack of control over the underlying disease and subsequent relapse, as well as in primary graft failure (PrGF) and poor graft function (PoGF) [9-12]. Several risk factors of post-transplant graft failure were revealed, e.g., patient’s age, donor-recipient blood mismatch and CMV infection (13]. Treatment options for poor graft functioning are still limited. In addition to reinfusion of stem cell, some recent studies report, e.g., positive effects of Eltrombopag, a thrombopoietin mimetic [14].
The aim of the study was to assess the incidence and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
Materials and methods
Patients and data collection
We carried out retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in R. M. Gorbacheva Research Institute at the Pavlov University between 1995 and 2020. Information on the disease stage at diagnosis, time to allo-HSCT, transplantation procedure, relapse, and treatment following allo-HSCT was gathered via systematic reviews of the patient records. General approaches to evaluation of HSCT patients at our clinic were described elsewhere [15].
Definitions
CML was diagnosed on the basis of clinical and laboratory data, the detection of Philadelphia (Ph) chromosome and/or the chimeric BCR-ABL gene. Disease phase was defined according to the WHO classification [16]. The first chronic phase (CP1) was recognized in the absence of accelerated phase (AP) and/or blast crisis (BC) in the patient’s history, otherwise CP≥2 was registered. Hematological, cytogenetic and molecular response to the treatment prior to allo-HSCT was defined using ELN criteria [17].
Indications for HSCT
Indications for HSCT were as follows: 1) AP/BC at diagnosis or progression to AP/BC; 2) treatment failure in pre-TKI era; 3) treatment failure due to TKI resistance/intolerance; 4) T315I mutation. TKI resistance and TKI intolerance were defined according to ELN criteria [17].
Laboratory studies
For cytogenetic evaluation, conventional synchronized culture was performed for 48 hours with at least 20 metaphases analyzed per a sample (GTG method). Leukemia cell karyotype was evaluated according to International System for Human Cytogenetic Nomenclature (ISCN) [18]. In cases when the standard cytogenetic investigation was not available (i.e., insufficient material), the bone marrow was assessed with fluorescence in situ hybridization (FISH) probes aimed for detection of (9;22) variants (LSI BCR-ABL, Dual Color, Dual Fusion, "Vysis").
Additional chromosomal abnormalities (ACA) were defined as any structural and numerical chromosomal aberrations other than t(9;22)(q34;q11) (detected by cytogenetic or molecular assays for cryptic abnormalities).
Molecular response after allo-HSCT was evaluated according to the National Comprehensive Cancer Network (NCCN) criteria (2021). PCR monitoring of BCR/ABL was carried out according to NCCN Guidelines once in 3 months for 2 years, then once in every 3 to 6 months. The relative BCR-ABL1 expression level was evaluated according to method described by Gabert et al [19]. This technique includes the following stages: 1) total RNA extraction from peripheral blood of patients with CML, 2) reverse transcription with random hexameric primers, 3) real-time PCR with primers and probes specific to р210, р190 control ABL gene sequences.
Assessment of relative expression levels was based on evaluation of BCR-ABL1/ABL1 ratios in the studied cDNA samples. The ABL1 gene was used for normalization of the results. In order to determine copy numbers of the BCR-ABL1 and ABL1 transcripts, and to assess the reaction effectiveness, standard dilution curves were plotted using a plasmid with inserts of known target gene sequences (Invitrogen, USA), at a standard concentration ranges of 102-106 copies/mcl, according to 2020 European LeukemiaNet (ELN) Recommendations [17]. ABL kinase domain mutations were determined by Sanger direct sequencing.
Post-transplant monitoring
Post-transplant engraftment was defined as absolute neutrophil count (ANC) of >0.5×109/L without administration of colony-stimulating factor within 3 days. Primary graft failure (PrGF) was diagnosed in absence of donor cells in recipient’s bone marrow by the day +30. Donor chimerism was checked at the time of myelopoiesis recovery, i.e. ANC> 0.5×109/L, and by the days +30, 60, +100, +200, and in case of any cytopenia, or signs of relapse. Post-transplant relapse was diagnosed in cases of clinical progression to AP/BC, cytogenetic relapse, or molecular relapse defined as two consecutive positive PCR tests, or, at least, 1-log persistent increase of BCR/ABL transcript level.
The criteria for severe poor graft function (sPGF) were as follows: cytopenia in two or more hematopoietic lineages (platelets <20×109/l, ANC <0.5×109/l, hemoglobin <70 g/l) any time after documented engraftment in presence of full or stable mixed donor chimerism >90% without signs of relapse of underlying disease, rejection or acute graft-versus-host disease (GVHD) grade III-IV.
Secondary graft failure was defined as loss of donor hematopoiesis to <5% and/or ANC counts to <0.5×109/L after initial engraftment being not related to relapse, infection, or drug toxicity [20].
Statistical evaluation
Descriptive characteristics of the cohort included number of cases, proportions for discrete factors, medians and range for continuous values. Individual pre-transplant risk for the HSCT patients was evaluated according to Gratwohl [21]. Overall survival (OS) was assessed using the Kaplan-Meier method from the time of allo-HSCT to the date of last contact or the date of death. Death from any cause was considered as an event.
Survival analysis was performed using log-rank test. Relapse and non-relapse mortality (NRM) rates were summarized using cumulative incidence estimates, with NRM as competing risk for relapse, and relapse regarded as competing risk for NRM.
The event-free survival (EFS) was estimated as a period from allo-HSCT until last contact date, death, or any of the following events: any kind of post-transplant relapse, graft-versus-host disease (GVHD) grade III-IV, severe poor graft function, or secondary graft failure. PrGF and sPGF were estimated as a proportion of cases in the total cohort. Cumulative incidence of sPGF was calculated with respect to competing risks (death before day +30, any type of relapse, GVHD grade III-IV).
The differences between groups were assessed using Fisher's exact test, Pearson χ2 test, and Mann-Whitney U-test for categorical and quantitative characteristics respectively, and Gray’s test for cumulative incidences. All the tests were two-sided, and P-values <0.05 were assessed as indicating for significant associations. Statistical analysis was performed using SPSS, IBM Statistics and EZR free statistical environment, version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
General characteristics of the patients and HSCT procedure
A total of 121 patients diagnosed with CML had undergone allo-HSCT. The median patients’ age was 37 years (range: 18-66). Other baseline characteristics for these patients are presented in Table 1.
The median time between CML diagnosis and allo-HSCT was 31 months (4.5-260). A total of 80 (66%) patients were transplanted in chronic phase (CP), the remaining 41 (34%) patients were in the active phase (AP or BC) at the time of HSCT. The median follow-up from allo-HSCT to the time of the last contact was 15 months (0.5-294).
HLA-matched or partially mismatched unrelated donors were used in 78 cases (65%), while matched related donors were employed in 34 cases (28%), and 9 (7%) patients received haploidentical allo-HSCT. The proportion of bone marrow (BM) and peripheral blood stem cells (PBSC) as the graft sources was almost equal: 49% (n=59) versus 51% (n=62).
Conditioning regimen included oral busulfan 8-12 mg/kg or melphalan 140 mg/m2 in combination with fludarabine 180 mg/m2 or cyclophosphamide. GVHD prophylaxis included calcineurin inhibitor (tacrolimus or cyclosporine A) and mycophenolate mofetil (30 mg/kg), or short course of posttransplant metotrexate, with or without antithymocyte globulin (horse, 60 mg/kg, or rabbit preparations, 5 mg/kg on day -3, -2, or high-dose), post-transplant cyclophosphamide (50 mg/kg, day +3 and +4 after allo-HSCT)/Alemtuzumab was used in two cases (Table 2).


Figure 1. Cumulative incidence of poor graft function post-HSCT in CML patients
Survival and relapse rates
Engraftment was documented in 106 (88%) patients, with median time to neutrophil recovery of 22 (8-58) days. Early death with no signs of engraftment before day +30 occurred in two cases. Thirty-one patients developed post-transplant relapse of any type with median time after allo-HSCT of 106 days (range: 15-333), included early CML relapse/progression before day +30 in 5 cases.
PrGF was documented in 8 (7%) cases. Two patients developed secondary graft failure, both in about two months after initial engraftment with lethal outcome due to severe bacterial infection. Severe poor graft function was diagnosed in 11 (9% of engrafted patients) with cumulative incidence of 10% (95% CI, 5-19) within 1 year after allo-HSCT (Fig. 1). Median time from HSCT to sPGF diagnosis was 43 (18-114) days.
The 1-year cumulative incidence rates of relapse and NRM comprised 35% (95% CI, 26-46) and 26% (95% CI, 18-35), respectively (Fig. 2).
A total of 57 (47%) patients died, the 1-year OS was 60% (95% CI, 51-69). Median OS was not reached. One-year EFS was 41% (95% CI, 32-50), median EFS was 271 (95% CI, 96-365) days (Fig. 3).

Figure 2. One-year cumulative incidence of relapses and NRM after allo-HSCT in CML patients

Figure 3. One-year overall and event-free survival after allogeneic HSCT in CML patients
Factors associated with primary graft failure and severe poor graft function
Among various pre-transplant characteristics, the presence of additional chromosomal abnormalities (ACA) was associated with cumulative incidence of PrGF and sPGF after HSCT. Thus, PrGF was 14% in the group with detectable ACA versus 3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% versus 12% in those without ACA, p=0.09. HLA-matched allo-HSCTs were beneficial for engraftment: 96% for HLA-matched transplantations vs 89% for allo-HSCT from HLA-mismatched donors, and 78% for haploidentical donors (p=0.05). Other pre-transplant factors didn’t show any statistical correlation with graft failure syndromes after HSCT (Table 3).
Table 3. Potential risk factors for the graft failure after allo-HSCT in CML patients
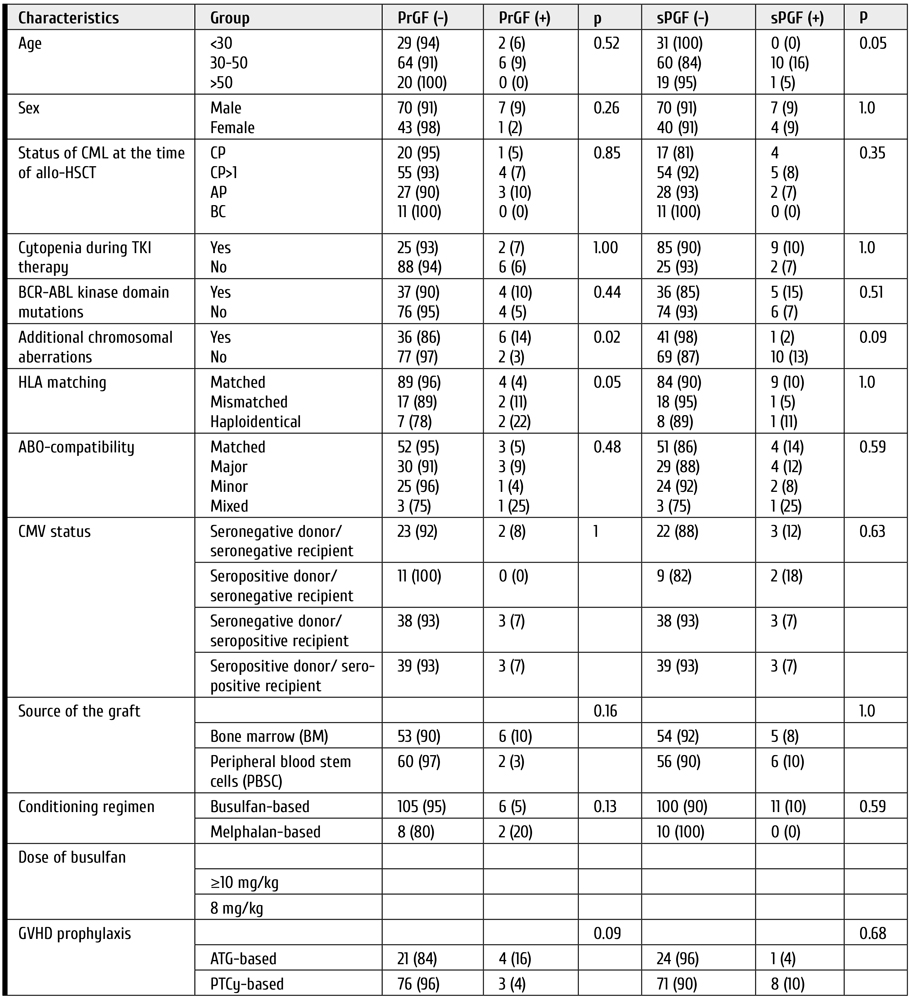
Clinical features and outcomes of graft failure and severe poor graft function
The median follow-up time after allo-HSCT was 68 days (range: 43-1792). All the patients with primary graft failure (PrGF) (n=8) were administered G-CSF, antimicrobial therapy and transfusion support. Two patients received donor lymphocyte infusions without any effect. The second allo-HSCT was performed in 4 cases. A total of 7 patients had lethal outcome (6, of infectious complications; 1, of relapse), whereas one patient is alive after the 2nd allo-HSCT (Fig. 4).

Figure 4. Treatment and outcomes of primary graft failure (PrGF) in CML patients after HSCT
Eleven patients exhibited severe poor graft function (sPGF) within median time of 21 (0-92) days after engraftment. Median length of sPGF was 52 days (range: 14-215). The median time of follow-up after allo-HSCT was 977 days (range: 45-2712).
Early sPGF with criterial cytopenia persisting after engraftment was diagnosed in 4 cases (36%), the remaining patients developed cytopenia after a period of normal graft function. A total of 3 cases of sPGF (27%) developed within 30 days after acute GVHD 2-3 grade (Fig. 5).

Figure 5. Timeline of severe poor graft function (SPGF) in a group of CML patients
All the patients with sPGF received antimicrobial therapy, transfusion support, and G-CSF in case of neutropenia. Other therapeutic options for sPGF therapy were: rituximab (n=4), the second allo-HSCT, or boost stem cell infusion (n=3); eltrombopag (n=1); supportive care (n=5), as seen from Fig. 4. Normal graft function was restored in 8 patients.
A total of 4 patients died. The causes of death were infectious complications (n=3) and late post-transplant relapse (n=1) (Fig. 6).
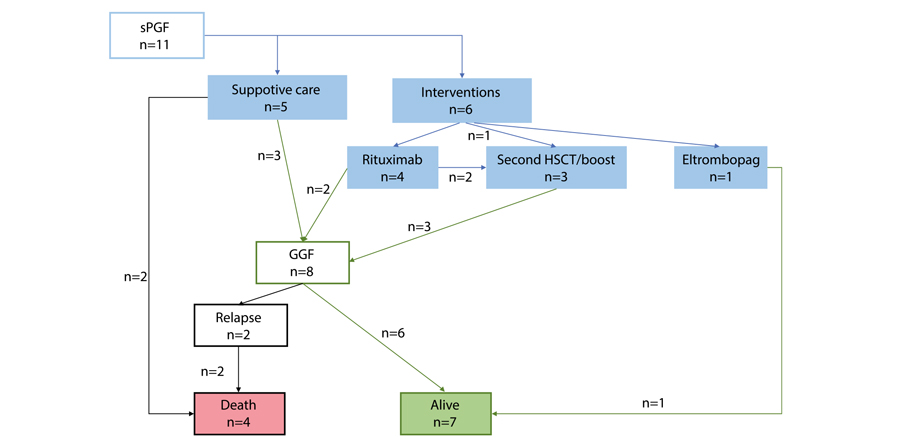
Figure 6. Treatment and outcomes of severe poor graft function (sPGF) in CML patients post-HSCT
Two cases of secondary graft failure occurred in about 3 months after allo-HSCT. Both patients died due to severe infection.
The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF as compared with those, who were free of these complications. Cumulative incidence of leukemia relapses was 31% (95% CI, 23-42), and 25% (95% CI, 4-87) in the patients with PrGF and engraftment (p=0.97), compared with 22% (95% CI, 3-54) and 32% (95% CI, 24-43) in the patients with sPGF and without sPGF (p=0.52), respectively.
Primary graft failure (PrGF) but not severe poor graft failure (sPGF) significantly increased non-relapse mortality during the first year after allo-HSCT. One-year NRM was 23% (95% CI, 15-32) in engrafted patients versus 71% (95% CI, 39-96) in the patients with PrGF (p<0.0001). Patients with and without sPGF had similar NRM: 20% (95% CI, 5-59) versus 26% (95% CI, 18-36) (p=0.74).
One-year OS was significantly lower in patients with PrGF: 13% (95% CI, 0.7-42) versus 64% (95% CI, 54-72) (p<0.0001) (Fig. 7). On the contrary, sPGF had no statistically significant influence on OS: 73% (95% CI, 37-90) versus 59% (95% CI, 49-69) (p=0.47).

Figure 7. Impact of primary graft failure (PrGF, A), and severe poor graft function (sPGF, B) on overall survival post-HSCT in CML patients
Discussion
In context of TKI therapy progress, the indications for allo-HSCT in CML are becoming more stringent, with respect both to selective TKI choice, relapse diagnostics, and improved transplant technologies [22]. In this regard, it becomes relevant to investigate the causes of allo-HSCT failure and to determine the risk factors for PrGF and sPGF in CML patients. While the factor of post-transplant relapse is discussed in most publications, the issues of PrGF and sPGF remain poorly reflected. Only few authors provided clear definitions and data on the incidence of these complications (mostly PrGF) in the patients with CML. At the same time, most studies of posttransplant graft failure syndromes show that the diagnosis of CML may be among risk factors of this complication. However, most previous studies concerned a heterogeneous range of diagnoses, e.g., acute leukemia, chronic myelo- and lymphoproliferative and non-malignant diseases. To our knowledge, the present work evaluates for the first time the incidence of both PrGF and PGF in a homogeneous cohort of CML patients.
According to our results, PrGF occurred in 7% of cases, thus being higher than in patients with acute leukemia as confirmed by other publications [10]. On the contrary, cumulative incidence of sPGF during the first year after allo-HSCT was 10%. This level is less than in general population of patients after allo-HSCT [15]. A prospective non-interventional study from the Chronic Malignancy Working Party of the EBMT also showed increased rate of graft dysfunction in CML patients after allo-HSCT. Impact of pre-transplant treatment with tyrosine kinase inhibitors of second generation on the allograft function due to myelotoxicity is still under discussion [23]. Presumably, the similar factors may contribute to the development of both PrGF and sPoGF.
We analyzed the data associated with characteristics of patients, donors, and the HSCT procedure. Due to small number of cases in the target groups, only univariate analysis was performed. In contrast to many studies, conditioning regimen, the source and cellularity of the graft, CMV status of the donor and the patient, ABO incompatibility did not show any statistical significance of the disease status, although it is proved an important characteristic for the prognosis of primary graft failure and poor graft function [10, 11, 24, 25, 26, 27, 28, 29, 30].
Nevertheless, it was the presence of ACA that showed statistical significance for PrGF. This may suggest insufficient control of the underlying disease to be among the main causes of any type of graft dysfunction. However, no association between post-transplant relapse and sPGF was noted in our study. The disease recurrence after resolution of graft failure remains an important cause of treatment failure. Contribution of the underlying disease to development of PrGF and sPGF needs to be investigated in future.
HLA incompatibility was another factor for PrGF in univariate analysis. The importance of this characteristic for HSC engraftment is well known [13, 15, 30]. Haploidentical HSCTs in this analysis showed larger proportion of PrGF and sPGF, but this result needs further proofs, as our group was small and mostly retrospective.
The question still exists if the intensity of conditioning regimen may contribute to insufficient hematopoietic reconstitution after allo-HSCT. Impairment of bone marrow microenvironment exposed to high doses of alkylating agents may be one of the possible pathogenic pathways [13, 31]. Nevertheless, our study did not show significant influence of conditioning intensity upon the clinical outcomes.
Natural history of the patients who developed graft failure and poor graft function was of particular interest in this retrospective study. Despite various interventions, primary graft failure is still associated with poor outcomes and death, mostly, due to infectious complications.
Survival and NRM analysis showed that, despite the rare occurrence, PrGF and sPGF are life-threatening and resource-consuming problems. Both PrGF and sPGF need aggressive approach in order to improve outcomes of allo- HSCT. Intensive interventions might be a rescue for, at least, a part of the patients and lead to prolonged survival. Stimulation of residual HSCs by TPO agonists using in the setting of persistent cytopenia after HSCT by several groups might be a promising strategy, although influence of TPO agonists on the leukemic stem cells and risk of relapse is debated. Early employment of a CD34+-selected stem cell boost, or a second allogeneic HSCT to restore an effective haematopoiesis might also be a life-saving option. Identification of patients at high risk for these complications and development strategies for early intervention might be in scope of further investigation.
Conclusion
Both PrGF and sPGF are significant life-threatening problems in allo-HSCT. Specifically, PrGF but not severe poor graft failure (sPGF) significantly increased non-relapse mortality during the first year after allo-HSCT. Meanwhile, the incidence of post-transplant relapses did not differ in the CML patients exhibiting primary graft failure or severe poor graft function. Identification of risk factors for these complications can improve the results of this treatment, by planning HSCT technology, to minimize them and modify approaches to post-transplant therapy.
Conflict of interest
None declared.
References
- Afanasyev BV, Zubarovskaya LS. Role of hematopoietic stem cell transplantation in therapy of adult patients with acute leukemias. Oncohematology. 2006;1(1-2): 70-85. (In Russian).
- Lübking A, Dreimane A, Sandin F et al. Allogeneic stem cell transplantation for chronic myeloid leukemia in the TKI era: population-based data from the Swedish CML registry. Bone Marrow Transplant. 2019;54, 1764-1774. doi: 10.1038/s41409-019-0513-5
- Barrett AJ, Ito S. The role of stem cell transplantation for chronic myelogenous leukemia in the 21st century. Blood. 2015;125(21):3230-3235. doi: 10.1182/blood-2014-10-567784
- Lyubimova LS, Kuzmina LA, E.S.Urnova ES, Zhelnova ES, Anukhina MV, Mendeleyeva LP, et al. Early HLA-identical bone marrow transplantation during chronic myeloid leukemia chronic phase vs. long-term tyrosine kinase inhibitor therapy? Gematologyia i Transfusiologiya. 2012; 57 (3): 6-10. (In Russian).
- Morozova EV, Vlasova YI, Barabanshikova MV, Afanaseva KS, Iurovskaia KS, Gindina TL, Barchatov IM, Alyanskiy AL, Bakin EA, Bondarenko SN, Moiseev IS, Zubarovskaya LS, Afanasyev BV. Allogeneic haematopoietic stem cell transplantation with reduced-intensity conditioning in chronic myeloid leukaemia. Russian Journal of Hematology and Transfusiology. 2020; 65(4): 386-402. (In Russian.). doi: 10.35754/0234-5730-2020-65-4-386-402
- Boehm A, Walcherberger B, Sperr WR, Woehrer S, Dieckmann K, Rosenmayr A, et al. Improved outcome in patients with chronic myelogenous leukemia after allogeneic hematopoietic stem cell transplantation over the past 25 years: A single-center experience. Biol Blood Marrow Transplant. 2011; 17: 133-140. doi: 10.1016/j.bbmt.2010.06.019
- Kolb HJ. Graft-versus-leukemia effects of transplantation and donor lymphocytes. Blood 2008; 112 (12): 4371-4383.
doi: 10.1182/blood-2008-03-077974 - Klyuchnikov E, Kröger N, Brummendorf TH et al. Current status and perspectives of tyrosine kinase inhibitor treatment in the posttransplant period in patients with chronic myelogenous leukemia (CML). Biol Blood Marrow Transplant. 2010; 16 (3): 301-310.
doi: 10.1016/j.bbmt.2009.08.019 - Bonifacio M, Stagno F, Scaffidi L, Krampera M, Raimondo FD. Management of chronic myeloid leukemia in advanced phase. Front Oncol. 2019; Oct 25; 9:1132. doi: 10.3389/fonc.2019.01132
- Olsson RF, Logan BR, Chaudhury S, Zhu X, Akpek G, Bolwell BJ, et al. Primary graft failure after myeloablative allogeneic hematopoietic cell transplantation for hematologic malignancies. Leukemia. 2015; 29(8), 1754-1762. doi: 10.1038/leu.2015.75
- Olsson RF, Berggren DM, Ringden O, Mattsson J, Remberger M. Graft failure in reduced intensity conditioning allogeneic hematopoietic stem cell transplantation. Blood. 2013; 122 (21): 4559. doi: 10.1182/blood.V122.21.4559.4559
- Locatelli F, Lucarelli B, Merli P. Current and future approaches to treat graft failure after allogeneic hematopoietic stem cell transplantation. Expert Opinion Pharmacother. 2014;15(1): 23-36. doi: 10.1517/14656566.2014.852537
- Xiao Y, Song J, Jiang Z, Li Y, Gao Y, Xu W, Lu Z, Wang Y, Xiao H. Risk-factor analysis of poor graft function after allogeneic hematopoietic stem cell transplantation. Int J Med Sci. 2014; 11(6):652-657. doi: 10.7150/ijms.6337
- Marotta S, Marano L, Ricci P, Cacace F, Frieri C, Simeone L, Trastulli F, Vitiello S, Cardano F, Pane F, Risitano AM. Eltrombopag for post-transplant cytopenias due to poor graft function. Bone Marrow Transplant. 2019; 54(8):1346-1353. doi: 10.1038/s41409-019-0442-3
- Rudakova TA, Kulagin AD, Klimova OU, Golubovskaya IK, Darskaya EI, Bykova TA, Smirnova AG, Morozova EV, Bondarenko SN, Moiseev IS, et al. Severe poor graft function after allogeneic hematopoietic stem cell transplantation in adult patients: Incidence, risk factors, and outcomes. Clinical Oncohematology. 2019;12(3):309-318 (In Russ). doi: 10.21320/2500-2139-2019-12-3-309-318
- Turkina AG, Zaritsky AYu, Chelysheva EYu. et al. Clinical recommendations for the diagnosis and treatment of chronic myelogenous leukemia. Clinical Oncohematology. 2017;10(3):294-316. (In Russian). doi: 10.21320/2500-2139-2017-10-3-294-316
- Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, Cervantes F, Clark RE, Cortes JE, Guilhot F, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122:872-884.
doi: 10.1182/blood-2013-05-501569 - McGowan-Jordan J, Simons A, Schmid M. International Standing Committee on Human Cytogenomic Nomenclature, 2016.
doi: 10.1159/isbn.978-3-318-06861-0 - Gabert J, Beillard E, van der Velden V., et al. Standardization and quality control studies of ‘real-time’ quantitative reverse transcriptase polymerase chain reaction of fusion gene transcripts for residual disease detection in leukemia- A Europe Against Cancer Program. Leukemia. 2003.17: 2318-2357. doi: 10.1038/sj.leu.2403135
- Valcárcel D, Sureda A. Graft Failure. In: Carreras E, Dufour C, Mohty M, Kröger N, editors. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies [Internet]. 7th ed. Cham (CH): Springer; 2019. Chapter 41. PMID: 32091792. https://www.ncbi.nlm.nih.gov/books/NBK553942/. doi: 10.1007/978-3-030-02278-5
- Gratwohl A. The EBMT risk score. Bone Marrow Transplantation. 2012;47:749-56. doi: 10.1038/bmt.2011.110
- Craddock CF. We do still transplant CML, don’t we? Hematology Am Soc Hematol Educ Program. 2018 (1): 177-184.
https://doi.org/10.1182/asheducation-2018.1.177 - Masouridi-Levrat S, Olavarria E, Iacobelli S, Aljurf M, Morozova E, Niittyvuopio R, Sengeloev H, Reményi P, Helbig G, Browne P, et al. Outcomes and toxicity of allogeneic hematopoietic cell transplantation in chronic myeloid leukemia patients previously treated with second-generation tyrosine kinase inhibitors: a prospective non-interventional study from the Chronic Malignancy Working Party of the EBMT. Bone Marrow Transplant. 2022; 57(1):23-30. doi: 10.1038/s41409-021-01472-x
- Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn BM, Mattsson J, Ringden O. Graft failure in the modern era of allogeneic hematopoietic SCT [published correction appears in Bone Marrow Transplant. 2013 Apr; 48(4):616]. Bone Marrow Transplant. 2013;48(4):537-543. doi: 10.1038/bmt.2012.239
- Moiseev IS, Morozova EV, Vlasova YY, et al. Interim results of the randomized trial of post-transplanation cyclophosphamide versus rabbit ATG for graft-versus-host disease prophylaxis in chronic myeloproliferative neoplasms and myelodysplastic syndrome. Cell Ther Transplant. 2016; 5(3):62-63. doi: 10.18620/ctt-1866-8836-2016-5-3-49-50
- Hallemeier C. Letter to the editor. Re: High rate of graft failure in 25 patients with chronic myelogenous leukemia conditioned with a reduced-intensity regimen of 550 cGy total body irradiation and cyclophosphamide for unrelated donor transplantation. Biol Blood Marrow Transplant. 2004; 10:726-727. doi: 10.1016/j.bbmt.2004.07.001
- Khoury H, Adkins, Brown RH, Pence, Vij R, Goodnough LT, et al. Low incidence of transplantation-related acute complications in patients with chronic myeloid leukemia undergoing aiiogeneic stem cell transplantation with a low-dose (550 cGy) total body irradiation conditioning regimen. Biol Blood Marrow Transplant. 2001; 7(6):352-358. doi: 10.1016/S1083-8791(01)80006-9
- Khoury HJ, Kukreja M, Goldman JM, Wang T, Halter J, Arora M, et al. Prognostic factors for outcomes in allogeneic transplantation for CML in the imatinib era: a CIBMTR analysis. Bone Marrow Transplant. 2012; 47, 810-816. doi: 10.1038/bmt.2011.194
- Radujkovic A, Dietrich S, Blok HJ, Nagler A, Ayuk F, Finke J, et al. Allogeneic stem cell transplantation for blast crisis chronic myeloid leukemia in the era of tyrosine kinase inhibitors: A retrospective study by the EBMT Chronic Malignancies Working Party. Biol Blood Marrow Transplant. 2019; 25(10): 2008-2016. doi: 10.1016/j.bbmt.2019.06.028
- Kuzmich YV, Alyanskiy AI, Ivanova NY, Vitrischak AA, Vladovskaya MD, Morozova YV, Bondarenko SN, Semenova YV, Zubarovskaya LS, Afanasyev BV. Analysis of the results of allogeneic hematopoietic stem cell transplantation depending on HLA matching of the unrelated donor/recipient pair. Oncohematology. 2014; 9(3):25-31. (In Russian). doi: 10.17650/1818-8346-2014-9-3-25-31
- Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, et al. CD34 selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014; 20(9): 1440-1443. doi: 10.1016/j.bbmt.2014.05.016
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "10" ["~SORT"]=> string(2) "10" ["CODE"]=> string(100) "pre-i-posttransplantatsionnye-faktory-assotsiirovannye-s-pervichnoy-nedostatochnostyu-i-tyazheloy-di" ["~CODE"]=> string(100) "pre-i-posttransplantatsionnye-faktory-assotsiirovannye-s-pervichnoy-nedostatochnostyu-i-tyazheloy-di" ["EXTERNAL_ID"]=> string(4) "2051" ["~EXTERNAL_ID"]=> string(4) "2051" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(607) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозеPre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(6014) "<p style="text-align: justify;">Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев. </p> <h3>Результаты</h3> <p style="text-align: justify;">Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.</p> <h3>Выводы</h3> <p style="text-align: justify;">Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.</p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_META_TITLE"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_META_KEYWORDS"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_META_DESCRIPTION"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_PICTURE_FILE_ALT"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_PICTURE_FILE_TITLE"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_PICTURE_FILE_NAME"]=> string(100) "pre-i-posttransplantatsionnye-faktory-assotsiirovannye-s-pervichnoy-nedostatochnostyu-i-tyazheloy-di" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(415) "Пре- и посттрансплантационные факторы, ассоциированные с первичной недостаточностью и тяжелой дисфункцией трансплантата после аллогенной трансплантации гемопоэтических стволовых клеток при хроническом миелоидном лейкозе" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(100) "pre-i-posttransplantatsionnye-faktory-assotsiirovannye-s-pervichnoy-nedostatochnostyu-i-tyazheloy-di" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(100) "pre-i-posttransplantatsionnye-faktory-assotsiirovannye-s-pervichnoy-nedostatochnostyu-i-tyazheloy-di" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(100) "pre-i-posttransplantatsionnye-faktory-assotsiirovannye-s-pervichnoy-nedostatochnostyu-i-tyazheloy-di" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "207" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28521" ["VALUE"]=> string(22) "03/09/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/09/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28522" ["VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28523" ["VALUE"]=> array(2) { ["TEXT"]=> string(384) "<p>Елена В. Морозова, Татьяна А. Рудакова, Юлия Ю. Власова, Мария В. Барабанщикова, Татьяна Л. Гиндина, Александр Л. Алянский, Мария Д. Владовская, Иван С. Моисеев, Людмила С. Зубаровская, Александр Д. Кулагин</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(372) "
Елена В. Морозова, Татьяна А. Рудакова, Юлия Ю. Власова, Мария В. Барабанщикова, Татьяна Л. Гиндина, Александр Л. Алянский, Мария Д. Владовская, Иван С. Моисеев, Людмила С. Зубаровская, Александр Д. Кулагин
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28524" ["VALUE"]=> array(2) { ["TEXT"]=> string(373) "<p>НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(361) "НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_RU"]=> array(36) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28525" ["VALUE"]=> array(2) { ["TEXT"]=> string(6014) "<p style="text-align: justify;">Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев. </p> <h3>Результаты</h3> <p style="text-align: justify;">Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.</p> <h3>Выводы</h3> <p style="text-align: justify;">Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(5856) "Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.
Пациенты и методы
Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев.
Результаты
Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.
Выводы
Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.
Ключевые слова
Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28518" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-13-23" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-13-23" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28526" ["VALUE"]=> array(2) { ["TEXT"]=> string(234) "<p>Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina, Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(222) "Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina, Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28527" ["VALUE"]=> array(2) { ["TEXT"]=> string(817) "<p>RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia<br> Phone: +7 (911) 927-82-29<br> E-mail: dr_morozova@mail.ru</p><br> <p><b>Citation:</b> Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(727) "RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia
Correspondence:
Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (911) 927-82-29
E-mail: dr_morozova@mail.ru
Citation: Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28528" ["VALUE"]=> array(2) { ["TEXT"]=> string(3228) "<p style="text-align: justify;"> Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients. </p> <h3>Patients and methods</h3> <p style="text-align: justify;"> We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases. </p> <h3>Results</h3> <p style="text-align: justify;"> Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA <i>versus </i>3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% <i>versus</i> 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF. </p> <h3>Conclusions</h3> <p style="text-align: justify;"> Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies. </p> <h2>Keywords</h2> <p style="text-align: justify;"> Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3046) "Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
Patients and methods
We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases.
Results
Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA versus 3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% versus 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF.
Conclusions
Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies.
Keywords
Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28519" ["VALUE"]=> string(192) "Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(192) "Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28520" ["VALUE"]=> string(4) "2765" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2765" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28529" ["VALUE"]=> string(4) "2768" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2768" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(10) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28526" ["VALUE"]=> array(2) { ["TEXT"]=> string(234) "<p>Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina, Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(222) "Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina, Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(222) "Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina, Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28528" ["VALUE"]=> array(2) { ["TEXT"]=> string(3228) "<p style="text-align: justify;"> Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients. </p> <h3>Patients and methods</h3> <p style="text-align: justify;"> We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases. </p> <h3>Results</h3> <p style="text-align: justify;"> Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA <i>versus </i>3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% <i>versus</i> 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF. </p> <h3>Conclusions</h3> <p style="text-align: justify;"> Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies. </p> <h2>Keywords</h2> <p style="text-align: justify;"> Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3046) "Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
Patients and methods
We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases.
Results
Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA versus 3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% versus 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF.
Conclusions
Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies.
Keywords
Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(3046) "Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
Patients and methods
We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases.
Results
Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA versus 3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% versus 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF.
Conclusions
Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies.
Keywords
Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28518" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-13-23" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-13-23" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-13-23" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28519" ["VALUE"]=> string(192) "Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(192) "Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(192) "Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28527" ["VALUE"]=> array(2) { ["TEXT"]=> string(817) "<p>RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia<br> Phone: +7 (911) 927-82-29<br> E-mail: dr_morozova@mail.ru</p><br> <p><b>Citation:</b> Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(727) "RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia
Correspondence:
Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (911) 927-82-29
E-mail: dr_morozova@mail.ru
Citation: Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(727) "RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia
Correspondence:
Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (911) 927-82-29
E-mail: dr_morozova@mail.ru
Citation: Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28523" ["VALUE"]=> array(2) { ["TEXT"]=> string(384) "<p>Елена В. Морозова, Татьяна А. Рудакова, Юлия Ю. Власова, Мария В. Барабанщикова, Татьяна Л. Гиндина, Александр Л. Алянский, Мария Д. Владовская, Иван С. Моисеев, Людмила С. Зубаровская, Александр Д. Кулагин</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(372) "Елена В. Морозова, Татьяна А. Рудакова, Юлия Ю. Власова, Мария В. Барабанщикова, Татьяна Л. Гиндина, Александр Л. Алянский, Мария Д. Владовская, Иван С. Моисеев, Людмила С. Зубаровская, Александр Д. Кулагин
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(372) "Елена В. Морозова, Татьяна А. Рудакова, Юлия Ю. Власова, Мария В. Барабанщикова, Татьяна Л. Гиндина, Александр Л. Алянский, Мария Д. Владовская, Иван С. Моисеев, Людмила С. Зубаровская, Александр Д. Кулагин
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28521" ["VALUE"]=> string(22) "03/09/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/09/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "03/09/2022 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28522" ["VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "03/18/2022 12:00:00 am" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28525" ["VALUE"]=> array(2) { ["TEXT"]=> string(6014) "<p style="text-align: justify;">Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.</p> <h3>Пациенты и методы</h3> <p style="text-align: justify;">Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев. </p> <h3>Результаты</h3> <p style="text-align: justify;">Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.</p> <h3>Выводы</h3> <p style="text-align: justify;">Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(5856) "Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.
Пациенты и методы
Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев.
Результаты
Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.
Выводы
Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.
Ключевые слова
Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(5856) "Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.
Пациенты и методы
Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев.
Результаты
Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.
Выводы
Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.
Ключевые слова
Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28524" ["VALUE"]=> array(2) { ["TEXT"]=> string(373) "<p>НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(361) "НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(361) "НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
" } } } [4]=> array(49) { ["IBLOCK_SECTION_ID"]=> string(3) "207" ["~IBLOCK_SECTION_ID"]=> string(3) "207" ["ID"]=> string(4) "2054" ["~ID"]=> string(4) "2054" ["IBLOCK_ID"]=> string(1) "2" ["~IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["~NAME"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["ACTIVE_FROM"]=> NULL ["~ACTIVE_FROM"]=> NULL ["TIMESTAMP_X"]=> string(22) "04/19/2022 11:34:59 am" ["~TIMESTAMP_X"]=> string(22) "04/19/2022 11:34:59 am" ["DETAIL_PAGE_URL"]=> string(148) "/en/archive/tom-11-nomer-1/klinicheskie-raboty/iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p/" ["~DETAIL_PAGE_URL"]=> string(148) "/en/archive/tom-11-nomer-1/klinicheskie-raboty/iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p/" ["LIST_PAGE_URL"]=> string(12) "/en/archive/" ["~LIST_PAGE_URL"]=> string(12) "/en/archive/" ["DETAIL_TEXT"]=> string(22008) "Introduction
Liver transplantation (LT) for hepatocellular carcinoma (HCC) has witnessed a historic change after the milestone article published by Mazzaferro et al. [1], who confirmed favorable outcomes for HCC patients similar to outcomes of LT for non-HCC indications. Since then, LT and its main option, the deceased-donor liver transplantation (DDLT) has become a well-established line of treatment with a highly curative profile for cirrhotic patients with HCC, but if only a liver graft is available.
The living-donor liver transplantation (LDLT) was introduced in order to reduce the organ shortage, due to expanding waiting lists for the patients awaiting liver transplant. In some countries, where the number of deceased donor is extremely small, the LDLT has been developed as an alternative treatment for the end-stage liver diseases, thus becoming an established treatment in HCC cases [2].
Nevertheless, recurrent HCC (rHCC) is still reported in up to 15% of cases following LT. HCC relapse is associated with dismal prognosis and, subsequently, LT failure in most instances [3]. Currently, LT for HCC has increased four-fold since early 2000s [4]. The impact of recurrent HCC is further enhanced by scarcity of liver grafts and fast expansion of LT waiting lists, whereas hepatic resection and other ablative modalities can offer up to 50% patient survival for HCC relapse [5].
Patient survival was shown to be better following LDLT for HCC compared to those transplanted from Deceased Donor (DD) [6, 7]. Many factors were held responsible for such results, including shorter time to transplant, better graft quality with shorter ischemia period.
Moreover, with the accumulation of cases, the impact of LDLT on the rHCC rates after LT has drawn attention of transplant community, since some reports showed higher incidence of rHCC following LDLT [8].
Many pathogenetic mechanisms were considered to explain these reports, including higher cytokine production in regenerating liver grafts and reduced time to transplant that could conceal aggressive tumor biology promoting the HCC recurrence [9-11]. These data were further analyzed to compare rHCC for patients transplanted from LDLT and DDLT source [12-15].
Hence, the aim of our single-center study was to compare overall and tumor-free survival among HCC patients subjected to liver transplantation from living donor (LDLT) versus liver transplant from deceased donor (DDLT).
Materials and methods
The study was started after obtaining the approval of Research Ethics Committee at our institution. All the patients were consented for the use of their clinical and pathological data for research purposes in anonymous manner, the patients were also informed that their decision to approve or disapprove the research consent will not influence their clinical management.
The cases of pediatric LT or liver retransplantation were excluded from this study. Finally, 136 patients diagnosed with HCC approved the research consent, being subsequently included in the study. Medical charts of the included patients were retrospectively reviewed. HCC was diagnosed by contrast-enhanced computed tomography (CT) and/or abdominal magnetic resonance imaging (MRI). The disease staging was based on chest CT, cranial CT, and technetium-99m bone scintigraphy, to exclude extra-hepatic disease. The following exclusion criteria were considered absolute contraindications for LT at our center:
• Failed or unfeasible downstaging of HCC originally beyond Milan, or UCSF transplant criteria, i.e., stable disease (SD), progressive disease (PD) according to modified RECIST criteria (16);
• Active extra-hepatic malignancies (excluding non-melanoma skin cancers);
• Untreatable advanced cardiopulmonary disease;
• Active infections e.g., active tuberculosis, uncontrollable sepsis;
• Unstable major psychiatric disorders;
• Disabling extensive intracranial neurological deficit;
• Substance abuse or active alcohol abuse over last 6 months;
• Documented medical non-compliance.
A total of 115 adult patients underwent LT for HCC at our institution between August 2006 and December 2019. LT was performed using either cadaveric, or living donor liver transplantation (LDLT). In LDLT setting, the donors were first- and second-degree relatives of respective patients.
Seventy-three patients conformed with Milan liver transplant criteria (MC) and, for the sake of comparison, they were divided into two groups as follows: Group A included forty-four HCC patients transplanted from living donors (LDLT); Group B consisted of twenty-nine HCC patients who received DDLT.
Fig. 1 illustrates the distribution of HCC patients with respect to decision for LT, and if the transplant was performed as LDLT or DDLT. The patients beyond Milan criteria, or those subjected to downstaging locoregional therapy were excluded from the study.

Figure 1. Flowchart of HCC patients enrolled during the study period
Details of the transplant procedure were documented; tumor characteristics were based on the pathological findings. HCC size, number of foci, tumor grade, and lymphatic invasion were diagnosed by an experienced pathologist. Demographic data, pre-transplant features, procedure-related variables, pathological findings were retrieved from the patient charts. Triple immunosuppression protocol was applied for the LT recipients including calcineurin inhibitor (CNI), glucocorticosteroids, and mycophenolate mofetil. Clinical and laboratory data were analyzed with t-test and Chi-square test. P-value of <0.05 was considered statistically significant. Kaplan-Meier curves were used to express survival outcomes, and statistical significance was determined by log-rank test. Overall and tumor-free survival were determined during the control contacts and examination of the patients.
Patient survival was calculated from the date of LT to the date of death or the date of the last follow-up for surviving patients. Graft survival was estimated as a death-censored graft survival. It was calculated from the date of transplantation to the date of irreversible graft failure signified by relisting of the patient on liver transplant waiting list, this method was used to avoid estimation of death with a functioning graft as a graft failure. Tumor-free survival was estimated from the date of transplant to the date of confirmed pathological evidence of recurrent HCC.
Results
Seventy-three patients underwent LT between August 2006 and December 2019 at our center for HCC which met MC. Table 1 is summarizing pre-transplant and pathological variables for these patients.
Table 1. Comparison of pre-transplant and pathological findings in LDLT and DDLT groups of the patients with hepatocellular carcinoma

Time to transplant ranged from 10 to 185 days, patients’ age, and time to transplant differed significantly between group A (living donors) and B (deceased donors), (P value, 0.002 and <0.001 respectively). On the other hand, pathological variables did not show significant difference between both groups.
The mean post-transplant follow-up for the studied patients was 46±33.3 months, ranging from 24.3 to 149.9 months. The overall 5-year patient survival, graft survival and tumor-free survival were 78.6%, 90.1% and 86.3% respectively. During the follow-up, a total of six patients manifested with rHCC (8.2%), i.e., four patients (9.1%) developed rHCC in group A, compared to two-cases (6.9%) of rHCC in group B patients, p value was 0.99. With respect to survival outcomes, LDLT group slightly differed from those who received DDLT. The overall patient survival was higher in Group A, at P=0.09 (log-rank test).
Conversely, tumor-free survival was only marginally better in group B, but it did not reach the significance level (P=0.6). On the other hand, graft survival was almost the same in both groups (P=0.99), as seen in Fig. 2 (A, B, C).

Figure 2. Comparisons for overall survival (A), tumor-free survival (B) and graft survival (C) between the groups A (LDLT) and B (DDLT) using the Kaplan-Meier approach
Discussion
There is a convincing evidence, that LT offers an excellent chance for cure of patients presenting with HCC, especially when their tumor burden is still within Milan criteria. The main concern regarding LT for HCC patients is the issue of liver graft availability and ethical costs to obtain it. Ethical concerns always overshadow the excellent results for LT in HCC patients, especially when allocation system favors HCC patients by the addition of 22 points [3, 4]. Consequently, more liver grafts are being allocated to HCC patients on the expense of patient suffering from liver insufficiency only. Furthermore, the use of LDLT to partially alleviate graft shortage is accompanied by inherent risk for healthy donor. Thus, outcomes of LT for HCC must be at optimal levels, to justify the ethical concerns encountered either in DDLT or LDLT settings. Hence, evaluation of clinical outcomes after LT for HCC in general, and comparative assessment of either LDLT or DDLT advantages over other options is quite important, especially in transplant centers where both LT modes are available.
DDLT is associated with long waiting times and consequently increased mortality and delisting rate while awaiting liver transplant. Hogen et al. [17], reported significantly higher waiting list mortality in UNOS regions with long waiting times compared to regions with short waiting times.
One of the main LDLT benefits is its ability to reduce the time to transplant and decrease the waiting list dropout. This is especially vital to the patients with HCC, to avoid tumor progression. Sandhu et al. [18], described a significantly shorter waiting time for LDLT compared to DDLT (3.1 vs 5.3 months respectively). Similarly, the current study reported significant data from the current study which showed 15% dropout rate for the patients originally presenting with HCC within Milan criteria. More than one third of this dropout rate was due to tumor progression. These patients underwent downstaging protocol using different locoregional neoadjuvant techniques.
The dropout rates vary considerably according to graft allocation policies. In the USA, there is a considerable variability of dropout rate based on the transplant waiting times. Mehta et al. [18], compared the dropout risk for HCC patients who received MELD exception points from 2005 and 2014. They described a significantly higher risk for dropout in UNOS regions with long transplant waiting times, the difference was three times higher than in the areas with short transplant waiting times (24% vs 8% dropout rate, respectively).
Few studies addressed the question of whether LDLT is associated with higher recurrence rate for HCC compared to DDLT, or not. One of the earliest reports on this issue (Lo et al.) described a significantly more common HCC recurrence at their LDLT arm (43 patients), compared to DDLT arm which included 17 patients. The study included heterogenous patient groups, i.e., corresponding the Milan or UCSF criteria, and beyond them. The cases subjected to downstaging locoregional therapy were not excluded from the study [12]. Similar findings were reported by Fischer et al. in their large cohort of patients, and they referred to different tumor characteristics, pretransplant locoregional therapies and short time to transplant as the key factors that explain the higher reported rHCC rates following LDLT [13].
On the other hand, Di Sandro et al., reported that LDLT had the same tumor-free survival compared to DDLT in the patients presenting within Milan transplant criteria, when tumor characteristics were kept unified during the study, and MC was recommended as the selection tool for further comparison of both LT modes [14]. Hence, this study reports similar findings, since LDLT was found to be insignificantly different from DDLT regarding tumor-free survival.
Such results were again confirmed by Sandhu et al., where the similar tumor-free survival rates were described in both LDLT and DDLT in a well-matched cohort of patients, especially for the tumor characteristics [15]. Ogawa et al., and Akamatsu et al., described comparable outcomes for both LDLT and DLT [19, 20]. Furthermore, Zhu et al., and Zhang et al. in their recently reported meta-analysis concluded that LDLT was not inferior to DDLT regarding overall or tumor-free survival [21, 22].
Conclusion
The results of the current study conclude that LDLT – while offering a slightly better overall survival – has insignificantly shorter tumor-free survival compared to DDLT. This is especially true, when the bias from different tumor characteristics was eliminated by studying a perfectly matched cohort of patients presenting with HCC within MC. Furthermore, LDLT group had a significantly shorter time to transplant compared to DDLT group. Consequently, the resulting decrease in dropout rate should be considered when comparing LLDT and DDLT options.
Conflict of interestsWith respect to the current study, the authors declare neither any conflict of interest, nor financial issues to be disclosed.
References
- Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. doi: 10.1056/NEJM199603143341104
- Akamatsu N, Sugawara Y, Kokudo N. Living donor liver transplantation for patients with hepatocellular carcinoma. Liver Cancer. 2014; 3: 108-118. doi: 10.1159/000343866
- Ioannou GN, Perkins JD, Carithers RL Jr. Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology. 2008; 134:1342-1351. doi: 10.1053/j.gastro.2008.02.013
- Massie AB, Caffo B, Gentry SE, Hall EC, Axelrod DA, Lentine KL, et al. MELD exceptions and rates of waiting list outcomes. Am J Transplant. 2011;11:2362-2371. doi: 10.1111/j.1600-6143.2011.03735.x
- Bodzin AS, Lunsford KE, Markovic D, Harlander-Locke MP, Busuttil RW, Agopian VG. Predicting mortality in patients developing recurrent hepatocellular carcinoma after liver transplantation: impact of treatment modality and recurrence characteristics. Ann Surg. 2017;266:118-125. doi: 10.1097/SLA.0000000000001894
- Gondolesi GE, Roayaie S, Muñoz L, Kim-Schluger L, Schiano T, Fishbein TM, et al. Adult living donor liver transplantation for patients with hepatocellular carcinoma: extending UNOS priority criteria. Ann Surg. 2004; 239:142-149. doi: 10.1097/01.sla.0000109022.32391.eb
- Kulik L, Abecassis M. Living donor liver transplantation for hepatocellular carcinoma. Gastroenterology. 2004; 127:S277-S282.
doi: 10.1053/j.gastro.2004.09.042 - Vakili K, Pomposelli JJ, Cheah YL, Akoad M, Lewis WD, Khettry U, et al. Living donor liver transplantation for hepatocellular carcinoma: increased recurrence but improved survival. Liver Transpl. 2009; 15:1861-1866. doi: 10.1002/lt.21940
- Yang ZF, Poon RT, Luo Y, Cheung CK, Ho DW, Lo CM, et al. Up-regulation of vascular endothelial growth factor (VEGF) in small-for-size liver grafts enhances macrophage activities through VEGF receptor 2-dependent pathway. J Immunol. 2004; 173:2507-2515.
doi: 10.4049/jimmunol.173.4.2507 - Shi JH, Huitfeldt HS, Suo ZH, Line PD. Growth of hepatocellular carcinoma in the regenerating liver. Liver Transpl. 2011;17:866-874.
doi: 10.1002/lt.22325 - Efimova EA, Glanemann M, Liu L, Schumacher G, Settmacher U, Jonas S, et al. Effects of human hepatocyte growth factor on the proliferation of human hepatocytes and hepatocellular carcinoma cell lines. Eur Surg Res. 2004; 36:300-307. doi: 10.1159/000079915
- Lo CM, Fan ST, Liu CL, Chan SC, Ng IO, Wong J. Living donor versus deceased donor liver transplantation for early irresectable hepatocellular carcinoma. Br J Surg. 2007; 94:78-86. doi: 10.1002/bjs.5528
- Fisher RA, Kulik LM, Freise CE, Lok AS, Shearon TH, Brown RS Jr, et al, for A2ALL Study Group. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant. 2007; 7: 1601-1608.
doi: 10.1111/j.1600-6143.2007.01802.x - Di Sandro S, Slim AO, Giacomoni A, Lauterio A, Mangoni I, Aseni P, et al. Living donor liver transplantation for hepatocellular carcinoma: long-term results compared with deceased donor liver transplantation. Transplant Proc. 2009; 41: 1283-1285.
doi: 10.1016/j.transproceed.2009.03.022 - Sandhu L, Sandroussi C, Guba M, Selzner M, Ghanekar A, Cattral MS, et al. Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: comparable survival and recurrence. Liver Transpl. 2012; 18(3):315-22.
doi: 10.1002/lt.22477 - Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52-60.
doi: 10.1055/s-0030-1247132 - Hogen R, Dinorcia J, Lo M, Nguyen B, Genyk Y, Sher L, Dhanireddy K. Long wait time regions for liver transplantation for HCC have a higher cumulative incidence of death. [abstract]. Am J Transplant. 2017; 17 (suppl 3).
- Mehta N, Dodge JL, Hirose R, Roberts JP, Yao FY. Increasing liver transplantation wait-list dropout for hepatocellular carcinoma with widening geographical disparities: implications for organ allocation. Liver Transpl. 2018; 24(10):1346-1356. doi: 10.1002/lt.25317
- Ogawa K, Takada Y. Living vs. deceased-donor liver transplantation for patients with hepatocellular carcinoma. Transl Gastroenterol Hepatol. 2016;1:35. doi: 10.21037/tgh.2016.04.03. eCollection 2016
- Akamatsu N, Sugawara Y, Kokudo N. Living-donor vs deceased-donor liver transplantation for patients with hepatocellular carcinoma. World J Hepatol. 2014; 6(9):626-631. doi: 10.4254/wjh.v6.i9.626
- Zhu B, Wang J, Li H, Chen X, Zeng Y. Living or deceased organ donors in liver transplantation for hepatocellular carcinoma: a systematic review and meta-analysis. HPB (Oxford). 2019; 21(2):133-147. doi: 10.1016/j.hpb.2018.11.004
- Zhang HM, Shi YX, Sun LY, Zhu ZJ. Hepatocellular carcinoma recurrence in living and deceased donor liver transplantation: a systematic review and meta-analysis. Chin Med J. 2019; 132(13):1599-1609. doi: 10.1097/CM9.0000000000000287
" ["~DETAIL_TEXT"]=> string(22008) "
Introduction
Liver transplantation (LT) for hepatocellular carcinoma (HCC) has witnessed a historic change after the milestone article published by Mazzaferro et al. [1], who confirmed favorable outcomes for HCC patients similar to outcomes of LT for non-HCC indications. Since then, LT and its main option, the deceased-donor liver transplantation (DDLT) has become a well-established line of treatment with a highly curative profile for cirrhotic patients with HCC, but if only a liver graft is available.
The living-donor liver transplantation (LDLT) was introduced in order to reduce the organ shortage, due to expanding waiting lists for the patients awaiting liver transplant. In some countries, where the number of deceased donor is extremely small, the LDLT has been developed as an alternative treatment for the end-stage liver diseases, thus becoming an established treatment in HCC cases [2].
Nevertheless, recurrent HCC (rHCC) is still reported in up to 15% of cases following LT. HCC relapse is associated with dismal prognosis and, subsequently, LT failure in most instances [3]. Currently, LT for HCC has increased four-fold since early 2000s [4]. The impact of recurrent HCC is further enhanced by scarcity of liver grafts and fast expansion of LT waiting lists, whereas hepatic resection and other ablative modalities can offer up to 50% patient survival for HCC relapse [5].
Patient survival was shown to be better following LDLT for HCC compared to those transplanted from Deceased Donor (DD) [6, 7]. Many factors were held responsible for such results, including shorter time to transplant, better graft quality with shorter ischemia period.
Moreover, with the accumulation of cases, the impact of LDLT on the rHCC rates after LT has drawn attention of transplant community, since some reports showed higher incidence of rHCC following LDLT [8].
Many pathogenetic mechanisms were considered to explain these reports, including higher cytokine production in regenerating liver grafts and reduced time to transplant that could conceal aggressive tumor biology promoting the HCC recurrence [9-11]. These data were further analyzed to compare rHCC for patients transplanted from LDLT and DDLT source [12-15].
Hence, the aim of our single-center study was to compare overall and tumor-free survival among HCC patients subjected to liver transplantation from living donor (LDLT) versus liver transplant from deceased donor (DDLT).
Materials and methods
The study was started after obtaining the approval of Research Ethics Committee at our institution. All the patients were consented for the use of their clinical and pathological data for research purposes in anonymous manner, the patients were also informed that their decision to approve or disapprove the research consent will not influence their clinical management.
The cases of pediatric LT or liver retransplantation were excluded from this study. Finally, 136 patients diagnosed with HCC approved the research consent, being subsequently included in the study. Medical charts of the included patients were retrospectively reviewed. HCC was diagnosed by contrast-enhanced computed tomography (CT) and/or abdominal magnetic resonance imaging (MRI). The disease staging was based on chest CT, cranial CT, and technetium-99m bone scintigraphy, to exclude extra-hepatic disease. The following exclusion criteria were considered absolute contraindications for LT at our center:
• Failed or unfeasible downstaging of HCC originally beyond Milan, or UCSF transplant criteria, i.e., stable disease (SD), progressive disease (PD) according to modified RECIST criteria (16);
• Active extra-hepatic malignancies (excluding non-melanoma skin cancers);
• Untreatable advanced cardiopulmonary disease;
• Active infections e.g., active tuberculosis, uncontrollable sepsis;
• Unstable major psychiatric disorders;
• Disabling extensive intracranial neurological deficit;
• Substance abuse or active alcohol abuse over last 6 months;
• Documented medical non-compliance.
A total of 115 adult patients underwent LT for HCC at our institution between August 2006 and December 2019. LT was performed using either cadaveric, or living donor liver transplantation (LDLT). In LDLT setting, the donors were first- and second-degree relatives of respective patients.
Seventy-three patients conformed with Milan liver transplant criteria (MC) and, for the sake of comparison, they were divided into two groups as follows: Group A included forty-four HCC patients transplanted from living donors (LDLT); Group B consisted of twenty-nine HCC patients who received DDLT.
Fig. 1 illustrates the distribution of HCC patients with respect to decision for LT, and if the transplant was performed as LDLT or DDLT. The patients beyond Milan criteria, or those subjected to downstaging locoregional therapy were excluded from the study.

Figure 1. Flowchart of HCC patients enrolled during the study period
Details of the transplant procedure were documented; tumor characteristics were based on the pathological findings. HCC size, number of foci, tumor grade, and lymphatic invasion were diagnosed by an experienced pathologist. Demographic data, pre-transplant features, procedure-related variables, pathological findings were retrieved from the patient charts. Triple immunosuppression protocol was applied for the LT recipients including calcineurin inhibitor (CNI), glucocorticosteroids, and mycophenolate mofetil. Clinical and laboratory data were analyzed with t-test and Chi-square test. P-value of <0.05 was considered statistically significant. Kaplan-Meier curves were used to express survival outcomes, and statistical significance was determined by log-rank test. Overall and tumor-free survival were determined during the control contacts and examination of the patients.
Patient survival was calculated from the date of LT to the date of death or the date of the last follow-up for surviving patients. Graft survival was estimated as a death-censored graft survival. It was calculated from the date of transplantation to the date of irreversible graft failure signified by relisting of the patient on liver transplant waiting list, this method was used to avoid estimation of death with a functioning graft as a graft failure. Tumor-free survival was estimated from the date of transplant to the date of confirmed pathological evidence of recurrent HCC.
Results
Seventy-three patients underwent LT between August 2006 and December 2019 at our center for HCC which met MC. Table 1 is summarizing pre-transplant and pathological variables for these patients.
Table 1. Comparison of pre-transplant and pathological findings in LDLT and DDLT groups of the patients with hepatocellular carcinoma

Time to transplant ranged from 10 to 185 days, patients’ age, and time to transplant differed significantly between group A (living donors) and B (deceased donors), (P value, 0.002 and <0.001 respectively). On the other hand, pathological variables did not show significant difference between both groups.
The mean post-transplant follow-up for the studied patients was 46±33.3 months, ranging from 24.3 to 149.9 months. The overall 5-year patient survival, graft survival and tumor-free survival were 78.6%, 90.1% and 86.3% respectively. During the follow-up, a total of six patients manifested with rHCC (8.2%), i.e., four patients (9.1%) developed rHCC in group A, compared to two-cases (6.9%) of rHCC in group B patients, p value was 0.99. With respect to survival outcomes, LDLT group slightly differed from those who received DDLT. The overall patient survival was higher in Group A, at P=0.09 (log-rank test).
Conversely, tumor-free survival was only marginally better in group B, but it did not reach the significance level (P=0.6). On the other hand, graft survival was almost the same in both groups (P=0.99), as seen in Fig. 2 (A, B, C).

Figure 2. Comparisons for overall survival (A), tumor-free survival (B) and graft survival (C) between the groups A (LDLT) and B (DDLT) using the Kaplan-Meier approach
Discussion
There is a convincing evidence, that LT offers an excellent chance for cure of patients presenting with HCC, especially when their tumor burden is still within Milan criteria. The main concern regarding LT for HCC patients is the issue of liver graft availability and ethical costs to obtain it. Ethical concerns always overshadow the excellent results for LT in HCC patients, especially when allocation system favors HCC patients by the addition of 22 points [3, 4]. Consequently, more liver grafts are being allocated to HCC patients on the expense of patient suffering from liver insufficiency only. Furthermore, the use of LDLT to partially alleviate graft shortage is accompanied by inherent risk for healthy donor. Thus, outcomes of LT for HCC must be at optimal levels, to justify the ethical concerns encountered either in DDLT or LDLT settings. Hence, evaluation of clinical outcomes after LT for HCC in general, and comparative assessment of either LDLT or DDLT advantages over other options is quite important, especially in transplant centers where both LT modes are available.
DDLT is associated with long waiting times and consequently increased mortality and delisting rate while awaiting liver transplant. Hogen et al. [17], reported significantly higher waiting list mortality in UNOS regions with long waiting times compared to regions with short waiting times.
One of the main LDLT benefits is its ability to reduce the time to transplant and decrease the waiting list dropout. This is especially vital to the patients with HCC, to avoid tumor progression. Sandhu et al. [18], described a significantly shorter waiting time for LDLT compared to DDLT (3.1 vs 5.3 months respectively). Similarly, the current study reported significant data from the current study which showed 15% dropout rate for the patients originally presenting with HCC within Milan criteria. More than one third of this dropout rate was due to tumor progression. These patients underwent downstaging protocol using different locoregional neoadjuvant techniques.
The dropout rates vary considerably according to graft allocation policies. In the USA, there is a considerable variability of dropout rate based on the transplant waiting times. Mehta et al. [18], compared the dropout risk for HCC patients who received MELD exception points from 2005 and 2014. They described a significantly higher risk for dropout in UNOS regions with long transplant waiting times, the difference was three times higher than in the areas with short transplant waiting times (24% vs 8% dropout rate, respectively).
Few studies addressed the question of whether LDLT is associated with higher recurrence rate for HCC compared to DDLT, or not. One of the earliest reports on this issue (Lo et al.) described a significantly more common HCC recurrence at their LDLT arm (43 patients), compared to DDLT arm which included 17 patients. The study included heterogenous patient groups, i.e., corresponding the Milan or UCSF criteria, and beyond them. The cases subjected to downstaging locoregional therapy were not excluded from the study [12]. Similar findings were reported by Fischer et al. in their large cohort of patients, and they referred to different tumor characteristics, pretransplant locoregional therapies and short time to transplant as the key factors that explain the higher reported rHCC rates following LDLT [13].
On the other hand, Di Sandro et al., reported that LDLT had the same tumor-free survival compared to DDLT in the patients presenting within Milan transplant criteria, when tumor characteristics were kept unified during the study, and MC was recommended as the selection tool for further comparison of both LT modes [14]. Hence, this study reports similar findings, since LDLT was found to be insignificantly different from DDLT regarding tumor-free survival.
Such results were again confirmed by Sandhu et al., where the similar tumor-free survival rates were described in both LDLT and DDLT in a well-matched cohort of patients, especially for the tumor characteristics [15]. Ogawa et al., and Akamatsu et al., described comparable outcomes for both LDLT and DLT [19, 20]. Furthermore, Zhu et al., and Zhang et al. in their recently reported meta-analysis concluded that LDLT was not inferior to DDLT regarding overall or tumor-free survival [21, 22].
Conclusion
The results of the current study conclude that LDLT – while offering a slightly better overall survival – has insignificantly shorter tumor-free survival compared to DDLT. This is especially true, when the bias from different tumor characteristics was eliminated by studying a perfectly matched cohort of patients presenting with HCC within MC. Furthermore, LDLT group had a significantly shorter time to transplant compared to DDLT group. Consequently, the resulting decrease in dropout rate should be considered when comparing LLDT and DDLT options.
Conflict of interestsWith respect to the current study, the authors declare neither any conflict of interest, nor financial issues to be disclosed.
References
- Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. doi: 10.1056/NEJM199603143341104
- Akamatsu N, Sugawara Y, Kokudo N. Living donor liver transplantation for patients with hepatocellular carcinoma. Liver Cancer. 2014; 3: 108-118. doi: 10.1159/000343866
- Ioannou GN, Perkins JD, Carithers RL Jr. Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology. 2008; 134:1342-1351. doi: 10.1053/j.gastro.2008.02.013
- Massie AB, Caffo B, Gentry SE, Hall EC, Axelrod DA, Lentine KL, et al. MELD exceptions and rates of waiting list outcomes. Am J Transplant. 2011;11:2362-2371. doi: 10.1111/j.1600-6143.2011.03735.x
- Bodzin AS, Lunsford KE, Markovic D, Harlander-Locke MP, Busuttil RW, Agopian VG. Predicting mortality in patients developing recurrent hepatocellular carcinoma after liver transplantation: impact of treatment modality and recurrence characteristics. Ann Surg. 2017;266:118-125. doi: 10.1097/SLA.0000000000001894
- Gondolesi GE, Roayaie S, Muñoz L, Kim-Schluger L, Schiano T, Fishbein TM, et al. Adult living donor liver transplantation for patients with hepatocellular carcinoma: extending UNOS priority criteria. Ann Surg. 2004; 239:142-149. doi: 10.1097/01.sla.0000109022.32391.eb
- Kulik L, Abecassis M. Living donor liver transplantation for hepatocellular carcinoma. Gastroenterology. 2004; 127:S277-S282.
doi: 10.1053/j.gastro.2004.09.042 - Vakili K, Pomposelli JJ, Cheah YL, Akoad M, Lewis WD, Khettry U, et al. Living donor liver transplantation for hepatocellular carcinoma: increased recurrence but improved survival. Liver Transpl. 2009; 15:1861-1866. doi: 10.1002/lt.21940
- Yang ZF, Poon RT, Luo Y, Cheung CK, Ho DW, Lo CM, et al. Up-regulation of vascular endothelial growth factor (VEGF) in small-for-size liver grafts enhances macrophage activities through VEGF receptor 2-dependent pathway. J Immunol. 2004; 173:2507-2515.
doi: 10.4049/jimmunol.173.4.2507 - Shi JH, Huitfeldt HS, Suo ZH, Line PD. Growth of hepatocellular carcinoma in the regenerating liver. Liver Transpl. 2011;17:866-874.
doi: 10.1002/lt.22325 - Efimova EA, Glanemann M, Liu L, Schumacher G, Settmacher U, Jonas S, et al. Effects of human hepatocyte growth factor on the proliferation of human hepatocytes and hepatocellular carcinoma cell lines. Eur Surg Res. 2004; 36:300-307. doi: 10.1159/000079915
- Lo CM, Fan ST, Liu CL, Chan SC, Ng IO, Wong J. Living donor versus deceased donor liver transplantation for early irresectable hepatocellular carcinoma. Br J Surg. 2007; 94:78-86. doi: 10.1002/bjs.5528
- Fisher RA, Kulik LM, Freise CE, Lok AS, Shearon TH, Brown RS Jr, et al, for A2ALL Study Group. Hepatocellular carcinoma recurrence and death following living and deceased donor liver transplantation. Am J Transplant. 2007; 7: 1601-1608.
doi: 10.1111/j.1600-6143.2007.01802.x - Di Sandro S, Slim AO, Giacomoni A, Lauterio A, Mangoni I, Aseni P, et al. Living donor liver transplantation for hepatocellular carcinoma: long-term results compared with deceased donor liver transplantation. Transplant Proc. 2009; 41: 1283-1285.
doi: 10.1016/j.transproceed.2009.03.022 - Sandhu L, Sandroussi C, Guba M, Selzner M, Ghanekar A, Cattral MS, et al. Living donor liver transplantation versus deceased donor liver transplantation for hepatocellular carcinoma: comparable survival and recurrence. Liver Transpl. 2012; 18(3):315-22.
doi: 10.1002/lt.22477 - Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52-60.
doi: 10.1055/s-0030-1247132 - Hogen R, Dinorcia J, Lo M, Nguyen B, Genyk Y, Sher L, Dhanireddy K. Long wait time regions for liver transplantation for HCC have a higher cumulative incidence of death. [abstract]. Am J Transplant. 2017; 17 (suppl 3).
- Mehta N, Dodge JL, Hirose R, Roberts JP, Yao FY. Increasing liver transplantation wait-list dropout for hepatocellular carcinoma with widening geographical disparities: implications for organ allocation. Liver Transpl. 2018; 24(10):1346-1356. doi: 10.1002/lt.25317
- Ogawa K, Takada Y. Living vs. deceased-donor liver transplantation for patients with hepatocellular carcinoma. Transl Gastroenterol Hepatol. 2016;1:35. doi: 10.21037/tgh.2016.04.03. eCollection 2016
- Akamatsu N, Sugawara Y, Kokudo N. Living-donor vs deceased-donor liver transplantation for patients with hepatocellular carcinoma. World J Hepatol. 2014; 6(9):626-631. doi: 10.4254/wjh.v6.i9.626
- Zhu B, Wang J, Li H, Chen X, Zeng Y. Living or deceased organ donors in liver transplantation for hepatocellular carcinoma: a systematic review and meta-analysis. HPB (Oxford). 2019; 21(2):133-147. doi: 10.1016/j.hpb.2018.11.004
- Zhang HM, Shi YX, Sun LY, Zhu ZJ. Hepatocellular carcinoma recurrence in living and deceased donor liver transplantation: a systematic review and meta-analysis. Chin Med J. 2019; 132(13):1599-1609. doi: 10.1097/CM9.0000000000000287
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "40" ["~SORT"]=> string(2) "40" ["CODE"]=> string(100) "iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p" ["~CODE"]=> string(100) "iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p" ["EXTERNAL_ID"]=> string(4) "2054" ["~EXTERNAL_ID"]=> string(4) "2054" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(399) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноровOutcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(3396) "<p style="text-align: justify;">Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).</p> <h3?Пациенты и методы</h3> <p style="text-align: justify;">73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.</p> <h3>Результаты</h3> <p style="text-align: justify;">5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6). </p> <h3>Выводы</h3> <p style="text-align: justify;">Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость. </p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_META_TITLE"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_META_KEYWORDS"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_META_DESCRIPTION"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_PICTURE_FILE_ALT"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_PICTURE_FILE_TITLE"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_PICTURE_FILE_NAME"]=> string(100) "iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(261) "Исходы трансплантации печени у пациентов с гепатоцеллюлярной карциномой от живых доноров по сравнению с трансплантацией от погибших доноров" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(100) "iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(100) "iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(100) "iskhody-transplantatsii-pecheni-u-patsientov-s-gepatotsellyulyarnoy-kartsinomoy-ot-zhivykh-donorov-p" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "207" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28554" ["VALUE"]=> string(22) "11/16/2021 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "11/16/2021 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28555" ["VALUE"]=> string(22) "12/15/2021 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "12/15/2021 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28558" ["VALUE"]=> array(2) { ["TEXT"]=> string(95) "<p>Мохамед Р. Абдельфаттах, Хуссейн Эльсиеси</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(83) "
Мохамед Р. Абдельфаттах, Хуссейн Эльсиеси
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28559" ["VALUE"]=> array(2) { ["TEXT"]=> string(169) "<p>Отдел хирургии, Факультет медицины, Университет Александрии, Александрия, Египет </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(157) "Отдел хирургии, Факультет медицины, Университет Александрии, Александрия, Египет
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_RU"]=> array(36) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28560" ["VALUE"]=> array(2) { ["TEXT"]=> string(3396) "<p style="text-align: justify;">Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).</p> <h3?Пациенты и методы</h3> <p style="text-align: justify;">73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.</p> <h3>Результаты</h3> <p style="text-align: justify;">5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6). </p> <h3>Выводы</h3> <p style="text-align: justify;">Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3241) "Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).
73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.
Результаты
5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6).
Выводы
Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.
Ключевые слова
Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28556" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-43-49" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-43-49" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28561" ["VALUE"]=> array(2) { ["TEXT"]=> string(58) "<p>Mohamed R. Abdelfattah, Hussein Elsiesy</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(46) "Mohamed R. Abdelfattah, Hussein Elsiesy
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28562" ["VALUE"]=> array(2) { ["TEXT"]=> string(736) "<p style="text-align: justify;">Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt</p><br> <p><b>Correspondence:</b><br> Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131<br> Phone: 002010 2306 1111<br> Email: mohamad.rabie@gmail.com</p><br> <p><b>Citation:</b> Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(636) "Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt
Correspondence:
Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131
Phone: 002010 2306 1111
Email: mohamad.rabie@gmail.com
Citation: Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28563" ["VALUE"]=> array(2) { ["TEXT"]=> string(1985) "<p style="text-align: justify;"> Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) <i>versus </i>liver transplantation from deceased donor (DDLT) treated at our center. </p> <h3>Patients and methods</h3> <p style="text-align: justify;"> Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study. </p> <h3>Results</h3> <p style="text-align: justify;"> Overall survival outcomes at 5 years were, respectively, 80.3% <i>vs </i>70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% <i>vs</i> 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6). <h3>Conclusion</h3> <p style="text-align: justify;">The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.</p> <h2>Keywords</h2> <p style="text-align: justify;">Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1797) "Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) versus liver transplantation from deceased donor (DDLT) treated at our center.
Patients and methods
Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study.
Results
Overall survival outcomes at 5 years were, respectively, 80.3% vs 70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% vs 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6).
Conclusion
The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.
Keywords
Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28557" ["VALUE"]=> string(138) "Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(138) "Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> &array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28564" ["VALUE"]=> string(4) "2802" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2802" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28565" ["VALUE"]=> string(4) "2803" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2803" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(10) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28561" ["VALUE"]=> array(2) { ["TEXT"]=> string(58) "<p>Mohamed R. Abdelfattah, Hussein Elsiesy</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(46) "Mohamed R. Abdelfattah, Hussein Elsiesy
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(46) "Mohamed R. Abdelfattah, Hussein Elsiesy
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28563" ["VALUE"]=> array(2) { ["TEXT"]=> string(1985) "<p style="text-align: justify;"> Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) <i>versus </i>liver transplantation from deceased donor (DDLT) treated at our center. </p> <h3>Patients and methods</h3> <p style="text-align: justify;"> Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study. </p> <h3>Results</h3> <p style="text-align: justify;"> Overall survival outcomes at 5 years were, respectively, 80.3% <i>vs </i>70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% <i>vs</i> 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6). <h3>Conclusion</h3> <p style="text-align: justify;">The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.</p> <h2>Keywords</h2> <p style="text-align: justify;">Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1797) "Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) versus liver transplantation from deceased donor (DDLT) treated at our center.
Patients and methods
Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study.
Results
Overall survival outcomes at 5 years were, respectively, 80.3% vs 70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% vs 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6).
Conclusion
The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.
Keywords
Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(1797) "Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) versus liver transplantation from deceased donor (DDLT) treated at our center.
Patients and methods
Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study.
Results
Overall survival outcomes at 5 years were, respectively, 80.3% vs 70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% vs 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6).
Conclusion
The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.
Keywords
Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28556" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-43-49" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-43-49" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-43-49" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28557" ["VALUE"]=> string(138) "Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(138) "Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(138) "Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28562" ["VALUE"]=> array(2) { ["TEXT"]=> string(736) "<p style="text-align: justify;">Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt</p><br> <p><b>Correspondence:</b><br> Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131<br> Phone: 002010 2306 1111<br> Email: mohamad.rabie@gmail.com</p><br> <p><b>Citation:</b> Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(636) "Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt
Correspondence:
Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131
Phone: 002010 2306 1111
Email: mohamad.rabie@gmail.com
Citation: Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(636) "Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt
Correspondence:
Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131
Phone: 002010 2306 1111
Email: mohamad.rabie@gmail.com
Citation: Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28558" ["VALUE"]=> array(2) { ["TEXT"]=> string(95) "<p>Мохамед Р. Абдельфаттах, Хуссейн Эльсиеси</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(83) "Мохамед Р. Абдельфаттах, Хуссейн Эльсиеси
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(83) "Мохамед Р. Абдельфаттах, Хуссейн Эльсиеси
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28554" ["VALUE"]=> string(22) "11/16/2021 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "11/16/2021 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "11/16/2021 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28555" ["VALUE"]=> string(22) "12/15/2021 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "12/15/2021 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "12/15/2021 12:00:00 am" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28560" ["VALUE"]=> array(2) { ["TEXT"]=> string(3396) "<p style="text-align: justify;">Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).</p> <h3?Пациенты и методы</h3> <p style="text-align: justify;">73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.</p> <h3>Результаты</h3> <p style="text-align: justify;">5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6). </p> <h3>Выводы</h3> <p style="text-align: justify;">Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3241) "Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).
73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.
Результаты
5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6).
Выводы
Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.
Ключевые слова
Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(3241) "Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).
73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.
Результаты
5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6).
Выводы
Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.
Ключевые слова
Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28559" ["VALUE"]=> array(2) { ["TEXT"]=> string(169) "<p>Отдел хирургии, Факультет медицины, Университет Александрии, Александрия, Египет </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(157) "Отдел хирургии, Факультет медицины, Университет Александрии, Александрия, Египет
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(157) "Отдел хирургии, Факультет медицины, Университет Александрии, Александрия, Египет
" } } } [5]=> array(49) { ["IBLOCK_SECTION_ID"]=> string(3) "207" ["~IBLOCK_SECTION_ID"]=> string(3) "207" ["ID"]=> string(4) "2053" ["~ID"]=> string(4) "2053" ["IBLOCK_ID"]=> string(1) "2" ["~IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["~NAME"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["ACTIVE_FROM"]=> NULL ["~ACTIVE_FROM"]=> NULL ["TIMESTAMP_X"]=> string(22) "04/18/2022 02:46:14 pm" ["~TIMESTAMP_X"]=> string(22) "04/18/2022 02:46:14 pm" ["DETAIL_PAGE_URL"]=> string(144) "/en/archive/tom-11-nomer-1/klinicheskie-raboty/mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok/" ["~DETAIL_PAGE_URL"]=> string(144) "/en/archive/tom-11-nomer-1/klinicheskie-raboty/mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok/" ["LIST_PAGE_URL"]=> string(12) "/en/archive/" ["~LIST_PAGE_URL"]=> string(12) "/en/archive/" ["DETAIL_TEXT"]=> string(22443) "Introduction
Hematopoietic stem cell transplantation (HSCT) is used as an efficient therapeutic approach for treatment of oncohematological diseases. This mode of treatment causes profound immunosuppression affecting non-specific and specific immunity. This temporary disorder results into frequent infectious complications over post-transplant period, which have been sufficiently studied. However, bacterial and fungal paranasal sinusitis, which is common in general population, has been scarcely studied in immunocompromised patients after HSCT [1].
According to numerous studies, sinusitis affects approximately 5-44% of all the patients in post-transplant period, mainly, at early terms after HSCT. In this regard, searching for bacteria which colonize nasal cavity and paranasal sinuses during the sinusitis seems to be an urgent task. In general excessive microbiota at the surface of nasal mucosa, paranasal sinuses and upper respiratory tract is of similar composition. Bacteriological studies of cultivable microbiota from the nasal cavity and aspirates of maxillary sinuses in chronic rhinosinusitis were carried out in different clinics of Russian Federation and revealed 154 isolates of aerobic bacteria belonging to 32 species, and 90 anaerobic lines, with predominance of Streptococci, Prevotella in aspirates, less often S.pneumoniae, H.influenza, and S.aureus [2]. Although many other microbial species were isolated from these samples, the authors did not reveal their clear relations to pathogenesis of chronic rhinosinusitis.
Over the last decade, the microbiota of paranasal sinuses has also been studied by molecular biology techniques (quantitative PCR, microarray methods, like as by NGS studies of polymorphisms in 16S rRNA gene which is universal to bacterial microbiota), thus making it possible to identify a lot of non-cultivable and previously unknown types of bacteria [3]. The authors have shown that, along with S.epidermidis, S.aureus, Corynebacteria spp, maxillar sinuses in the patients may harbor, e.g., Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, as well as Stenotrophomonas maltophilia, Enterobacter which may be associated with chronic rhinosinusitis. Significant differences in the composition and diversity of the microbiota of the paranasal sinuses largely depend on the methods used in distinct studies. E.g., analysis of the microbiota at these sites by means of next-generation sequencing (NGS) showed persistence of Staphylococci, Streptococci, Neisseria, Corynebacteria and reduced biodiversity of local microbiota in chronic rhinosinusitis [4]. In general, however, bacteriological evaluation of biological samples retains its diagnostic value because of its ability to assess antibiotic resistance of microbial isolates. The aim of this study was a comparative assessment of aerobic and facultative anaerobic microbiota components of nasal and paranasal cavities in sinusitis, which is often observed in immunocompromised patients after intensive chemotherapy, antibiotic therapy and subsequent HSCT.
Patients and methods
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged from 1 to 62 years treated at the R. M. Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation under the protocols of intensive chemotherapy and allogeneic HSCT over the period of 2016 to 2021 as described in our previous work [5]. During HSCT, patients received an antibiotic prophylaxis regimen that included intravenous administration of fluoroquinolones (sometimes switching to oral administration) from D+1 to D+60. To this purpose, amoxicillin was also prescribed, in particular to pediatric patients. In febrile neutropenia, broad-spectrum antibiotics were empirically administered. Later on, upon occurrence of resistant microbial strains, the patients were treated with antibiotics, orally or systemically, as guided by the in vitro sensitivity testing of the microbial isolates.
As indicated by consulting specialist (ORL clinician), according to clinical indications, the biomaterial was taken from patients (nasal swabs or washings from the paranasal sinuses) at the terms of -100 to +180 days after the day of allogeneic HSCT. Of these specimens, we have examined 124 samples of the maxillary sinus punctures from 97 patients, and 973 scrapings from nasal cavity of the patients from general HSCT group.
Seeding and isolation of bacteria from the biological samples were made by classical bacteriological techniques, The isolated microorganisms were identified by means of commercial biochemical test systems (BBL Crystal), as well as with MALDI-TOF mass spectrometry using VITEK MS instrument. The sensitivity of clinical isolates to antibiotics was determined by means of disk diffusion test systems. The results of microbial sensitivity tests were interpreted according to the Guidelines of European Committee on Antimicrobial Susceptibility Testing (EUCAST) criteria. For statistical analysis, the groups of patients were also divided by age: 0-5 years (group 1); 6-14 children (2); 15-21 years old (3); >22 years (4). Moreover, the results of bacteriological examination were classified by terms post-transplant, starting from <100 days before HSCT (point 0); during the 1st month (point 1); 2nd month (point 2); 3rd month (point 3), etc., up to 6 months after HSCT (point 6). Statistical analysis of the data was carried out by means of parametric and nonparametric statistics, concerning individual types of inoculated microorganisms, and for distinct microbial associations at different times after HSCT using the STATISTICA 10 program.
Results
The detection frequency of cultured bacteria from nasal cavity and maxillary sinuses in the oncohematological patients with ORL disorders was as follows: S.epidermidis, 34.7% of biological samples (377/1097); S.viridans, 2.2% (24/1097); S.aureus, 1.91% (21/1097); Klebsiella spp., 1% (11/1097); Corynebacteria spp., 0.9% (10/1097); Pseudomonas spp., 0.54% (6/1097); E. coli, 0.36% (4/1097); Neisseria spp., 0.36% (4/1097); E.faecalis, 0.18% (2/1097). Meanwhile, Proteus, M.luteus, Citrobacter isolates were not revealed. Seeding rates for the most common bacterial species by the age groups are shown in Fig. 1A and 1B.

Figure 1. Age dependence of bacterial seeding rates for the dominant bacterial species in oncohematological patients (group 1: 0-5 years; group 2: 6-14 years; group 3: 15-21 years; group 4: >22 years)
As seen from Fig. 1, the frequency of S.epidermidis detection was minimal in younger age group and increases at the age of >15 years (1A). Also, the occurrence of S.viridans is minimal among younger patients, with a maximum in the older group (>15 years). Moreover, we assessed the dynamics for these species at various times after HSCT (Fig. 2A and 2B).

Figure 2. Dynamics of detection for the main types of bacteria at different terms after HSCT
As seen from Fig. 2A, the detection rate of S.epidermidis is sharply reduced over the first 2 months after HSCT, thus confirming significant depletion of this microbial population due to antibiotic prophylaxis and anti-infectious therapy at the early stages after HSCT. At the same time, frequency of S.viridans did not change significantly during the post-transplant period (up to 6 months).
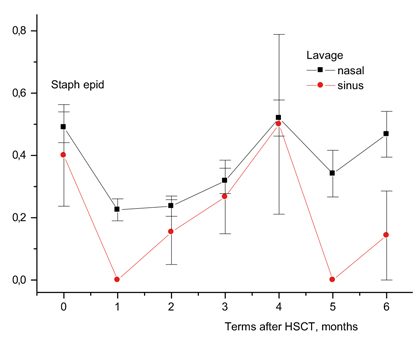
Figure 3. Frequency of S.epidermidis detection in nasal swabs (squares) and maxillary sinuses (circles) at various terms after HSCT
Separate analysis in adjacent infection loci (nasal and maxillar cavities) showed that the most profound suppression of S.epidermidis growth was observed in paranasal sinuses, especially, within 1 month after HSCT (Fig. 3). Of interest, the frequency of S.epidermidis isolation in the presence of clinically sound sinusitis was even more reduced during the 1st month after HSCT, as well as in later periods (>4 months after HSCT), as shown in Fig. 4.
High frequency of Klebsiella spp. isolation in the samples from maxillar sinuses proved to be the most pronounced feature of pathogenic microbiota in the patients at the late terms after HSCT (an average of 16.3% (20/123) versus 2.1% (18/864), p=2×10^14), along with low frequency detection in nasal swabs (Fig. 5). Similarly, high seeding rates from sinus washes were shown for Pseudomonas spp. (8.1%, 10/123 versus 0.7%, 5/864, p=1.5×10^10).

As can be seen from Table 1, S.epidermidis, the most common microflora for the nasopharynx, is found in material from the nose much more often than in swabs from the maxillary sinuses (Fig. 4). Meanwhile, inoculation with S.epidermidis from the maxillary sinuses is minimal during 1 and 5 months after HSCT. At the same time, opportunistic pathogens (E. coli, Klebsiella spp., Pseudomonas spp.) in the lavage from maxillary sinuses of the patients with sinusitis were detected more frequently than in nasal cavity lavage.
Table 1. Comparative detection frequency of main bacterial species in the samples from nasal cavity and paranasal sinuses in the patients with ORL disorders after HSCT

This confirms the diagnostic significance of the bacteriological analysis of the exudate obtained by sinus puncture and, possibly, the protective function of S.epidermidis on the skin and mucous membranes.
Next, we determined the isolation frequency of distinct microbes from the general data massive (nasal cavity + maxillary sinuses) and found that Klebsiella spp. with symptoms of sinusitis occurs significantly more often than in patients free of these symptoms, respectively, 6/102 (5.9%) versus 8/501 (1.6%), p=0.009. A similar increase was shown for Pseudomonas spp. and E.coli (see Table 2). A higher frequency of detection of Klebsiella spp. in the punctures from maxillary sinuses was noted in cases of clinical sinusitis at the 1st, 2nd month, as well as from the 4th month and later post-HSCT.
Table 2. Incidence of different bacterial species in the samples from nasal cavity and/or maxillary sinuses in the patients with sinusitis compared with sinusitis-free patients subjected to HSCT

Moreover, we estimated the frequency of bacterial findings within +30 days since clinical diagnosis of sinusitis. Higher frequency of Pseudomonas spp. (1/378 vs 7/217) was revealed in the samples from paranasal sinuses in 5 patients within 3 weeks after clinical diagnosis of sinusitis.
Antibiotic resistance
Several resistant bacterial strains were isolated from nasal cavity and paranasal sinuses in the patients with sinusitis, mostly, at later terms (>2 months post-transplant).
Over the entire period of time (2019 to 2021), the clinical staphylococcal isolates were tested for their sensitivity to cefoxitin, erythromycin, clindamycin, gentamycin, norfloxacin, tetracycline, tigecycline, and linezolid. According to the expert Guidelines of European Committee on Antimicrobial Susceptibility Testing (EUCAST). Cefoxitin is considered a screening drug in order to discriminate between the categories of methicillin-resistant staphylococci (MRS) and methicillin-sensitive strains (MSS). Throughout the observation terms, the methicillin-resistant S.aureus (MRSA) were isolated in 4% of lavage and puncture samples obtained from maxillar sinuses in the patients with oncohematological disorders. Over this period of time, we did not reveal any S. aureus strains resistant to linezolid or tigecycline. 31% of S.aureus isolates were resistant to erythromycin. The revealed category of erythromycin sensitivity, in accordance with EUCAST rules, is also extended to clarithromycin and roxytromycin. Norfloxacin resistance was shown for 5% of S.aureus strains. The norfloxacin-sensitive staphylococci are regarded as sensitive to moxifloxacin and, at higher doses (or with prolonged infusion), to levofloxacin and ciprofloxacin. Tetracycline resistance of S. aureus strains was shown in 10%. The tetracycline-sensitive staphylococci are also considered sensitive to doxycycline and minocycline. Maximal percentage of antibiotic resistance for staphylococcal strains was found with gentamycin (24%). Gradient diffusion tests for vancomycin resistance were applied to methycillin-resistant staphylococci (E-test). All the MRSA strains proved to be vancomycin-sensitive.
All the E.faecalis isolates obtained from nasal cavity of the patients treated for oncohematological disorders who suffered from sinusitis have shown good sensitivity level with antibacterial drugs, i.e., 100% to ampicillin, linezolid, vancomycin and tigecycline.
100% of S.pneumoniae strains isolated in this study were sensitive to oxacillin, and therefore, to all β-lactam antibiotics. Among them, 90% showed sensitivity to norfloxacin and, hence, to moxifloxacin. Over the study period, we have not revealed any Pneumococcus strains resistant to vancomycin and linezolid. Resistance to tetracycline and erythromycin was detected for 70% of S.pneumoniae strains.
The species of Enterobacterales exhibited different patterns of antibiotic resistance. E.g., all E. coli strains were sensitive to amikacine, 3rd-generation cephalosporins (cefotaxim, ceftazidim, ceftriaxone), protected aminopenicillines, and meropenem. Meanwhile, resistance of Klebsiella pneumoniae ssp pneumoniae, the actual nosocomial pathogen, proved to be increased over this observation period, being as high as 85% to cephalosporins (III generation) and to meropenem (60%).
Discussion
Acute sinusitis is a common complication following HSCT, and several studies addressed this issue [6, 7]. Immunosuppressive drugs, chemotherapy, radiation treatment, prolonged antibiotic therapy, autoaggressive graft-versus-host disease (GVHD), and long periods of hospitalization are predisposing factors for the upper respiratory tract infections. Current clinical diagnostics of sinusitis, both before and after HSCT, is often based on computed tomography (CT) findings, which in many cases correlate with history and clinical examination data [8]. The authors have shown that the severity of pre-transplant sinus lesions revealed on CT scans correlated with clinical and radiological signs of sinusitis later post-transplant, having been associated with a trend for reduced survival. Therefore, the clinical background before HSCT is also important for assessing further risks of developing ORL disorders. Our results of bacteriological testing are based on the clinical cohort treated at the R. M. Gorbacheva Memorial Research Institute of Children Oncology, Hematology and Transplantation [5]. Infectious complications in allogeneic HSCT are significantly more common than in autologous HSCT, with respect to cytopenic period and rates of hematopoietic recovery. Our data refer to the patients who received allogeneic HSCT. Acute symptoms of rhinosinusitis may be registered at any term after HSCT, reaching 5.3% (95% CI 5.0%-5.6%) at the stage before transplantation; 3.01% (95% CI 2.8%-3.2%) in the course of engraftment, and 8.13% (95% CI 7.67%-8.60%), post-engraftment. From this comparison, one may suggest that massive antibiotic therapy after HSCT appears to prevent some of infectious conditions at the early stages post-transplant. However, later recolonization of pathogenic microorganisms is possible, including Klebsiella spp., S. aureus, S.pneumoniae, at a high risk of resistant strain selection, which was confirmed by us in the present work. One should note, however, that these 3 types of pathogenic bacteria were detected in a total of 13% of patients with sinusitis, i.e. the pathogen remained unknown in most cases. For additional diagnostics, along with search for pathogenic fungi and viruses, the extended diagnostics, e.g., of strictly anaerobic microbiota, are needed. In this aspect, implementation of advanced sequencing (NGS technique) will be of great importance, thus making it possible to assess biological diversity and the ratio of main microbiota classes in complex clinical samples, e.g., from mucosal surfaces.
Conclusions
1. The studies of relationships between the presence of facultative anaerobic, opportunistic microbiota in maxillar punctures and nasal cavities, and clinical course of sinusitis in the patients undergoing allogeneic HSCT did not reveal any significant correlations with severity of the disease (mild versus moderate grade).
2. Standard bacteriological testing aimed for detection of facultative anaerobic microorganisms in the maxillary sinus punctures after HSCT is of limited value within 1 month after HSCT, due to massive antibiotic therapy and suppressed growth of antibiotic-sensitive bacteria.
3. Massive antimicrobial therapy leads to the selection of resistant strains of Klebsiella spp., Pseudomonas spp., E.coli, S.aureus, mainly within 2 or more months after HSCT.
4. Low frequency of cultivable potentially pathogenic microorganisms in sino-nasal exudates cultures suggests reduced detection efficiency for the etiologically important bacteria which may cause sinusitis.
5. More sensitive and specific methods for detecting bacteria on the oropharyngeal and nasopharyngeal mucosa could be based on DNA diagnostics and multiplex PCR techniques, especially due to possible contamination of these sites with anaerobic bacteria of intestinal origin.
Conflict of interest
None declared.
References
- Bento LR, Ortiz E, Nicola EM, Vigorito AC, Sakano E. Sinonasal disorders in hematopoietic stem cell transplantation. Braz J Otorhinolaryngol. 2014; 80: 285-289. doi: 10.1016/j.bjorl.2014.05.009
- Ivanchenko OA, Karpishchenko SA, Kozlov RS, Krechikova OI, Otvagin IV, Sopko ON, Piskunov GZ, Lopatin AS. The microbiome of the maxillary sinus and middle nasal meatus in chronic rhinosinusitis. Rhinology. 2016; 54: 68-74. doi: 10.4193/Rhino15.018
- Lee JT, Frank DN, Ramakrishnan V. Microbiome of the paranasal sinuses: Update and literature review. Am J Rhinol Allergy 2016; 30: 3-16. doi: 10.2500/ajra.2016.30.4255
- De Boeck I, Wittouck S, Martens K, Claes J, Jorissen M, Steelant B, van den Broek, MFL, Seys SF, Hellings PW, Vanderveken OM, Lebeer S. Anterior nares diversity and pathobionts represent sinus microbiome in chronic rhinosinusitis. mSphere 2019; 4:e00532-19. doi: 10.1128/mSphere.00532-19
- Dolgov OI, Karpishchenko SA, Rodneva YA, Utimisheva ES, Moiseev IS, Zubarovskaya LS, Kulagin AD. Prevalence of acute inflammatory otorhinolaryngological diseases in hematopoietic stem cell transplant recipients. Russian Otorhinolaryngology. 2021;20(3):20-26 (In Russian.). doi: 10.18692/1810-4800-2021-3-20-26
- Drozd-Sokolowska JE, Sokolowski J, Wiktor-Jedrzejczak W, Niemczyk K. Sinusitis in patients undergoing allogeneic bone marrow transplantation – a review. Braz J Otorhinolaryngol. 2017 Jan-Feb;83(1):105-111. doi: 10.1016/j.bjorl.2016.02.012
- Utimisheva ES, Dolgov OI, Paina OV, Ekushov KA, Vitrischak AA, Smirnov BI, Zubarovskaya LS, Karpischenko SA, Afanasyev BV. Incidence, diagnosis and treatment of sinusitis in children and adolescents after hematopoietic stem cell transplantation. Cell Ther Transplant. 2019; 8(1):46-53.
- Billings KR, Lowe LH, AquinoVM, Biavati MJ. Screening sinus CT scans in pediatric bone marrow transplant patients. Otorhinolaryngology. 2000; 52(3): 253-260.
" ["~DETAIL_TEXT"]=> string(22443) "
Introduction
Hematopoietic stem cell transplantation (HSCT) is used as an efficient therapeutic approach for treatment of oncohematological diseases. This mode of treatment causes profound immunosuppression affecting non-specific and specific immunity. This temporary disorder results into frequent infectious complications over post-transplant period, which have been sufficiently studied. However, bacterial and fungal paranasal sinusitis, which is common in general population, has been scarcely studied in immunocompromised patients after HSCT [1].
According to numerous studies, sinusitis affects approximately 5-44% of all the patients in post-transplant period, mainly, at early terms after HSCT. In this regard, searching for bacteria which colonize nasal cavity and paranasal sinuses during the sinusitis seems to be an urgent task. In general excessive microbiota at the surface of nasal mucosa, paranasal sinuses and upper respiratory tract is of similar composition. Bacteriological studies of cultivable microbiota from the nasal cavity and aspirates of maxillary sinuses in chronic rhinosinusitis were carried out in different clinics of Russian Federation and revealed 154 isolates of aerobic bacteria belonging to 32 species, and 90 anaerobic lines, with predominance of Streptococci, Prevotella in aspirates, less often S.pneumoniae, H.influenza, and S.aureus [2]. Although many other microbial species were isolated from these samples, the authors did not reveal their clear relations to pathogenesis of chronic rhinosinusitis.
Over the last decade, the microbiota of paranasal sinuses has also been studied by molecular biology techniques (quantitative PCR, microarray methods, like as by NGS studies of polymorphisms in 16S rRNA gene which is universal to bacterial microbiota), thus making it possible to identify a lot of non-cultivable and previously unknown types of bacteria [3]. The authors have shown that, along with S.epidermidis, S.aureus, Corynebacteria spp, maxillar sinuses in the patients may harbor, e.g., Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, as well as Stenotrophomonas maltophilia, Enterobacter which may be associated with chronic rhinosinusitis. Significant differences in the composition and diversity of the microbiota of the paranasal sinuses largely depend on the methods used in distinct studies. E.g., analysis of the microbiota at these sites by means of next-generation sequencing (NGS) showed persistence of Staphylococci, Streptococci, Neisseria, Corynebacteria and reduced biodiversity of local microbiota in chronic rhinosinusitis [4]. In general, however, bacteriological evaluation of biological samples retains its diagnostic value because of its ability to assess antibiotic resistance of microbial isolates. The aim of this study was a comparative assessment of aerobic and facultative anaerobic microbiota components of nasal and paranasal cavities in sinusitis, which is often observed in immunocompromised patients after intensive chemotherapy, antibiotic therapy and subsequent HSCT.
Patients and methods
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged from 1 to 62 years treated at the R. M. Gorbacheva Memorial Research Institute of Pediatric Oncology, Hematology and Transplantation under the protocols of intensive chemotherapy and allogeneic HSCT over the period of 2016 to 2021 as described in our previous work [5]. During HSCT, patients received an antibiotic prophylaxis regimen that included intravenous administration of fluoroquinolones (sometimes switching to oral administration) from D+1 to D+60. To this purpose, amoxicillin was also prescribed, in particular to pediatric patients. In febrile neutropenia, broad-spectrum antibiotics were empirically administered. Later on, upon occurrence of resistant microbial strains, the patients were treated with antibiotics, orally or systemically, as guided by the in vitro sensitivity testing of the microbial isolates.
As indicated by consulting specialist (ORL clinician), according to clinical indications, the biomaterial was taken from patients (nasal swabs or washings from the paranasal sinuses) at the terms of -100 to +180 days after the day of allogeneic HSCT. Of these specimens, we have examined 124 samples of the maxillary sinus punctures from 97 patients, and 973 scrapings from nasal cavity of the patients from general HSCT group.
Seeding and isolation of bacteria from the biological samples were made by classical bacteriological techniques, The isolated microorganisms were identified by means of commercial biochemical test systems (BBL Crystal), as well as with MALDI-TOF mass spectrometry using VITEK MS instrument. The sensitivity of clinical isolates to antibiotics was determined by means of disk diffusion test systems. The results of microbial sensitivity tests were interpreted according to the Guidelines of European Committee on Antimicrobial Susceptibility Testing (EUCAST) criteria. For statistical analysis, the groups of patients were also divided by age: 0-5 years (group 1); 6-14 children (2); 15-21 years old (3); >22 years (4). Moreover, the results of bacteriological examination were classified by terms post-transplant, starting from <100 days before HSCT (point 0); during the 1st month (point 1); 2nd month (point 2); 3rd month (point 3), etc., up to 6 months after HSCT (point 6). Statistical analysis of the data was carried out by means of parametric and nonparametric statistics, concerning individual types of inoculated microorganisms, and for distinct microbial associations at different times after HSCT using the STATISTICA 10 program.
Results
The detection frequency of cultured bacteria from nasal cavity and maxillary sinuses in the oncohematological patients with ORL disorders was as follows: S.epidermidis, 34.7% of biological samples (377/1097); S.viridans, 2.2% (24/1097); S.aureus, 1.91% (21/1097); Klebsiella spp., 1% (11/1097); Corynebacteria spp., 0.9% (10/1097); Pseudomonas spp., 0.54% (6/1097); E. coli, 0.36% (4/1097); Neisseria spp., 0.36% (4/1097); E.faecalis, 0.18% (2/1097). Meanwhile, Proteus, M.luteus, Citrobacter isolates were not revealed. Seeding rates for the most common bacterial species by the age groups are shown in Fig. 1A and 1B.

Figure 1. Age dependence of bacterial seeding rates for the dominant bacterial species in oncohematological patients (group 1: 0-5 years; group 2: 6-14 years; group 3: 15-21 years; group 4: >22 years)
As seen from Fig. 1, the frequency of S.epidermidis detection was minimal in younger age group and increases at the age of >15 years (1A). Also, the occurrence of S.viridans is minimal among younger patients, with a maximum in the older group (>15 years). Moreover, we assessed the dynamics for these species at various times after HSCT (Fig. 2A and 2B).

Figure 2. Dynamics of detection for the main types of bacteria at different terms after HSCT
As seen from Fig. 2A, the detection rate of S.epidermidis is sharply reduced over the first 2 months after HSCT, thus confirming significant depletion of this microbial population due to antibiotic prophylaxis and anti-infectious therapy at the early stages after HSCT. At the same time, frequency of S.viridans did not change significantly during the post-transplant period (up to 6 months).
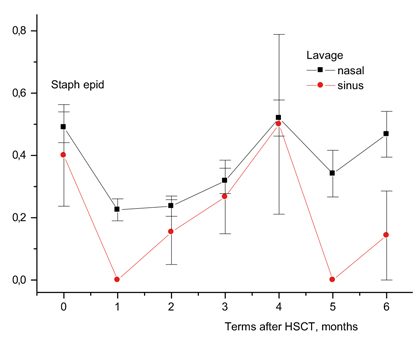
Figure 3. Frequency of S.epidermidis detection in nasal swabs (squares) and maxillary sinuses (circles) at various terms after HSCT
Separate analysis in adjacent infection loci (nasal and maxillar cavities) showed that the most profound suppression of S.epidermidis growth was observed in paranasal sinuses, especially, within 1 month after HSCT (Fig. 3). Of interest, the frequency of S.epidermidis isolation in the presence of clinically sound sinusitis was even more reduced during the 1st month after HSCT, as well as in later periods (>4 months after HSCT), as shown in Fig. 4.
High frequency of Klebsiella spp. isolation in the samples from maxillar sinuses proved to be the most pronounced feature of pathogenic microbiota in the patients at the late terms after HSCT (an average of 16.3% (20/123) versus 2.1% (18/864), p=2×10^14), along with low frequency detection in nasal swabs (Fig. 5). Similarly, high seeding rates from sinus washes were shown for Pseudomonas spp. (8.1%, 10/123 versus 0.7%, 5/864, p=1.5×10^10).

As can be seen from Table 1, S.epidermidis, the most common microflora for the nasopharynx, is found in material from the nose much more often than in swabs from the maxillary sinuses (Fig. 4). Meanwhile, inoculation with S.epidermidis from the maxillary sinuses is minimal during 1 and 5 months after HSCT. At the same time, opportunistic pathogens (E. coli, Klebsiella spp., Pseudomonas spp.) in the lavage from maxillary sinuses of the patients with sinusitis were detected more frequently than in nasal cavity lavage.
Table 1. Comparative detection frequency of main bacterial species in the samples from nasal cavity and paranasal sinuses in the patients with ORL disorders after HSCT

This confirms the diagnostic significance of the bacteriological analysis of the exudate obtained by sinus puncture and, possibly, the protective function of S.epidermidis on the skin and mucous membranes.
Next, we determined the isolation frequency of distinct microbes from the general data massive (nasal cavity + maxillary sinuses) and found that Klebsiella spp. with symptoms of sinusitis occurs significantly more often than in patients free of these symptoms, respectively, 6/102 (5.9%) versus 8/501 (1.6%), p=0.009. A similar increase was shown for Pseudomonas spp. and E.coli (see Table 2). A higher frequency of detection of Klebsiella spp. in the punctures from maxillary sinuses was noted in cases of clinical sinusitis at the 1st, 2nd month, as well as from the 4th month and later post-HSCT.
Table 2. Incidence of different bacterial species in the samples from nasal cavity and/or maxillary sinuses in the patients with sinusitis compared with sinusitis-free patients subjected to HSCT

Moreover, we estimated the frequency of bacterial findings within +30 days since clinical diagnosis of sinusitis. Higher frequency of Pseudomonas spp. (1/378 vs 7/217) was revealed in the samples from paranasal sinuses in 5 patients within 3 weeks after clinical diagnosis of sinusitis.
Antibiotic resistance
Several resistant bacterial strains were isolated from nasal cavity and paranasal sinuses in the patients with sinusitis, mostly, at later terms (>2 months post-transplant).
Over the entire period of time (2019 to 2021), the clinical staphylococcal isolates were tested for their sensitivity to cefoxitin, erythromycin, clindamycin, gentamycin, norfloxacin, tetracycline, tigecycline, and linezolid. According to the expert Guidelines of European Committee on Antimicrobial Susceptibility Testing (EUCAST). Cefoxitin is considered a screening drug in order to discriminate between the categories of methicillin-resistant staphylococci (MRS) and methicillin-sensitive strains (MSS). Throughout the observation terms, the methicillin-resistant S.aureus (MRSA) were isolated in 4% of lavage and puncture samples obtained from maxillar sinuses in the patients with oncohematological disorders. Over this period of time, we did not reveal any S. aureus strains resistant to linezolid or tigecycline. 31% of S.aureus isolates were resistant to erythromycin. The revealed category of erythromycin sensitivity, in accordance with EUCAST rules, is also extended to clarithromycin and roxytromycin. Norfloxacin resistance was shown for 5% of S.aureus strains. The norfloxacin-sensitive staphylococci are regarded as sensitive to moxifloxacin and, at higher doses (or with prolonged infusion), to levofloxacin and ciprofloxacin. Tetracycline resistance of S. aureus strains was shown in 10%. The tetracycline-sensitive staphylococci are also considered sensitive to doxycycline and minocycline. Maximal percentage of antibiotic resistance for staphylococcal strains was found with gentamycin (24%). Gradient diffusion tests for vancomycin resistance were applied to methycillin-resistant staphylococci (E-test). All the MRSA strains proved to be vancomycin-sensitive.
All the E.faecalis isolates obtained from nasal cavity of the patients treated for oncohematological disorders who suffered from sinusitis have shown good sensitivity level with antibacterial drugs, i.e., 100% to ampicillin, linezolid, vancomycin and tigecycline.
100% of S.pneumoniae strains isolated in this study were sensitive to oxacillin, and therefore, to all β-lactam antibiotics. Among them, 90% showed sensitivity to norfloxacin and, hence, to moxifloxacin. Over the study period, we have not revealed any Pneumococcus strains resistant to vancomycin and linezolid. Resistance to tetracycline and erythromycin was detected for 70% of S.pneumoniae strains.
The species of Enterobacterales exhibited different patterns of antibiotic resistance. E.g., all E. coli strains were sensitive to amikacine, 3rd-generation cephalosporins (cefotaxim, ceftazidim, ceftriaxone), protected aminopenicillines, and meropenem. Meanwhile, resistance of Klebsiella pneumoniae ssp pneumoniae, the actual nosocomial pathogen, proved to be increased over this observation period, being as high as 85% to cephalosporins (III generation) and to meropenem (60%).
Discussion
Acute sinusitis is a common complication following HSCT, and several studies addressed this issue [6, 7]. Immunosuppressive drugs, chemotherapy, radiation treatment, prolonged antibiotic therapy, autoaggressive graft-versus-host disease (GVHD), and long periods of hospitalization are predisposing factors for the upper respiratory tract infections. Current clinical diagnostics of sinusitis, both before and after HSCT, is often based on computed tomography (CT) findings, which in many cases correlate with history and clinical examination data [8]. The authors have shown that the severity of pre-transplant sinus lesions revealed on CT scans correlated with clinical and radiological signs of sinusitis later post-transplant, having been associated with a trend for reduced survival. Therefore, the clinical background before HSCT is also important for assessing further risks of developing ORL disorders. Our results of bacteriological testing are based on the clinical cohort treated at the R. M. Gorbacheva Memorial Research Institute of Children Oncology, Hematology and Transplantation [5]. Infectious complications in allogeneic HSCT are significantly more common than in autologous HSCT, with respect to cytopenic period and rates of hematopoietic recovery. Our data refer to the patients who received allogeneic HSCT. Acute symptoms of rhinosinusitis may be registered at any term after HSCT, reaching 5.3% (95% CI 5.0%-5.6%) at the stage before transplantation; 3.01% (95% CI 2.8%-3.2%) in the course of engraftment, and 8.13% (95% CI 7.67%-8.60%), post-engraftment. From this comparison, one may suggest that massive antibiotic therapy after HSCT appears to prevent some of infectious conditions at the early stages post-transplant. However, later recolonization of pathogenic microorganisms is possible, including Klebsiella spp., S. aureus, S.pneumoniae, at a high risk of resistant strain selection, which was confirmed by us in the present work. One should note, however, that these 3 types of pathogenic bacteria were detected in a total of 13% of patients with sinusitis, i.e. the pathogen remained unknown in most cases. For additional diagnostics, along with search for pathogenic fungi and viruses, the extended diagnostics, e.g., of strictly anaerobic microbiota, are needed. In this aspect, implementation of advanced sequencing (NGS technique) will be of great importance, thus making it possible to assess biological diversity and the ratio of main microbiota classes in complex clinical samples, e.g., from mucosal surfaces.
Conclusions
1. The studies of relationships between the presence of facultative anaerobic, opportunistic microbiota in maxillar punctures and nasal cavities, and clinical course of sinusitis in the patients undergoing allogeneic HSCT did not reveal any significant correlations with severity of the disease (mild versus moderate grade).
2. Standard bacteriological testing aimed for detection of facultative anaerobic microorganisms in the maxillary sinus punctures after HSCT is of limited value within 1 month after HSCT, due to massive antibiotic therapy and suppressed growth of antibiotic-sensitive bacteria.
3. Massive antimicrobial therapy leads to the selection of resistant strains of Klebsiella spp., Pseudomonas spp., E.coli, S.aureus, mainly within 2 or more months after HSCT.
4. Low frequency of cultivable potentially pathogenic microorganisms in sino-nasal exudates cultures suggests reduced detection efficiency for the etiologically important bacteria which may cause sinusitis.
5. More sensitive and specific methods for detecting bacteria on the oropharyngeal and nasopharyngeal mucosa could be based on DNA diagnostics and multiplex PCR techniques, especially due to possible contamination of these sites with anaerobic bacteria of intestinal origin.
Conflict of interest
None declared.
References
- Bento LR, Ortiz E, Nicola EM, Vigorito AC, Sakano E. Sinonasal disorders in hematopoietic stem cell transplantation. Braz J Otorhinolaryngol. 2014; 80: 285-289. doi: 10.1016/j.bjorl.2014.05.009
- Ivanchenko OA, Karpishchenko SA, Kozlov RS, Krechikova OI, Otvagin IV, Sopko ON, Piskunov GZ, Lopatin AS. The microbiome of the maxillary sinus and middle nasal meatus in chronic rhinosinusitis. Rhinology. 2016; 54: 68-74. doi: 10.4193/Rhino15.018
- Lee JT, Frank DN, Ramakrishnan V. Microbiome of the paranasal sinuses: Update and literature review. Am J Rhinol Allergy 2016; 30: 3-16. doi: 10.2500/ajra.2016.30.4255
- De Boeck I, Wittouck S, Martens K, Claes J, Jorissen M, Steelant B, van den Broek, MFL, Seys SF, Hellings PW, Vanderveken OM, Lebeer S. Anterior nares diversity and pathobionts represent sinus microbiome in chronic rhinosinusitis. mSphere 2019; 4:e00532-19. doi: 10.1128/mSphere.00532-19
- Dolgov OI, Karpishchenko SA, Rodneva YA, Utimisheva ES, Moiseev IS, Zubarovskaya LS, Kulagin AD. Prevalence of acute inflammatory otorhinolaryngological diseases in hematopoietic stem cell transplant recipients. Russian Otorhinolaryngology. 2021;20(3):20-26 (In Russian.). doi: 10.18692/1810-4800-2021-3-20-26
- Drozd-Sokolowska JE, Sokolowski J, Wiktor-Jedrzejczak W, Niemczyk K. Sinusitis in patients undergoing allogeneic bone marrow transplantation – a review. Braz J Otorhinolaryngol. 2017 Jan-Feb;83(1):105-111. doi: 10.1016/j.bjorl.2016.02.012
- Utimisheva ES, Dolgov OI, Paina OV, Ekushov KA, Vitrischak AA, Smirnov BI, Zubarovskaya LS, Karpischenko SA, Afanasyev BV. Incidence, diagnosis and treatment of sinusitis in children and adolescents after hematopoietic stem cell transplantation. Cell Ther Transplant. 2019; 8(1):46-53.
- Billings KR, Lowe LH, AquinoVM, Biavati MJ. Screening sinus CT scans in pediatric bone marrow transplant patients. Otorhinolaryngology. 2000; 52(3): 253-260.
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "30" ["~SORT"]=> string(2) "30" ["CODE"]=> string(96) "mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok" ["~CODE"]=> string(96) "mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok" ["EXTERNAL_ID"]=> string(4) "2053" ["~EXTERNAL_ID"]=> string(4) "2053" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(262) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клетокMicrobiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(5126) "<p style="text-align: justify;"> Трансплантация гемопоэтических стволовых клеток (ТГСК) часто сопровождается инфекционными осложнениями. Целью настоящего исследования была сравнительная оценка состава факультативно-анаэробных представителей микробиоты полости носа и его придаточных пазух при синусите, который нередко развивается у иммунокомпромиссных пациентов после интенсивной химио- и антибиотикотерапии и трансплантации гемопоэтических клеток (ТГСК). </p> <h3>Материалы и методы</h3> <p style="text-align: justify;"> В исследовании участвовали 194 пациента с различными миело- и лимфопролиферативными заболеваниями в возрасте от 1 до 62 лет, проходившие интенсивную химиотерапию и аллогенную ТГСК. При наличии клинических показаний у пациентов забирали биоматериал (смывы из околоносовых пазух и/или назальные мазки) в сроки от -100 до +180 суток после аллогенной ТГСК. Исследовано 124 образца пунктатов верхнечелюстных пазух от 97 пациентов и 973 мазка-соскоба из полости носа. Посев биоматериала и выделение микроорганизмов проводили классическими бактериологическими методами. Чувствительность клинических изолятов к антибиотикам определяли диско-диффузионным методом. Интерпретацию результатов чувствительности осуществляли согласно критериям EUCAST. </p> <h3>Результаты</h3> <p style="text-align: justify;"> В биоматериале из полости носа и околоносовых пазух наиболее часто высевали <i>S.epidermidis</i> – 34,7% (377/1097); <i>S.viridans</i> – 2,2% (24/1097); <i>S. aureus</i> – 1,91% (21/1097); <i>Klebsiella spp</i> – 1% (11/1097). Частота выявления <i>S.epidermidis</i> и <i>S.viridans</i> была минимальной в младшей возрастной группе (до 5 лет) и возрастала в группах от 15 лет и выше. Глубокое подавление роста <i>S.epidermidis</i> отмечалось (в особенности – в околоносовых синусах) в течение 1-го мес. после ТГСК на фоне массивной антибиотикотерапии. Отмечена высокая частота выявления <i>Klebsiella spp</i> в материале из синусов в поздние сроки (2-3 мес.) после ТГСК при малой частоте выявления в материале из полости носа (в среднем 16,3% против 2.1%, р=2×10^14). Кроме того, мы оценили частоту высеваемости бактерий в сроки +30 сут. от постановки диагноза синусита. При этом была выявлена повышенная частота выделения <i>Pseudomonas spp</i> (1/378 <i>vs </i>7/217) в материале из придаточных пазух. </p> <h3>Заключение</h3> <p style="text-align: justify;"> Бактериологические исследование материала из гайморовых пазух имеет ограниченную ценность в течение 1-го мес. после ТГСК в связи с массивной антибиотикотерапией, которая сопровождается селекцией резистентных штаммов <i>Klebsiella spp, Pseudomonas spp, E.coli, S.aureus</i>, главным образом – в сроки 2 и более мес. после ТГСК. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;"> Tрансплантация гемопоэтических стволовых клеток, околоносовые пазухи, микробиота, антибиотикорезистентность. </p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_META_TITLE"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_META_KEYWORDS"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_META_DESCRIPTION"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_PICTURE_FILE_ALT"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_PICTURE_FILE_TITLE"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_PICTURE_FILE_NAME"]=> string(100) "mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok-img" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(173) "Микробиота полости носа при синуситах после трансплантации гемопоэтических стволовых клеток" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(100) "mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok-img" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(100) "mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok-img" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(100) "mikrobiota-polosti-nosa-pri-sinusitakh-posle-transplantatsii-gemopoeticheskikh-stvolovykh-kletok-img" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "207" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28542" ["VALUE"]=> string(22) "02/06/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "02/06/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28543" ["VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28544" ["VALUE"]=> array(2) { ["TEXT"]=> string(566) "<p>Олег И. Долгов<sup>1</sup>, Сергей А. Карпищенко<sup>1</sup>, Екатерина С. Утимишева<sup>1</sup>, Диана А. Григорьянц<sup>1</sup>, Анна А. Спиридонова<sup>1,2</sup>, Иван С. Моисеев<sup>1</sup>, Людмила С. Зубаровская<sup>1</sup>, Алексей Б. Чухловин<sup>1</sup>, Александр Д. Кулагин<sup>1</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(446) "
Олег И. Долгов1, Сергей А. Карпищенко1, Екатерина С. Утимишева1, Диана А. Григорьянц1, Анна А. Спиридонова1,2, Иван С. Моисеев1, Людмила С. Зубаровская1, Алексей Б. Чухловин1, Александр Д. Кулагин1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28545" ["VALUE"]=> array(2) { ["TEXT"]=> string(435) "<p><sup>1</sup> Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия<br> <sup>2</sup> ФБУН НИИ эпидемиологии и микробиологии имени Пастера, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(393) "1 Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 ФБУН НИИ эпидемиологии и микробиологии имени Пастера, Санкт-Петербург, Россия
Трансплантация гемопоэтических стволовых клеток (ТГСК) часто сопровождается инфекционными осложнениями. Целью настоящего исследования была сравнительная оценка состава факультативно-анаэробных представителей микробиоты полости носа и его придаточных пазух при синусите, который нередко развивается у иммунокомпромиссных пациентов после интенсивной химио- и антибиотикотерапии и трансплантации гемопоэтических клеток (ТГСК).
Материалы и методы
В исследовании участвовали 194 пациента с различными миело- и лимфопролиферативными заболеваниями в возрасте от 1 до 62 лет, проходившие интенсивную химиотерапию и аллогенную ТГСК. При наличии клинических показаний у пациентов забирали биоматериал (смывы из околоносовых пазух и/или назальные мазки) в сроки от -100 до +180 суток после аллогенной ТГСК. Исследовано 124 образца пунктатов верхнечелюстных пазух от 97 пациентов и 973 мазка-соскоба из полости носа. Посев биоматериала и выделение микроорганизмов проводили классическими бактериологическими методами. Чувствительность клинических изолятов к антибиотикам определяли диско-диффузионным методом. Интерпретацию результатов чувствительности осуществляли согласно критериям EUCAST.
Результаты
В биоматериале из полости носа и околоносовых пазух наиболее часто высевали S.epidermidis – 34,7% (377/1097); S.viridans – 2,2% (24/1097); S. aureus – 1,91% (21/1097); Klebsiella spp – 1% (11/1097). Частота выявления S.epidermidis и S.viridans была минимальной в младшей возрастной группе (до 5 лет) и возрастала в группах от 15 лет и выше. Глубокое подавление роста S.epidermidis отмечалось (в особенности – в околоносовых синусах) в течение 1-го мес. после ТГСК на фоне массивной антибиотикотерапии. Отмечена высокая частота выявления Klebsiella spp в материале из синусов в поздние сроки (2-3 мес.) после ТГСК при малой частоте выявления в материале из полости носа (в среднем 16,3% против 2.1%, р=2×10^14). Кроме того, мы оценили частоту высеваемости бактерий в сроки +30 сут. от постановки диагноза синусита. При этом была выявлена повышенная частота выделения Pseudomonas spp (1/378 vs 7/217) в материале из придаточных пазух.
Заключение
Бактериологические исследование материала из гайморовых пазух имеет ограниченную ценность в течение 1-го мес. после ТГСК в связи с массивной антибиотикотерапией, которая сопровождается селекцией резистентных штаммов Klebsiella spp, Pseudomonas spp, E.coli, S.aureus, главным образом – в сроки 2 и более мес. после ТГСК.
Ключевые слова
Tрансплантация гемопоэтических стволовых клеток, околоносовые пазухи, микробиота, антибиотикорезистентность.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28547" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-36-42" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-36-42" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28550" ["VALUE"]=> array(2) { ["TEXT"]=> string(429) "<p>Oleg I. Dolgov<sup>1</sup>, Sergey A. Karpishchenko<sup>1</sup>, Ekaterina S. Utimisheva<sup>1</sup>, Diana A. Grigoryanz<sup>1</sup>, Anna A. Spiridonova<sup>1,2</sup>, Ivan S. Moiseev<sup>1</sup>, Ludmila S. Zubarovskaya<sup>1</sup>, Alexei B. Chukhlovin<sup>1</sup>, Alexander D. Kulagin<sup>1</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(309) "Oleg I. Dolgov1, Sergey A. Karpishchenko1, Ekaterina S. Utimisheva1, Diana A. Grigoryanz1, Anna A. Spiridonova1,2, Ivan S. Moiseev1, Ludmila S. Zubarovskaya1, Alexei B. Chukhlovin1, Alexander D. Kulagin1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28551" ["VALUE"]=> array(2) { ["TEXT"]=> string(693) "<p><sup>1</sup> Pavlov University, St. Petersburg, Russia<br> <sup>2</sup> St. Petersburg Pasteur Institute, St. Petersburg, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Oleg I. Dolgov, Department of Otorhinolaryngology, Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia<br> Phone: +7 (921) 845-03-51<br> E-mail: oidolgov@yandex.ru</p><br> <p><b>Citation:</b> Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(573) "1 Pavlov University, St. Petersburg, Russia
2 St. Petersburg Pasteur Institute, St. Petersburg, Russia
Correspondence:
Dr. Oleg I. Dolgov, Department of Otorhinolaryngology,
Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (921) 845-03-51
E-mail: oidolgov@yandex.ru
Citation: Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28552" ["VALUE"]=> array(2) { ["TEXT"]=> string(3275) "<p style="text-align: justify;"> Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT). </p> <h3>Materials and methods</h3> <p style="text-align: justify;"> The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria. </p> <h3>Results</h3> <p style="text-align: justify;"> In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); <i>S.viridans</i> (2.2%, 24/1097); <i>S. aureus</i> (1.91%, 21/1097); <i>Klebsiella spp</i> (1%, 11/1097). Detection frequency of <i>S.epidermidis</i> and <i>S.viridans</i> was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of <i>S.epidermidis</i> growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of <i>Klebsiella spp</i> detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% <i>vs</i> 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of <i>Pseudomonas spp</i> isolation (1/378 <i>vs </i>7/217) was revealed in the material from paranasal sinuses. </p> <h3>Conclusion</h3> <p style="text-align: justify;"> Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of <i>Klebsiella spp, Pseudomonas spp, E. coli, S. aureus</i>, mainly at the terms of >2 months after HSCT. </p> <h2>Keywords</h2> <p style="text-align: justify;"> Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2977) "Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT).
Materials and methods
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria.
Results
In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); S.viridans (2.2%, 24/1097); S. aureus (1.91%, 21/1097); Klebsiella spp (1%, 11/1097). Detection frequency of S.epidermidis and S.viridans was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of S.epidermidis growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of Klebsiella spp detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% vs 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of Pseudomonas spp isolation (1/378 vs 7/217) was revealed in the material from paranasal sinuses.
Conclusion
Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of Klebsiella spp, Pseudomonas spp, E. coli, S. aureus, mainly at the terms of >2 months after HSCT.
Keywords
Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28548" ["VALUE"]=> string(89) "Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(89) "Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28549" ["VALUE"]=> string(4) "2788" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2788" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28553" ["VALUE"]=> string(4) "2796" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2796" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(10) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28550" ["VALUE"]=> array(2) { ["TEXT"]=> string(429) "<p>Oleg I. Dolgov<sup>1</sup>, Sergey A. Karpishchenko<sup>1</sup>, Ekaterina S. Utimisheva<sup>1</sup>, Diana A. Grigoryanz<sup>1</sup>, Anna A. Spiridonova<sup>1,2</sup>, Ivan S. Moiseev<sup>1</sup>, Ludmila S. Zubarovskaya<sup>1</sup>, Alexei B. Chukhlovin<sup>1</sup>, Alexander D. Kulagin<sup>1</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(309) "Oleg I. Dolgov1, Sergey A. Karpishchenko1, Ekaterina S. Utimisheva1, Diana A. Grigoryanz1, Anna A. Spiridonova1,2, Ivan S. Moiseev1, Ludmila S. Zubarovskaya1, Alexei B. Chukhlovin1, Alexander D. Kulagin1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(309) "Oleg I. Dolgov1, Sergey A. Karpishchenko1, Ekaterina S. Utimisheva1, Diana A. Grigoryanz1, Anna A. Spiridonova1,2, Ivan S. Moiseev1, Ludmila S. Zubarovskaya1, Alexei B. Chukhlovin1, Alexander D. Kulagin1
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28552" ["VALUE"]=> array(2) { ["TEXT"]=> string(3275) "<p style="text-align: justify;"> Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT). </p> <h3>Materials and methods</h3> <p style="text-align: justify;"> The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria. </p> <h3>Results</h3> <p style="text-align: justify;"> In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); <i>S.viridans</i> (2.2%, 24/1097); <i>S. aureus</i> (1.91%, 21/1097); <i>Klebsiella spp</i> (1%, 11/1097). Detection frequency of <i>S.epidermidis</i> and <i>S.viridans</i> was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of <i>S.epidermidis</i> growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of <i>Klebsiella spp</i> detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% <i>vs</i> 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of <i>Pseudomonas spp</i> isolation (1/378 <i>vs </i>7/217) was revealed in the material from paranasal sinuses. </p> <h3>Conclusion</h3> <p style="text-align: justify;"> Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of <i>Klebsiella spp, Pseudomonas spp, E. coli, S. aureus</i>, mainly at the terms of >2 months after HSCT. </p> <h2>Keywords</h2> <p style="text-align: justify;"> Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2977) "Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT).
Materials and methods
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria.
Results
In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); S.viridans (2.2%, 24/1097); S. aureus (1.91%, 21/1097); Klebsiella spp (1%, 11/1097). Detection frequency of S.epidermidis and S.viridans was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of S.epidermidis growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of Klebsiella spp detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% vs 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of Pseudomonas spp isolation (1/378 vs 7/217) was revealed in the material from paranasal sinuses.
Conclusion
Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of Klebsiella spp, Pseudomonas spp, E. coli, S. aureus, mainly at the terms of >2 months after HSCT.
Keywords
Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(2977) "Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT).
Materials and methods
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria.
Results
In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); S.viridans (2.2%, 24/1097); S. aureus (1.91%, 21/1097); Klebsiella spp (1%, 11/1097). Detection frequency of S.epidermidis and S.viridans was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of S.epidermidis growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of Klebsiella spp detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% vs 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of Pseudomonas spp isolation (1/378 vs 7/217) was revealed in the material from paranasal sinuses.
Conclusion
Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of Klebsiella spp, Pseudomonas spp, E. coli, S. aureus, mainly at the terms of >2 months after HSCT.
Keywords
Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28547" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-36-42" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-36-42" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-36-42" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28548" ["VALUE"]=> string(89) "Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(89) "Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(89) "Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28551" ["VALUE"]=> array(2) { ["TEXT"]=> string(693) "<p><sup>1</sup> Pavlov University, St. Petersburg, Russia<br> <sup>2</sup> St. Petersburg Pasteur Institute, St. Petersburg, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Oleg I. Dolgov, Department of Otorhinolaryngology, Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia<br> Phone: +7 (921) 845-03-51<br> E-mail: oidolgov@yandex.ru</p><br> <p><b>Citation:</b> Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(573) "1 Pavlov University, St. Petersburg, Russia
2 St. Petersburg Pasteur Institute, St. Petersburg, Russia
Correspondence:
Dr. Oleg I. Dolgov, Department of Otorhinolaryngology,
Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (921) 845-03-51
E-mail: oidolgov@yandex.ru
Citation: Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(573) "1 Pavlov University, St. Petersburg, Russia
2 St. Petersburg Pasteur Institute, St. Petersburg, Russia
Correspondence:
Dr. Oleg I. Dolgov, Department of Otorhinolaryngology,
Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (921) 845-03-51
E-mail: oidolgov@yandex.ru
Citation: Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28544" ["VALUE"]=> array(2) { ["TEXT"]=> string(566) "<p>Олег И. Долгов<sup>1</sup>, Сергей А. Карпищенко<sup>1</sup>, Екатерина С. Утимишева<sup>1</sup>, Диана А. Григорьянц<sup>1</sup>, Анна А. Спиридонова<sup>1,2</sup>, Иван С. Моисеев<sup>1</sup>, Людмила С. Зубаровская<sup>1</sup>, Алексей Б. Чухловин<sup>1</sup>, Александр Д. Кулагин<sup>1</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(446) "Олег И. Долгов1, Сергей А. Карпищенко1, Екатерина С. Утимишева1, Диана А. Григорьянц1, Анна А. Спиридонова1,2, Иван С. Моисеев1, Людмила С. Зубаровская1, Алексей Б. Чухловин1, Александр Д. Кулагин1
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(446) "Олег И. Долгов1, Сергей А. Карпищенко1, Екатерина С. Утимишева1, Диана А. Григорьянц1, Анна А. Спиридонова1,2, Иван С. Моисеев1, Людмила С. Зубаровская1, Алексей Б. Чухловин1, Александр Д. Кулагин1
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28542" ["VALUE"]=> string(22) "02/06/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "02/06/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "02/06/2022 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28543" ["VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "03/18/2022 12:00:00 am" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28546" ["VALUE"]=> array(2) { ["TEXT"]=> string(5126) "<p style="text-align: justify;"> Трансплантация гемопоэтических стволовых клеток (ТГСК) часто сопровождается инфекционными осложнениями. Целью настоящего исследования была сравнительная оценка состава факультативно-анаэробных представителей микробиоты полости носа и его придаточных пазух при синусите, который нередко развивается у иммунокомпромиссных пациентов после интенсивной химио- и антибиотикотерапии и трансплантации гемопоэтических клеток (ТГСК). </p> <h3>Материалы и методы</h3> <p style="text-align: justify;"> В исследовании участвовали 194 пациента с различными миело- и лимфопролиферативными заболеваниями в возрасте от 1 до 62 лет, проходившие интенсивную химиотерапию и аллогенную ТГСК. При наличии клинических показаний у пациентов забирали биоматериал (смывы из околоносовых пазух и/или назальные мазки) в сроки от -100 до +180 суток после аллогенной ТГСК. Исследовано 124 образца пунктатов верхнечелюстных пазух от 97 пациентов и 973 мазка-соскоба из полости носа. Посев биоматериала и выделение микроорганизмов проводили классическими бактериологическими методами. Чувствительность клинических изолятов к антибиотикам определяли диско-диффузионным методом. Интерпретацию результатов чувствительности осуществляли согласно критериям EUCAST. </p> <h3>Результаты</h3> <p style="text-align: justify;"> В биоматериале из полости носа и околоносовых пазух наиболее часто высевали <i>S.epidermidis</i> – 34,7% (377/1097); <i>S.viridans</i> – 2,2% (24/1097); <i>S. aureus</i> – 1,91% (21/1097); <i>Klebsiella spp</i> – 1% (11/1097). Частота выявления <i>S.epidermidis</i> и <i>S.viridans</i> была минимальной в младшей возрастной группе (до 5 лет) и возрастала в группах от 15 лет и выше. Глубокое подавление роста <i>S.epidermidis</i> отмечалось (в особенности – в околоносовых синусах) в течение 1-го мес. после ТГСК на фоне массивной антибиотикотерапии. Отмечена высокая частота выявления <i>Klebsiella spp</i> в материале из синусов в поздние сроки (2-3 мес.) после ТГСК при малой частоте выявления в материале из полости носа (в среднем 16,3% против 2.1%, р=2×10^14). Кроме того, мы оценили частоту высеваемости бактерий в сроки +30 сут. от постановки диагноза синусита. При этом была выявлена повышенная частота выделения <i>Pseudomonas spp</i> (1/378 <i>vs </i>7/217) в материале из придаточных пазух. </p> <h3>Заключение</h3> <p style="text-align: justify;"> Бактериологические исследование материала из гайморовых пазух имеет ограниченную ценность в течение 1-го мес. после ТГСК в связи с массивной антибиотикотерапией, которая сопровождается селекцией резистентных штаммов <i>Klebsiella spp, Pseudomonas spp, E.coli, S.aureus</i>, главным образом – в сроки 2 и более мес. после ТГСК. </p> <h2>Ключевые слова</h2> <p style="text-align: justify;"> Tрансплантация гемопоэтических стволовых клеток, околоносовые пазухи, микробиота, антибиотикорезистентность. </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(4836) "Трансплантация гемопоэтических стволовых клеток (ТГСК) часто сопровождается инфекционными осложнениями. Целью настоящего исследования была сравнительная оценка состава факультативно-анаэробных представителей микробиоты полости носа и его придаточных пазух при синусите, который нередко развивается у иммунокомпромиссных пациентов после интенсивной химио- и антибиотикотерапии и трансплантации гемопоэтических клеток (ТГСК).
Материалы и методы
В исследовании участвовали 194 пациента с различными миело- и лимфопролиферативными заболеваниями в возрасте от 1 до 62 лет, проходившие интенсивную химиотерапию и аллогенную ТГСК. При наличии клинических показаний у пациентов забирали биоматериал (смывы из околоносовых пазух и/или назальные мазки) в сроки от -100 до +180 суток после аллогенной ТГСК. Исследовано 124 образца пунктатов верхнечелюстных пазух от 97 пациентов и 973 мазка-соскоба из полости носа. Посев биоматериала и выделение микроорганизмов проводили классическими бактериологическими методами. Чувствительность клинических изолятов к антибиотикам определяли диско-диффузионным методом. Интерпретацию результатов чувствительности осуществляли согласно критериям EUCAST.
Результаты
В биоматериале из полости носа и околоносовых пазух наиболее часто высевали S.epidermidis – 34,7% (377/1097); S.viridans – 2,2% (24/1097); S. aureus – 1,91% (21/1097); Klebsiella spp – 1% (11/1097). Частота выявления S.epidermidis и S.viridans была минимальной в младшей возрастной группе (до 5 лет) и возрастала в группах от 15 лет и выше. Глубокое подавление роста S.epidermidis отмечалось (в особенности – в околоносовых синусах) в течение 1-го мес. после ТГСК на фоне массивной антибиотикотерапии. Отмечена высокая частота выявления Klebsiella spp в материале из синусов в поздние сроки (2-3 мес.) после ТГСК при малой частоте выявления в материале из полости носа (в среднем 16,3% против 2.1%, р=2×10^14). Кроме того, мы оценили частоту высеваемости бактерий в сроки +30 сут. от постановки диагноза синусита. При этом была выявлена повышенная частота выделения Pseudomonas spp (1/378 vs 7/217) в материале из придаточных пазух.
Заключение
Бактериологические исследование материала из гайморовых пазух имеет ограниченную ценность в течение 1-го мес. после ТГСК в связи с массивной антибиотикотерапией, которая сопровождается селекцией резистентных штаммов Klebsiella spp, Pseudomonas spp, E.coli, S.aureus, главным образом – в сроки 2 и более мес. после ТГСК.
Ключевые слова
Tрансплантация гемопоэтических стволовых клеток, околоносовые пазухи, микробиота, антибиотикорезистентность.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(4836) "Трансплантация гемопоэтических стволовых клеток (ТГСК) часто сопровождается инфекционными осложнениями. Целью настоящего исследования была сравнительная оценка состава факультативно-анаэробных представителей микробиоты полости носа и его придаточных пазух при синусите, который нередко развивается у иммунокомпромиссных пациентов после интенсивной химио- и антибиотикотерапии и трансплантации гемопоэтических клеток (ТГСК).
Материалы и методы
В исследовании участвовали 194 пациента с различными миело- и лимфопролиферативными заболеваниями в возрасте от 1 до 62 лет, проходившие интенсивную химиотерапию и аллогенную ТГСК. При наличии клинических показаний у пациентов забирали биоматериал (смывы из околоносовых пазух и/или назальные мазки) в сроки от -100 до +180 суток после аллогенной ТГСК. Исследовано 124 образца пунктатов верхнечелюстных пазух от 97 пациентов и 973 мазка-соскоба из полости носа. Посев биоматериала и выделение микроорганизмов проводили классическими бактериологическими методами. Чувствительность клинических изолятов к антибиотикам определяли диско-диффузионным методом. Интерпретацию результатов чувствительности осуществляли согласно критериям EUCAST.
Результаты
В биоматериале из полости носа и околоносовых пазух наиболее часто высевали S.epidermidis – 34,7% (377/1097); S.viridans – 2,2% (24/1097); S. aureus – 1,91% (21/1097); Klebsiella spp – 1% (11/1097). Частота выявления S.epidermidis и S.viridans была минимальной в младшей возрастной группе (до 5 лет) и возрастала в группах от 15 лет и выше. Глубокое подавление роста S.epidermidis отмечалось (в особенности – в околоносовых синусах) в течение 1-го мес. после ТГСК на фоне массивной антибиотикотерапии. Отмечена высокая частота выявления Klebsiella spp в материале из синусов в поздние сроки (2-3 мес.) после ТГСК при малой частоте выявления в материале из полости носа (в среднем 16,3% против 2.1%, р=2×10^14). Кроме того, мы оценили частоту высеваемости бактерий в сроки +30 сут. от постановки диагноза синусита. При этом была выявлена повышенная частота выделения Pseudomonas spp (1/378 vs 7/217) в материале из придаточных пазух.
Заключение
Бактериологические исследование материала из гайморовых пазух имеет ограниченную ценность в течение 1-го мес. после ТГСК в связи с массивной антибиотикотерапией, которая сопровождается селекцией резистентных штаммов Klebsiella spp, Pseudomonas spp, E.coli, S.aureus, главным образом – в сроки 2 и более мес. после ТГСК.
Ключевые слова
Tрансплантация гемопоэтических стволовых клеток, околоносовые пазухи, микробиота, антибиотикорезистентность.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28545" ["VALUE"]=> array(2) { ["TEXT"]=> string(435) "<p><sup>1</sup> Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия<br> <sup>2</sup> ФБУН НИИ эпидемиологии и микробиологии имени Пастера, Санкт-Петербург, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(393) "1 Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 ФБУН НИИ эпидемиологии и микробиологии имени Пастера, Санкт-Петербург, Россия
1 Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 ФБУН НИИ эпидемиологии и микробиологии имени Пастера, Санкт-Петербург, Россия
Introduction
The development of solid organ transplantation and the subsequent lifelong immunosuppressive therapy (IST) is naturally accompanied by the development of complications associated with a specific spectrum of infections, organ dysfunctions, and also with the occurrence of tumor diseases of various etiology. Increasing the number of patients who underwent transplantation of kidneys, liver, heart, lungs, etc. results in the number of patients with post-transplant malignant neoplasms [1]. The most common of them are neoplastic diseases of the hemopoietic system and, mainly, various malignant lymphoproliferative diseases. Even separate forms of these types of tumors which is associated with previous long-term immunosuppression are distinguished in the modern WHO classification [2].
The risk of developing post-transplant lymphoproliferative disease (PTLD) increases by 20-120% in patients after solid organ transplantation compared with the general population and depends on the intensity of IST. PTLD was first described in 1968 by Doak P. B. in two patients after cadaveric kidney transplantation and IST with azathioprine and prednisolone [3]. The term PTLD was introduced by T. E. Starzl in 1984 [4]. The role of the Epstein-Barr virus (EBV) in the pathogenesis of PTLD was described in 1981 [5]. The developing of this disease most frequently associated with solid organ transplantation like heart, lung, intestine and multi-organ transplantation, while this complication develops less frequently in kidney and liver recipients [6, 7]. There was no increase in the incidence of PTLD when cyclosporine was used in comparison with therapy with azathioprine in combination with glucocorticosteroids. Tacrolimus also increases the risk of this complication [7]. Immunosuppressive therapy with antithymocyte globulin (ATG) increases the risk of PTLD within the first year after solid organ transplantation, and no such dependence was found when antibodies to the IL-2 receptor were used [7]. It has been established that in the pathogenesis of PTLD, the presence of certain human leukocyte antigens (HLA) in a patient is important. If alleles HLA-A26 and HLA-B38 are detected in a recipient, the risk of PTLD development increases, while donor haplotypes HLA-A1, HLA-B8, and HLA-DR3 were identified as factors in which this complication develops less frequently [8]. Other studies have identified an increased risk of PTLD in a recipient with HLA-A2, HLA-A11, HLA-B5, HLA-B18, HLA-B21, and HLA-B35 [9, 10].
The clinical manifestations of PTLD are often nonspecific. Involvement of the gastrointestinal (GI) tract, lungs, skin, bone marrow, and central nervous system (CNS) is common [11-15]. CNS involvement is present in about 10-15% of all PTLD cases [11]. B-symptoms such as pyrexia, sweating and weight loss are also common. Damage to the transplanted organ is noted in about a third of all PTLD cases [13]. According to the WHO classification 2017, there are the following types of PTLD: early lesions (plasmacytic hyperplasia, infectious mononucleosis, and florid follicular hyperplasia) – 5% of all PTLD, polymorphic PTLD – 15-20%, monomorphic B-cell neoplasm (diffuse large B-cell lymphoma, Burkitt lymphoma, plasma cell myeloma and other) – more than 70% of all PTLD, monomorphic T/NK-cell neoplasms PTLD (peripheral T-cell lymphoma and other) – less than 5%, and classic Hodgkin lymphoma PTLD – less than 5% [2].
The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. Due to the clinical and pathological heterogeneity of PTLD (type of transplant, risk of rejection and concomitant diseases, tumor burden, etc.), there is no standardized approach to treatment. Nevertheless, the key approach is the reduction of IST: complete cancellation or partial (by 50-75%) reduction the dose of immunosuppressive drugs to prevent rejection of the transplanted organ. In this case, the response is achieved in about half of the patients, but long-term remissions are rare [12, 14-16]. Other methods that can be used in the treatment of PTLD are monoclonal antibodies to the CD20 antigen (rituximab) as monotherapy or in combination with chemotherapy, surgery, and radiation therapy. In the event that the development of PTLD is associated with EBV infection, antiviral therapy (intravenous immunoglobulins) and/or EBV-specific T-lymphocytes are used, autologous or allogeneic hematopoietic stem cells transplantation are used less often as a consolidating treatment [11, 13, 14, 16.17]. Overall survival of patients after PTLD therapy has significantly improved in recent years, by the using of monoclonal antibodies. Mortality rate earlier was reached 50-70%, nowadays the 3-year overall survival rate is 60-70%, according published studies in recent years [7, 13, 14].
The role of allogeneic hematopoietic stem cells (allo-HSCT) transplantation in PTLD therapy after solid organ transplantation has not been determined. The use of high-dose chemotherapy can be accompanied by high toxicity for the transplanted organ. Graft-versus-host disease (GVHD), which develops after allo-HSCT, can contribute to the rejection of a transplanted solid organ. And the presence of a solid organ transplant before allo-HSCT may increase the probability of rejection of hematopoietic stem cells. Only a few successful clinical cases of allo-HSCT in PTLD after solid organ transplantation have been described [1, 18-20].
The aim of this work: to present a clinical case of a patient in whom transplantation of an allogeneic cadaveric kidney was complicated by the development of PTLD, which was initially successfully treated, but due to the ongoing IST, a relapse was established, which required HSCT from a haploidentical donor. Clinical case is presented with the consent of the patient.
Clinical case description
Patient B., female, the disease manifested at the age of 9 years, in 1996 with proteinuria (3 g/day) and increased arterial pressure up to 160/90 mm Hg. Acute glomerulonephritis was diagnosed, and prednisolone therapy was started. In 1998, the diagnosis of mesangioproliferative glomerulonephritis was confirmed by histological examination of a kidney biopsy. Progression to the terminal stage of chronic renal failure (stage 5) was documented in 2003, hemodialysis was started, with arteriovenous fistula arranged. Transplantation of allogeneic cadaveric kidney was performed at the N. V. Sklifosovsky Research Institute for Emergency Medicine in April 2011. Delayed recovery of renal transplant function was noted; hemodialysis was carried out within a month after the organ transplantation. Tacrolimus, mycophenolate mofetil, methylprednisolone were applied as immunosuppressive therapy. Blood creatinine level in the post-transplant period was 110-130 μmol/L, glomerular filtration rate (GFR), according to the CKD-EPI formula, was 48-61 ml/min/1.73 m2. Due to the pregnancy planning, mycophenolate mofetil was replaced by azathioprine in 2016. Pancytopenia was detected in June 2017, but the dose of immunosuppressive drugs was not reduced. Since the end of July 2017, the patient had febrile body temperature, decreasing body weight, dry cough, increased abdominal volume, and irregularity in the menstrual cycle, but the patient did not seek medical asssistance.
In August 2017 the examination revealed proteinuria 2.3 g/l, hypoalbuminemia 28 g/l, high level of blood creatinine (214 μmol/l) and C-reactive protein (115 mg/dl), an increased LDH activity to 923 U/l, ESR up to 70 mm/h, an increased IgM content in the blood (1288 mg/dl), mainly, due to IgMλ. Pancytopenia still persisted (leukocytes 1.9×109/l, platelets 90×109/l). Antibiotic therapy was carried out for suspected infection, azathioprine was canceled. Hepatosplenomegaly was revealed on the CT examination of abdominal organs. Given these findings, lymphoproliferative disease was suggested, thus requiring special examination.
The patient was examined at National Research Center for Hematology at 23.08.2017. Infiltrative-ulcerative defects of the gastric mucosa were found during esophagogastroduodenoscopy. The data of histological and immunohistochemical studies of gastric biopsy revealed the substrate of extranodal diffuse large B-cell lymphoma (tumor cells monomorphically expressed CD 20). In addition, the data of histological and immunohistochemical studies of the bone marrow also was determined: interstitial-small-focal B-cell infiltration with the presence of clusters of large CD 20+ cells, intravascular foci of small CD 20+ B-cells. The expression of EBER (EBV-encoded RNA) was not detected, but the virus replication was detected in blood. Paraprotein M lambda, 21.3 g/l; Bens-Jones protein lambda 0.35 g/l was revealed in blood serum by immunochemistry. Hyperpdiloid karyotype and complex cytogenetic rearrangements involving chromosomes 3, 7, 4, 9, 10, 14, 15, 17, 18 were registered by standard cytogenetic study of the bone marrow samples. According to CT scan, hepatosplenomegaly was determined: the vertical size of the liver was 23.5 cm, the size of the spleen was 160×60×235 mm. Based on the obtained data, the diagnosis of PTLD was specified as a diffuse large B-cell lymphoma (PTLD-DLBCL) associated with immunosuppressive therapy, with involvement of liver, spleen, stomach and bone marrow.
Despite the presence of a transplanted organ, taking into the variant of the disease and the generally accepted practice of managing such patients, the IST was reduced: methylprednisolone and tacrolimus were completely canceled since 24.08.2017.
From 26.08.2017 to 30.08.2017, a pre-phase with dexamethasone and cyclophosphamide was carried out and a positive trend was noted as decreasing size of the liver and spleen. From 31.08.2017 to 05.09.2017, the 1st course of CHOD protocol in combination with rituximab (600 mg) was administered (total drug doses: cyclophosphamide 1200 mg, doxorubicin 75 mg, vincristine 2 mg, dexamethasone 80 mg). The treatment was complicated by febrile fever, oropharyngeal candidiasis, bilateral pleuropneumonia; the patient underwent massive antimicrobial therapy: imipenem/cilastatin, sodium colistimethate, fluconazole, acyclovir and intravenous immunoglobulin. In addition, the patient developed hypotension (up to 80/50 mm Hg). Subsequent examination revealed adrenal insufficiency, which required administration of hydrocortisone (2.5-5 mg per day). A partial remission of the disease was obtained after first R-CHOD. From 26.09.2017 to 11.01.2018, five R-CHOD courses were performed. A complete remission of PTLD-DLBCL was achieved after second course of R-CHOD as confirmed by PET-CT (Fig. 1).

Figure 1. CT dynamics of internal organs. A, in the debut of PTLD-DLBCL (August 2017); B, first remission of PTLD-DLBCL (January 2018); C, relapse of PTLD-DLBCL (January 2019); D, before haplo-HSCT (May 2019)
Due to the risk of renal transplant rejection, the patient resumed immunosuppressive therapy with tacrolimus (2 mg/day) and prednisolone (5 mg/day) after completing chemotherapy (6 courses), since April 2018. In December 2018, 10 months after the completion of therapy for PTLD-DLBCL, the patient had a febrile episode of up to 40°C. Ultrasound examination revealed a focal lesion in the liver. At that moment, no other signs of PTLD progression (based on bone marrow and gastric biopsies) were present. However, a month later, in January 2019, the febrile fever was again observed. The patient was admitted to the hospital in an extremely severe condition with signs of septic shock, bilateral pneumonia with respiratory failure, and evolving acute renal injury (blood creatinine levels reached 522 μmol/l). At the intensive care unit, the patient underwent massive antimicrobial therapy (meropenem, linezolid, sodium colistimethate, fluconazole, acyclovir), and hemodiafiltration were performed, with immunosuppressive therapy still continued. Additional examination revealed an increasing size of the liver (vertical size 24 cm) and spleen (121×54×175 mm) (Fig. 1). B-cell clonality was revealed in the gastric tissue biopsy, infiltration with tumor CD20+ cells was noted in the bone marrow biopsy, monoclonal secretion of M lambda in serum was determined in blood (5.3 g/l), a trace amount of the Bence-Jones protein lambda was detected in the urine, standard cytogenetic study of bone marrow and gastric tissue biopsies no mitosis was detected. Thus, after 11 months of achievement of PET-CT-negative remission and 9 months after the resumption of the IST, a relapse of PTLD-DLBCL was documented.
The severity of the patient's condition was due to both septic condition and emerging relapse of the disease, including specific liver damage. As a result, severe coagulation disorders developed, with re-appearing signs of adrenal insufficiency (decreased concentration of cortisol in blood serum: 90.47 nmol/L (reference range of 185-624 nmol/L), which required administration of hydrocortisone (2.5-5 mg per day), blood transfusions and management of blood clotting problems.
Due to PTLD-DLBCL relapse and severe infectious complications, despite presence of a transplanted organ, the IST was canceled 01.05.2019, and the antitumor effect was not achieved again. The patient's condition remained extremely serious, and according to vital indications, from 01.11.2019 to 15.01.2019 the pre-phase therapy with cyclophosphamide and dexamethasone was started. Positive clinical dynamics was noted, i.e., normalization of body temperature and decrease in the liver and spleen size few days after pre-phase therapy.
Thereafter, a modified course of chemotherapy with cytarabine (=4 g) + etoposide (∑ = 400 mg) combined with lenalidomide (∑ = 30 mg) was carried out from 16.01.2019 to 17.01.2019. Lenalidomide was included in the treatment, according to the previously published data on improvement of overall and progression-free survival when using it in the patients with DLBCL [21, 22]. At the control examination (08.02.2019) we have revealed a decreased size of the liver (vertical size 18 cm) and spleen (115×47×130 mm), complete regression of focal liver lesion, regression of hystological changes in the bone marrow biopsy, and only trace secretion of paraprotein IgM.
Two more courses using cytarabine + etoposide + lenalidomide were performed from 15.02.2019 to 06.05.2019. The second PET-CT-negative remission of PTLD-DLBCL was achieved (Fig. 1).
Thus, the young patient re-achieved PET-СТ negative remission of PTLD-DLBCL, and still required resumption of IST to prevent kidney transplant rejection, which would entail another relapse of the disease. Program therapy for patients in the second remission of the DLBCL implies to consolidate remission by autologous hematopoietic stem cell transplantation. However, our patient would have to return again immunosuppressive therapy to prevent kidney transplant rejection. Therefore, we decided to perform allo-HSCT to induce tolerance of the donor-derived immune cells to the transplanted kidney. The patient didn’t have a fully matched related or unrelated donor, since the HSCT was planned from a related haploidentical (haplo-HSCT) donor (mother), however, with TCRαβ +/CD19+ depletion of the graft. The choice of such a transplant approach was determined by the fact that it does not use long-term (minimum 6 months) immunosuppressive therapy. The last injection of IST drugs (tocilizumab and abatacept) was administered on day +30 after haplo-HSCT with TCRαβ+/CD19+ depletion. Following HLA typing of the patient and her mother was performed, HLA-B18 was identified in the HLA genotype of the patient. This allele is associated with increased incidence of PTLD. The donor was diagnosed with microcytic hypochromic anemia (Hb 101 g/L), she was observed for a long time at a hematologist with a diagnosis of iron deficiency anemia and was treated with iron preparations.
Pre-transplant conditioning regimen included: treosulfan (∑ = 45 g) + melphalan (∑ = 100 mg) + fludarabine (∑ = 225 mg). Haplo-HSCT was performed 14.05.2019 the number of CD34 + cells in the graft was 10.8×106/kg, the number of TCRαβ + lymphocytes was 271.5×103/kg. GVHD prophylaxis consisted of rituximab (∑ = 170 mg) + bortezomib (∑ = 4.2 mg) + tocilizumab (∑ = 460 g) + abatacept (∑ = 1740 mg), the patient did not receive any other immunosuppressive therapy. The early post-transplant period was complicated by febrile fever, mucositis, and neutropenic enterocolitis, positive effect was obtained on carbapenem therapy. The recovery of leukocytes was on day +13 after haplo-HSCT (3.0×109/l).
The patient was discharged from the hospital on day + 21 after haplo-HSCT. There were no problems with the functioning of the renal graft, during conditioning regimen and in the early post-transplant period too.
Early control examinations after haplo-HSCT (+1, +2 months) has shown bone marrow remission of the disease with normal function of erythropoiesis and 100% donor chimerism. However, despite the absence of ABO incompatibility between the patient and the donor (the patient and the donor have the same blood group: 0 (I) Rh + CcDee with differences in the MN system), 95% of erythrocytes had patient’s phenotype. Meanwhile, severe anemia persisted for 6 months after haplo-HSCT, requiring monthly blood transfusions. Therefore, additional tests were performed to search for possible causes of anemia (Table 1). Initially, there were signs of either iron deficient anemia, or anemia of chronic disease (25.06.2019). Parvovirus B19-associated anemia was excluded. However, in September 2019, the signs of microcytic hypochromic anemia worsened, there were a decrease in TIBC, LIBC and transferrin, along with increased ferritin level and normal serum iron content. Mild iron overload was determined by MRI. The clinical diagnosis was considered as follows: anemia of chronic conditions in a patient with transplanted kidney and multiple complications associated with therapy of the disease.
Table 1. Post-transplant monitoring of anemia
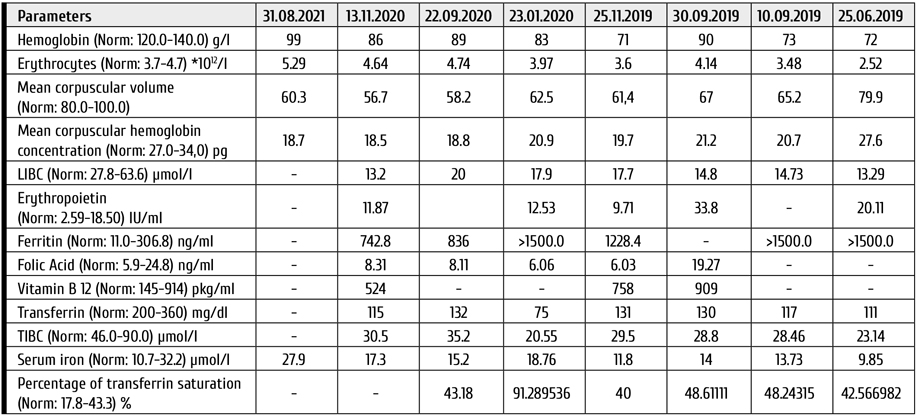

Figure 2. A: Slight increase in the light and heavy fractions of erythrocytes (abscissa, relative cell density, g/cm3). The average density of red blood cells is within normal limits. (B, C): Osmotic fragility (OFT) is altered before and after incubation (abscissa, % of NaCl in saline for RBC incubation)
Given the fact that before haplo-HSCT patient didn’t have any signs of microcytic hypochromic anemia, we have performed hemoglobin electrophoresis, density distribution of erythrocytes, and the osmotic fragility test (OFT) (Fig. 2). The content of the fraction of normal hemoglobin A was 95.9% and hemoglobin A2 was 4.1%.
According to these studies, clinical thalassemia was suspected, and during DNA diagnostic test was found heterozygous carriage of beta (+) – thalassemic mutation IVS1 + 5 G> T. A genetic study of an archived sample of the patient's bone marrow before haplo-HSCT was carried out: thalassemic mutation was not detectable. Thus, the patient was diagnosed with a heterozygous form of beta-thalassemia, which was a consequence of the reconstitution of donor hematopoiesis.
The examination of the haploidentical related donor, the mother, was carried out, and again, as before donation, moderate microcytic hypochromic anemia was revealed. A genetic study was performed, and it was confirmed that the mother is also a heterozygous carrier of the beta (+) – thalassemic mutation IVS1 + 5 G> T.
At the present time, 2.5 years have passed after haplo-HSCT, and 10.5 years after transplantation of allogeneic cadaveric kidney. In this case, the patient had a short course of immunosuppressive drugs (rituximab, bortezomib, tocilizumab, abatacept) only at the early post-transplant period, ceasing the IST at later terms. Immunological tolerance has been achieved: the patient has no signs of GVHD, and the kidney transplant is functioning normally. The patient has PET-CT-negative remission of PTLD-DLBCL. Despite the fact that the patient is a heterozygous carrier of the beta-thalassemia mutation, her primary disease was complicated by the anemia of chronic conditions, which required hemotransfusions for a year after haplo-HSCT. Currently, the patient is transfusion-independent.
Conclusion
Post-transplant lymphoproliferative disease is not such a rare complication after solid organ transplantation, since the immunosuppressive therapy performed increases the risks of developing lymphoid tumors.
We have described for the first time a case of haploidentical HSCT with TCRαβ+/CD19+ graft depletion in a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a transplant of allogeneic cadaveric kidney. In the literature, there are only a few descriptions of allo-HSCT from related or unrelated donors in PTLD after solid organ transplantation, and haploidentical HSCT with TCRαβ+/CD19+ graft depletion has not been previously described. This transplant mode was chosen due to absence of HLA-identical donors, second remission of PTLD-DLBCL, and the fact that the previous relapse was associated with resumption of immunosuppressive therapy (IST) for the transplanted kidney. Haploidentical HSCT with TCRαβ+/CD19+ depletion was performed, since the duration of immunosuppressive therapy is only one month after such procedure. The therapy we have chosen in relapsed PTLD-DLBCL allowed us to achieve a second complete PET-CT-negative remission, then was consolidation with haplo-HSCT, which led to development of immunological tolerance of the donor immune system to the previously transplanted cadaveric kidney and withdrawal of IST, which seemed to be the key factor of PTLD. Both kidney transplant and a bone marrow graft show adequate functioning without additional IST.
Another feature of this patient is that the donor for HSCT is a heterozygous carrier of beta-thalassemia mutation IVS1 + 5 G> T, which was not detected during the initial examination, manifesting with serum iron deficiency. There is no doubt that initial detection of beta-thalassemia trait in the donor could influence the donor choice, since the presence of this mutation and the transplanted kidney during the first year complicated the patient's quality of life after haplo-HSCT.
Conflict of interest
None reported.
References
- Doney KC, Mielcarek M, Stewart FM, Frederick R. Hematopoietic cell transplantation after solid organ transplantation. Biol Blood Marrow Transplant. 2015;21(12):2123-2128. doi: 10.1016/j.bbmt.2015.08.004
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J. WHO Classification of tumours of haematopoietic and lymphoid tissues – IARC [Internet]. Revised 4th edition. Lyon: IARC Press. Lyon: IARC Press; 2017.
- Doak PB, Montgomerie JZ, North JDK, Smith F. Reticulum cell sarcoma after renal homotransplantation and azathioprine and prednisone therapy. Br Med J. 1968; 4(5633): 746-748. doi: 10.1136/bmj.4.5633.746
- Starzl TE, Porter KA, Iwatsuki S, Rosenthal JT, Shaw BW, Atchison RW, et al. Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin-steroid therapy. Lancet. 1984; 323 (8377):583-587. doi: 10.1016/S0140-6736(84)90994-2
- Klein G, Purtilo D. Summary: symposium on Epstein-Barr virus-induced lymphoproliferative diseases in immunodeficient patients. Cancer Res. 1981; 41(11 Pt 1): 4302-4304.
- Cockfield SM. Identifying the patient at risk for post-transplant lymphoproliferative disorder. Transplant Infect Dis. 2001; 3: 70-78. doi: 10.1034/j.1399-3062.2001.003002070.x
- Opelz G, Döhler B. Lymphomas after solid organ transplantation: a collaborative transplant study report. Am J Transplant. 2004; 4(2): 222-230. doi: 10.1046/j.1600-6143.2003.00325.x
- Reshef R, Luskin MR, Kamoun M, Heitjan DF, Hadjiliadis D, Goral S, et al. Association of HLA polymorphisms with post-transplant lymphoproliferative disorder in solid-organ transplant recipients. Am J Transplant. 2011;11(4):817-825. doi: 10.1111/j.1600-6143.2011.03454.x
- Pourfarziani V, Einollahi B, Taheri S, Nemati E, Nafar M, Kalantar E, et al. Associations of Human Leukocyte Antigen (HLA) haplotypes with risk of developing lymphoproliferative disorders after renal transplantation. Ann Transplant. 2007;12(4):16-22. PMID: 18344933
- Subklewe M, Marquis R, Choquet S, Leblond V, Garnier JL, Hetzer R, et al. Association of human leukocyte antigen haplotypes with posttransplant lymphoproliferative disease after solid organ transplantation. Transplantation. 2006;82(8):1093-1100.
doi: 10.1097/01.tp.0000235889.05171.12 - Al-Mansour Z, Nelson BP, Evens A.M. Post-transplant lymphoproliferative disease (PTLD): Risk factors, diagnosis, and current treatment strategies. Curr Hematol Malig Rep. 2013; 8(3):173-183. doi: 10.1007/s11899-013-0162-5
- Jagadeesh D, Woda BA, Draper J, Evens A.M. Posttransplant lymphoproliferative disorders: Risk, classification, and therapeutic recommendations. Curr Treat Options Oncol. 2012;13(1):122-136. doi: 10.1007/s11864-011-0177-x
- Ghobrial IM, Habermann TM, Maurer MJ, Geyer SM, Ristow KM, Larson TS et al. Prognostic analysis for survival in adult solid organ transplant recipients with post-transplantation lymphoproliferative disorders. J Clin Oncol. 2005;23(30):7574-7582. doi: 10.1200/JCO.2005.01.0934
- Evens AM, David KA, Helenowski I, Nelson BK, Dixon K, Sheetal M, et al. Multicenter analysis of 80 solid organ transplantation recipients with post-transplantation lymphoproliferative disease: Outcomes and prognostic factors in the modern era. J Clin Oncol. 2010;28(6):1038-1046. doi: 10.1200/JCO.2009.25.4961
- Gavrilina OA, Troitskaya VV, Zvonkov EE, Parovichnikova EN, Galstyan GM, Biryukova LS, et al. EBV-positive central nervous system lymphoproliferative disease associated with immunosuppression after organ transplantation: Long-term remission without chemotherapy. Ter Arkh. 2017;89(7):69-75. (In Russian). doi: 10.17116/terarkh201789769-75
- Reshef R, Vardhanabhuti S, Luskin MR, Heitjan DF, Hadjiliadis D, Goral S, et al. Reduction of immunosuppression as initial therapy for posttransplantation lymphoproliferative disorder. Am J Transplant. 2011;11(2):336-347. doi: 10.1111/j.1600-6143.2010.03387.x
- Zimmermann H, Trappe RU. Therapeutic options in post-transplant lymphoproliferative disorders. Vol. 2, Therapeutic Advances in Hematology. SAGE Publications; 2011. p. 393-407. doi: 10.1177/2040620711412417
- Lister J, Simpson JK, DeMagalhaes-Silverman MM, Rybka WB, Donnenberg AD, Myers DJ, et al. Allogeneic peripheral blood stem cell transplant for myelodysplasia after chemotherapy for post-transplant lymphoma in a cardiac transplant recipient at 10 years. Bone Marrow Transplant. 1997;19(9):943-945. doi: 10.1038/sj.bmt.1700758
- Kim M.J, Kim I, Bae HM, Seo K, Park N, Yoon SS, et al. Hematopoietic stem cell transplantation after posttransplant lymphoproliferative disorder. J Korean Med Sci. 2010;25(5):781-784. doi: 10.3346/jkms.2010.25.5.781
- Schechter-Finkelstein T, Gassas A, Weitzman S, Grant D, Pollock-Barziv S, Dipchand A, et al. Hematopoietic stem-cell transplantation following solid-organ transplantation in children. Bone Marrow Transplant. 2011;46(10):1321-1325. doi: 10.1038/bmt.2011.153
- Gabeeva NG, Zvonkov EE, Koroleva DA, Chukavina MM, Obukhova TN, Kovrigina AM et al. Successful experience of treatment of a patient with generalized non-GCB-DLBCL using the R-mNHL-BFM-90 protocol with lenalidomide: Case report and review of literature. Ter Arkh. 2018;90(7): 96-101. (In Russian). doi: 10.26442/terarkh201890796-101
- Nowakowski GS, LaPlant B, Macon WR, Reeder CB, Foran JM, Nelson GD, et al. Lenalidomide combined with R-CHOP overcomes negative prognostic impact of non-germinal center B-cell phenotype in newly diagnosed diffuse large B-cell lymphoma: A phase II study. J Clin Oncol. 2015;33(3):251-257. doi: 10.1200/JCO.2014.55.5714
" ["~DETAIL_TEXT"]=> string(31798) "
Introduction
The development of solid organ transplantation and the subsequent lifelong immunosuppressive therapy (IST) is naturally accompanied by the development of complications associated with a specific spectrum of infections, organ dysfunctions, and also with the occurrence of tumor diseases of various etiology. Increasing the number of patients who underwent transplantation of kidneys, liver, heart, lungs, etc. results in the number of patients with post-transplant malignant neoplasms [1]. The most common of them are neoplastic diseases of the hemopoietic system and, mainly, various malignant lymphoproliferative diseases. Even separate forms of these types of tumors which is associated with previous long-term immunosuppression are distinguished in the modern WHO classification [2].
The risk of developing post-transplant lymphoproliferative disease (PTLD) increases by 20-120% in patients after solid organ transplantation compared with the general population and depends on the intensity of IST. PTLD was first described in 1968 by Doak P. B. in two patients after cadaveric kidney transplantation and IST with azathioprine and prednisolone [3]. The term PTLD was introduced by T. E. Starzl in 1984 [4]. The role of the Epstein-Barr virus (EBV) in the pathogenesis of PTLD was described in 1981 [5]. The developing of this disease most frequently associated with solid organ transplantation like heart, lung, intestine and multi-organ transplantation, while this complication develops less frequently in kidney and liver recipients [6, 7]. There was no increase in the incidence of PTLD when cyclosporine was used in comparison with therapy with azathioprine in combination with glucocorticosteroids. Tacrolimus also increases the risk of this complication [7]. Immunosuppressive therapy with antithymocyte globulin (ATG) increases the risk of PTLD within the first year after solid organ transplantation, and no such dependence was found when antibodies to the IL-2 receptor were used [7]. It has been established that in the pathogenesis of PTLD, the presence of certain human leukocyte antigens (HLA) in a patient is important. If alleles HLA-A26 and HLA-B38 are detected in a recipient, the risk of PTLD development increases, while donor haplotypes HLA-A1, HLA-B8, and HLA-DR3 were identified as factors in which this complication develops less frequently [8]. Other studies have identified an increased risk of PTLD in a recipient with HLA-A2, HLA-A11, HLA-B5, HLA-B18, HLA-B21, and HLA-B35 [9, 10].
The clinical manifestations of PTLD are often nonspecific. Involvement of the gastrointestinal (GI) tract, lungs, skin, bone marrow, and central nervous system (CNS) is common [11-15]. CNS involvement is present in about 10-15% of all PTLD cases [11]. B-symptoms such as pyrexia, sweating and weight loss are also common. Damage to the transplanted organ is noted in about a third of all PTLD cases [13]. According to the WHO classification 2017, there are the following types of PTLD: early lesions (plasmacytic hyperplasia, infectious mononucleosis, and florid follicular hyperplasia) – 5% of all PTLD, polymorphic PTLD – 15-20%, monomorphic B-cell neoplasm (diffuse large B-cell lymphoma, Burkitt lymphoma, plasma cell myeloma and other) – more than 70% of all PTLD, monomorphic T/NK-cell neoplasms PTLD (peripheral T-cell lymphoma and other) – less than 5%, and classic Hodgkin lymphoma PTLD – less than 5% [2].
The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. Due to the clinical and pathological heterogeneity of PTLD (type of transplant, risk of rejection and concomitant diseases, tumor burden, etc.), there is no standardized approach to treatment. Nevertheless, the key approach is the reduction of IST: complete cancellation or partial (by 50-75%) reduction the dose of immunosuppressive drugs to prevent rejection of the transplanted organ. In this case, the response is achieved in about half of the patients, but long-term remissions are rare [12, 14-16]. Other methods that can be used in the treatment of PTLD are monoclonal antibodies to the CD20 antigen (rituximab) as monotherapy or in combination with chemotherapy, surgery, and radiation therapy. In the event that the development of PTLD is associated with EBV infection, antiviral therapy (intravenous immunoglobulins) and/or EBV-specific T-lymphocytes are used, autologous or allogeneic hematopoietic stem cells transplantation are used less often as a consolidating treatment [11, 13, 14, 16.17]. Overall survival of patients after PTLD therapy has significantly improved in recent years, by the using of monoclonal antibodies. Mortality rate earlier was reached 50-70%, nowadays the 3-year overall survival rate is 60-70%, according published studies in recent years [7, 13, 14].
The role of allogeneic hematopoietic stem cells (allo-HSCT) transplantation in PTLD therapy after solid organ transplantation has not been determined. The use of high-dose chemotherapy can be accompanied by high toxicity for the transplanted organ. Graft-versus-host disease (GVHD), which develops after allo-HSCT, can contribute to the rejection of a transplanted solid organ. And the presence of a solid organ transplant before allo-HSCT may increase the probability of rejection of hematopoietic stem cells. Only a few successful clinical cases of allo-HSCT in PTLD after solid organ transplantation have been described [1, 18-20].
The aim of this work: to present a clinical case of a patient in whom transplantation of an allogeneic cadaveric kidney was complicated by the development of PTLD, which was initially successfully treated, but due to the ongoing IST, a relapse was established, which required HSCT from a haploidentical donor. Clinical case is presented with the consent of the patient.
Clinical case description
Patient B., female, the disease manifested at the age of 9 years, in 1996 with proteinuria (3 g/day) and increased arterial pressure up to 160/90 mm Hg. Acute glomerulonephritis was diagnosed, and prednisolone therapy was started. In 1998, the diagnosis of mesangioproliferative glomerulonephritis was confirmed by histological examination of a kidney biopsy. Progression to the terminal stage of chronic renal failure (stage 5) was documented in 2003, hemodialysis was started, with arteriovenous fistula arranged. Transplantation of allogeneic cadaveric kidney was performed at the N. V. Sklifosovsky Research Institute for Emergency Medicine in April 2011. Delayed recovery of renal transplant function was noted; hemodialysis was carried out within a month after the organ transplantation. Tacrolimus, mycophenolate mofetil, methylprednisolone were applied as immunosuppressive therapy. Blood creatinine level in the post-transplant period was 110-130 μmol/L, glomerular filtration rate (GFR), according to the CKD-EPI formula, was 48-61 ml/min/1.73 m2. Due to the pregnancy planning, mycophenolate mofetil was replaced by azathioprine in 2016. Pancytopenia was detected in June 2017, but the dose of immunosuppressive drugs was not reduced. Since the end of July 2017, the patient had febrile body temperature, decreasing body weight, dry cough, increased abdominal volume, and irregularity in the menstrual cycle, but the patient did not seek medical asssistance.
In August 2017 the examination revealed proteinuria 2.3 g/l, hypoalbuminemia 28 g/l, high level of blood creatinine (214 μmol/l) and C-reactive protein (115 mg/dl), an increased LDH activity to 923 U/l, ESR up to 70 mm/h, an increased IgM content in the blood (1288 mg/dl), mainly, due to IgMλ. Pancytopenia still persisted (leukocytes 1.9×109/l, platelets 90×109/l). Antibiotic therapy was carried out for suspected infection, azathioprine was canceled. Hepatosplenomegaly was revealed on the CT examination of abdominal organs. Given these findings, lymphoproliferative disease was suggested, thus requiring special examination.
The patient was examined at National Research Center for Hematology at 23.08.2017. Infiltrative-ulcerative defects of the gastric mucosa were found during esophagogastroduodenoscopy. The data of histological and immunohistochemical studies of gastric biopsy revealed the substrate of extranodal diffuse large B-cell lymphoma (tumor cells monomorphically expressed CD 20). In addition, the data of histological and immunohistochemical studies of the bone marrow also was determined: interstitial-small-focal B-cell infiltration with the presence of clusters of large CD 20+ cells, intravascular foci of small CD 20+ B-cells. The expression of EBER (EBV-encoded RNA) was not detected, but the virus replication was detected in blood. Paraprotein M lambda, 21.3 g/l; Bens-Jones protein lambda 0.35 g/l was revealed in blood serum by immunochemistry. Hyperpdiloid karyotype and complex cytogenetic rearrangements involving chromosomes 3, 7, 4, 9, 10, 14, 15, 17, 18 were registered by standard cytogenetic study of the bone marrow samples. According to CT scan, hepatosplenomegaly was determined: the vertical size of the liver was 23.5 cm, the size of the spleen was 160×60×235 mm. Based on the obtained data, the diagnosis of PTLD was specified as a diffuse large B-cell lymphoma (PTLD-DLBCL) associated with immunosuppressive therapy, with involvement of liver, spleen, stomach and bone marrow.
Despite the presence of a transplanted organ, taking into the variant of the disease and the generally accepted practice of managing such patients, the IST was reduced: methylprednisolone and tacrolimus were completely canceled since 24.08.2017.
From 26.08.2017 to 30.08.2017, a pre-phase with dexamethasone and cyclophosphamide was carried out and a positive trend was noted as decreasing size of the liver and spleen. From 31.08.2017 to 05.09.2017, the 1st course of CHOD protocol in combination with rituximab (600 mg) was administered (total drug doses: cyclophosphamide 1200 mg, doxorubicin 75 mg, vincristine 2 mg, dexamethasone 80 mg). The treatment was complicated by febrile fever, oropharyngeal candidiasis, bilateral pleuropneumonia; the patient underwent massive antimicrobial therapy: imipenem/cilastatin, sodium colistimethate, fluconazole, acyclovir and intravenous immunoglobulin. In addition, the patient developed hypotension (up to 80/50 mm Hg). Subsequent examination revealed adrenal insufficiency, which required administration of hydrocortisone (2.5-5 mg per day). A partial remission of the disease was obtained after first R-CHOD. From 26.09.2017 to 11.01.2018, five R-CHOD courses were performed. A complete remission of PTLD-DLBCL was achieved after second course of R-CHOD as confirmed by PET-CT (Fig. 1).

Figure 1. CT dynamics of internal organs. A, in the debut of PTLD-DLBCL (August 2017); B, first remission of PTLD-DLBCL (January 2018); C, relapse of PTLD-DLBCL (January 2019); D, before haplo-HSCT (May 2019)
Due to the risk of renal transplant rejection, the patient resumed immunosuppressive therapy with tacrolimus (2 mg/day) and prednisolone (5 mg/day) after completing chemotherapy (6 courses), since April 2018. In December 2018, 10 months after the completion of therapy for PTLD-DLBCL, the patient had a febrile episode of up to 40°C. Ultrasound examination revealed a focal lesion in the liver. At that moment, no other signs of PTLD progression (based on bone marrow and gastric biopsies) were present. However, a month later, in January 2019, the febrile fever was again observed. The patient was admitted to the hospital in an extremely severe condition with signs of septic shock, bilateral pneumonia with respiratory failure, and evolving acute renal injury (blood creatinine levels reached 522 μmol/l). At the intensive care unit, the patient underwent massive antimicrobial therapy (meropenem, linezolid, sodium colistimethate, fluconazole, acyclovir), and hemodiafiltration were performed, with immunosuppressive therapy still continued. Additional examination revealed an increasing size of the liver (vertical size 24 cm) and spleen (121×54×175 mm) (Fig. 1). B-cell clonality was revealed in the gastric tissue biopsy, infiltration with tumor CD20+ cells was noted in the bone marrow biopsy, monoclonal secretion of M lambda in serum was determined in blood (5.3 g/l), a trace amount of the Bence-Jones protein lambda was detected in the urine, standard cytogenetic study of bone marrow and gastric tissue biopsies no mitosis was detected. Thus, after 11 months of achievement of PET-CT-negative remission and 9 months after the resumption of the IST, a relapse of PTLD-DLBCL was documented.
The severity of the patient's condition was due to both septic condition and emerging relapse of the disease, including specific liver damage. As a result, severe coagulation disorders developed, with re-appearing signs of adrenal insufficiency (decreased concentration of cortisol in blood serum: 90.47 nmol/L (reference range of 185-624 nmol/L), which required administration of hydrocortisone (2.5-5 mg per day), blood transfusions and management of blood clotting problems.
Due to PTLD-DLBCL relapse and severe infectious complications, despite presence of a transplanted organ, the IST was canceled 01.05.2019, and the antitumor effect was not achieved again. The patient's condition remained extremely serious, and according to vital indications, from 01.11.2019 to 15.01.2019 the pre-phase therapy with cyclophosphamide and dexamethasone was started. Positive clinical dynamics was noted, i.e., normalization of body temperature and decrease in the liver and spleen size few days after pre-phase therapy.
Thereafter, a modified course of chemotherapy with cytarabine (=4 g) + etoposide (∑ = 400 mg) combined with lenalidomide (∑ = 30 mg) was carried out from 16.01.2019 to 17.01.2019. Lenalidomide was included in the treatment, according to the previously published data on improvement of overall and progression-free survival when using it in the patients with DLBCL [21, 22]. At the control examination (08.02.2019) we have revealed a decreased size of the liver (vertical size 18 cm) and spleen (115×47×130 mm), complete regression of focal liver lesion, regression of hystological changes in the bone marrow biopsy, and only trace secretion of paraprotein IgM.
Two more courses using cytarabine + etoposide + lenalidomide were performed from 15.02.2019 to 06.05.2019. The second PET-CT-negative remission of PTLD-DLBCL was achieved (Fig. 1).
Thus, the young patient re-achieved PET-СТ negative remission of PTLD-DLBCL, and still required resumption of IST to prevent kidney transplant rejection, which would entail another relapse of the disease. Program therapy for patients in the second remission of the DLBCL implies to consolidate remission by autologous hematopoietic stem cell transplantation. However, our patient would have to return again immunosuppressive therapy to prevent kidney transplant rejection. Therefore, we decided to perform allo-HSCT to induce tolerance of the donor-derived immune cells to the transplanted kidney. The patient didn’t have a fully matched related or unrelated donor, since the HSCT was planned from a related haploidentical (haplo-HSCT) donor (mother), however, with TCRαβ +/CD19+ depletion of the graft. The choice of such a transplant approach was determined by the fact that it does not use long-term (minimum 6 months) immunosuppressive therapy. The last injection of IST drugs (tocilizumab and abatacept) was administered on day +30 after haplo-HSCT with TCRαβ+/CD19+ depletion. Following HLA typing of the patient and her mother was performed, HLA-B18 was identified in the HLA genotype of the patient. This allele is associated with increased incidence of PTLD. The donor was diagnosed with microcytic hypochromic anemia (Hb 101 g/L), she was observed for a long time at a hematologist with a diagnosis of iron deficiency anemia and was treated with iron preparations.
Pre-transplant conditioning regimen included: treosulfan (∑ = 45 g) + melphalan (∑ = 100 mg) + fludarabine (∑ = 225 mg). Haplo-HSCT was performed 14.05.2019 the number of CD34 + cells in the graft was 10.8×106/kg, the number of TCRαβ + lymphocytes was 271.5×103/kg. GVHD prophylaxis consisted of rituximab (∑ = 170 mg) + bortezomib (∑ = 4.2 mg) + tocilizumab (∑ = 460 g) + abatacept (∑ = 1740 mg), the patient did not receive any other immunosuppressive therapy. The early post-transplant period was complicated by febrile fever, mucositis, and neutropenic enterocolitis, positive effect was obtained on carbapenem therapy. The recovery of leukocytes was on day +13 after haplo-HSCT (3.0×109/l).
The patient was discharged from the hospital on day + 21 after haplo-HSCT. There were no problems with the functioning of the renal graft, during conditioning regimen and in the early post-transplant period too.
Early control examinations after haplo-HSCT (+1, +2 months) has shown bone marrow remission of the disease with normal function of erythropoiesis and 100% donor chimerism. However, despite the absence of ABO incompatibility between the patient and the donor (the patient and the donor have the same blood group: 0 (I) Rh + CcDee with differences in the MN system), 95% of erythrocytes had patient’s phenotype. Meanwhile, severe anemia persisted for 6 months after haplo-HSCT, requiring monthly blood transfusions. Therefore, additional tests were performed to search for possible causes of anemia (Table 1). Initially, there were signs of either iron deficient anemia, or anemia of chronic disease (25.06.2019). Parvovirus B19-associated anemia was excluded. However, in September 2019, the signs of microcytic hypochromic anemia worsened, there were a decrease in TIBC, LIBC and transferrin, along with increased ferritin level and normal serum iron content. Mild iron overload was determined by MRI. The clinical diagnosis was considered as follows: anemia of chronic conditions in a patient with transplanted kidney and multiple complications associated with therapy of the disease.
Table 1. Post-transplant monitoring of anemia
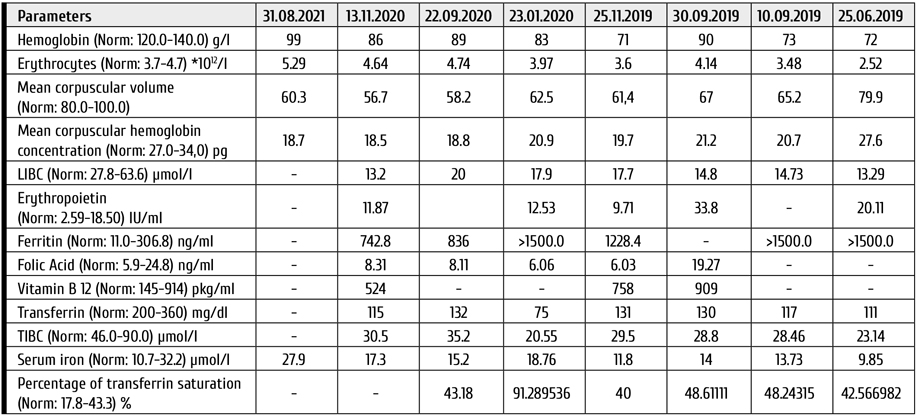

Figure 2. A: Slight increase in the light and heavy fractions of erythrocytes (abscissa, relative cell density, g/cm3). The average density of red blood cells is within normal limits. (B, C): Osmotic fragility (OFT) is altered before and after incubation (abscissa, % of NaCl in saline for RBC incubation)
Given the fact that before haplo-HSCT patient didn’t have any signs of microcytic hypochromic anemia, we have performed hemoglobin electrophoresis, density distribution of erythrocytes, and the osmotic fragility test (OFT) (Fig. 2). The content of the fraction of normal hemoglobin A was 95.9% and hemoglobin A2 was 4.1%.
According to these studies, clinical thalassemia was suspected, and during DNA diagnostic test was found heterozygous carriage of beta (+) – thalassemic mutation IVS1 + 5 G> T. A genetic study of an archived sample of the patient's bone marrow before haplo-HSCT was carried out: thalassemic mutation was not detectable. Thus, the patient was diagnosed with a heterozygous form of beta-thalassemia, which was a consequence of the reconstitution of donor hematopoiesis.
The examination of the haploidentical related donor, the mother, was carried out, and again, as before donation, moderate microcytic hypochromic anemia was revealed. A genetic study was performed, and it was confirmed that the mother is also a heterozygous carrier of the beta (+) – thalassemic mutation IVS1 + 5 G> T.
At the present time, 2.5 years have passed after haplo-HSCT, and 10.5 years after transplantation of allogeneic cadaveric kidney. In this case, the patient had a short course of immunosuppressive drugs (rituximab, bortezomib, tocilizumab, abatacept) only at the early post-transplant period, ceasing the IST at later terms. Immunological tolerance has been achieved: the patient has no signs of GVHD, and the kidney transplant is functioning normally. The patient has PET-CT-negative remission of PTLD-DLBCL. Despite the fact that the patient is a heterozygous carrier of the beta-thalassemia mutation, her primary disease was complicated by the anemia of chronic conditions, which required hemotransfusions for a year after haplo-HSCT. Currently, the patient is transfusion-independent.
Conclusion
Post-transplant lymphoproliferative disease is not such a rare complication after solid organ transplantation, since the immunosuppressive therapy performed increases the risks of developing lymphoid tumors.
We have described for the first time a case of haploidentical HSCT with TCRαβ+/CD19+ graft depletion in a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a transplant of allogeneic cadaveric kidney. In the literature, there are only a few descriptions of allo-HSCT from related or unrelated donors in PTLD after solid organ transplantation, and haploidentical HSCT with TCRαβ+/CD19+ graft depletion has not been previously described. This transplant mode was chosen due to absence of HLA-identical donors, second remission of PTLD-DLBCL, and the fact that the previous relapse was associated with resumption of immunosuppressive therapy (IST) for the transplanted kidney. Haploidentical HSCT with TCRαβ+/CD19+ depletion was performed, since the duration of immunosuppressive therapy is only one month after such procedure. The therapy we have chosen in relapsed PTLD-DLBCL allowed us to achieve a second complete PET-CT-negative remission, then was consolidation with haplo-HSCT, which led to development of immunological tolerance of the donor immune system to the previously transplanted cadaveric kidney and withdrawal of IST, which seemed to be the key factor of PTLD. Both kidney transplant and a bone marrow graft show adequate functioning without additional IST.
Another feature of this patient is that the donor for HSCT is a heterozygous carrier of beta-thalassemia mutation IVS1 + 5 G> T, which was not detected during the initial examination, manifesting with serum iron deficiency. There is no doubt that initial detection of beta-thalassemia trait in the donor could influence the donor choice, since the presence of this mutation and the transplanted kidney during the first year complicated the patient's quality of life after haplo-HSCT.
Conflict of interest
None reported.
References
- Doney KC, Mielcarek M, Stewart FM, Frederick R. Hematopoietic cell transplantation after solid organ transplantation. Biol Blood Marrow Transplant. 2015;21(12):2123-2128. doi: 10.1016/j.bbmt.2015.08.004
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J. WHO Classification of tumours of haematopoietic and lymphoid tissues – IARC [Internet]. Revised 4th edition. Lyon: IARC Press. Lyon: IARC Press; 2017.
- Doak PB, Montgomerie JZ, North JDK, Smith F. Reticulum cell sarcoma after renal homotransplantation and azathioprine and prednisone therapy. Br Med J. 1968; 4(5633): 746-748. doi: 10.1136/bmj.4.5633.746
- Starzl TE, Porter KA, Iwatsuki S, Rosenthal JT, Shaw BW, Atchison RW, et al. Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin-steroid therapy. Lancet. 1984; 323 (8377):583-587. doi: 10.1016/S0140-6736(84)90994-2
- Klein G, Purtilo D. Summary: symposium on Epstein-Barr virus-induced lymphoproliferative diseases in immunodeficient patients. Cancer Res. 1981; 41(11 Pt 1): 4302-4304.
- Cockfield SM. Identifying the patient at risk for post-transplant lymphoproliferative disorder. Transplant Infect Dis. 2001; 3: 70-78. doi: 10.1034/j.1399-3062.2001.003002070.x
- Opelz G, Döhler B. Lymphomas after solid organ transplantation: a collaborative transplant study report. Am J Transplant. 2004; 4(2): 222-230. doi: 10.1046/j.1600-6143.2003.00325.x
- Reshef R, Luskin MR, Kamoun M, Heitjan DF, Hadjiliadis D, Goral S, et al. Association of HLA polymorphisms with post-transplant lymphoproliferative disorder in solid-organ transplant recipients. Am J Transplant. 2011;11(4):817-825. doi: 10.1111/j.1600-6143.2011.03454.x
- Pourfarziani V, Einollahi B, Taheri S, Nemati E, Nafar M, Kalantar E, et al. Associations of Human Leukocyte Antigen (HLA) haplotypes with risk of developing lymphoproliferative disorders after renal transplantation. Ann Transplant. 2007;12(4):16-22. PMID: 18344933
- Subklewe M, Marquis R, Choquet S, Leblond V, Garnier JL, Hetzer R, et al. Association of human leukocyte antigen haplotypes with posttransplant lymphoproliferative disease after solid organ transplantation. Transplantation. 2006;82(8):1093-1100.
doi: 10.1097/01.tp.0000235889.05171.12 - Al-Mansour Z, Nelson BP, Evens A.M. Post-transplant lymphoproliferative disease (PTLD): Risk factors, diagnosis, and current treatment strategies. Curr Hematol Malig Rep. 2013; 8(3):173-183. doi: 10.1007/s11899-013-0162-5
- Jagadeesh D, Woda BA, Draper J, Evens A.M. Posttransplant lymphoproliferative disorders: Risk, classification, and therapeutic recommendations. Curr Treat Options Oncol. 2012;13(1):122-136. doi: 10.1007/s11864-011-0177-x
- Ghobrial IM, Habermann TM, Maurer MJ, Geyer SM, Ristow KM, Larson TS et al. Prognostic analysis for survival in adult solid organ transplant recipients with post-transplantation lymphoproliferative disorders. J Clin Oncol. 2005;23(30):7574-7582. doi: 10.1200/JCO.2005.01.0934
- Evens AM, David KA, Helenowski I, Nelson BK, Dixon K, Sheetal M, et al. Multicenter analysis of 80 solid organ transplantation recipients with post-transplantation lymphoproliferative disease: Outcomes and prognostic factors in the modern era. J Clin Oncol. 2010;28(6):1038-1046. doi: 10.1200/JCO.2009.25.4961
- Gavrilina OA, Troitskaya VV, Zvonkov EE, Parovichnikova EN, Galstyan GM, Biryukova LS, et al. EBV-positive central nervous system lymphoproliferative disease associated with immunosuppression after organ transplantation: Long-term remission without chemotherapy. Ter Arkh. 2017;89(7):69-75. (In Russian). doi: 10.17116/terarkh201789769-75
- Reshef R, Vardhanabhuti S, Luskin MR, Heitjan DF, Hadjiliadis D, Goral S, et al. Reduction of immunosuppression as initial therapy for posttransplantation lymphoproliferative disorder. Am J Transplant. 2011;11(2):336-347. doi: 10.1111/j.1600-6143.2010.03387.x
- Zimmermann H, Trappe RU. Therapeutic options in post-transplant lymphoproliferative disorders. Vol. 2, Therapeutic Advances in Hematology. SAGE Publications; 2011. p. 393-407. doi: 10.1177/2040620711412417
- Lister J, Simpson JK, DeMagalhaes-Silverman MM, Rybka WB, Donnenberg AD, Myers DJ, et al. Allogeneic peripheral blood stem cell transplant for myelodysplasia after chemotherapy for post-transplant lymphoma in a cardiac transplant recipient at 10 years. Bone Marrow Transplant. 1997;19(9):943-945. doi: 10.1038/sj.bmt.1700758
- Kim M.J, Kim I, Bae HM, Seo K, Park N, Yoon SS, et al. Hematopoietic stem cell transplantation after posttransplant lymphoproliferative disorder. J Korean Med Sci. 2010;25(5):781-784. doi: 10.3346/jkms.2010.25.5.781
- Schechter-Finkelstein T, Gassas A, Weitzman S, Grant D, Pollock-Barziv S, Dipchand A, et al. Hematopoietic stem-cell transplantation following solid-organ transplantation in children. Bone Marrow Transplant. 2011;46(10):1321-1325. doi: 10.1038/bmt.2011.153
- Gabeeva NG, Zvonkov EE, Koroleva DA, Chukavina MM, Obukhova TN, Kovrigina AM et al. Successful experience of treatment of a patient with generalized non-GCB-DLBCL using the R-mNHL-BFM-90 protocol with lenalidomide: Case report and review of literature. Ter Arkh. 2018;90(7): 96-101. (In Russian). doi: 10.26442/terarkh201890796-101
- Nowakowski GS, LaPlant B, Macon WR, Reeder CB, Foran JM, Nelson GD, et al. Lenalidomide combined with R-CHOP overcomes negative prognostic impact of non-germinal center B-cell phenotype in newly diagnosed diffuse large B-cell lymphoma: A phase II study. J Clin Oncol. 2015;33(3):251-257. doi: 10.1200/JCO.2014.55.5714
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "10" ["~SORT"]=> string(2) "10" ["CODE"]=> string(100) "transplantatsiya-allogennykh-gemopoeticheskikh-stvolovykh-kletok-ot-gaploidentichnogo-donora-bolnoy-" ["~CODE"]=> string(100) "transplantatsiya-allogennykh-gemopoeticheskikh-stvolovykh-kletok-ot-gaploidentichnogo-donora-bolnoy-" ["EXTERNAL_ID"]=> string(4) "2055" ["~EXTERNAL_ID"]=> string(4) "2055" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(596) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почкиA case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(2918) "<p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток. </p> <p style="text-align: justify;">Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.</p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_META_TITLE"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_META_KEYWORDS"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_META_DESCRIPTION"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_PICTURE_FILE_ALT"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_PICTURE_FILE_TITLE"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_PICTURE_FILE_NAME"]=> string(100) "transplantatsiya-allogennykh-gemopoeticheskikh-stvolovykh-kletok-ot-gaploidentichnogo-donora-bolnoy-" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(408) "Трансплантация аллогенных гемопоэтических стволовых клеток от гаплоидентичного донора больной диффузной В-клеточной крупноклеточной лимфомой, развившейся на фоне иммуносупрессивной терапии после трансплантации почки" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(100) "transplantatsiya-allogennykh-gemopoeticheskikh-stvolovykh-kletok-ot-gaploidentichnogo-donora-bolnoy-" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(100) "transplantatsiya-allogennykh-gemopoeticheskikh-stvolovykh-kletok-ot-gaploidentichnogo-donora-bolnoy-" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(100) "transplantatsiya-allogennykh-gemopoeticheskikh-stvolovykh-kletok-ot-gaploidentichnogo-donora-bolnoy-" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "208" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28566" ["VALUE"]=> string(22) "01/25/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/25/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28567" ["VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28568" ["VALUE"]=> array(2) { ["TEXT"]=> string(495) "<p>Елена Н. Паровичникова, Вера А. Васильева, Ольга А. Алешина, Мария В. Довыденко, Лариса А. Кузьмина, Михаил Ю. Дроков, Ирина А. Лукьянова, Вера В. Троицкая, Евгений Е. Звонков, Алла М. Ковригина, <span style="border: 1px solid black; margin: 0; padding: 2px 2px;">Валерий Г. Савченко</span></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(461) "
Елена Н. Паровичникова, Вера А. Васильева, Ольга А. Алешина, Мария В. Довыденко, Лариса А. Кузьмина, Михаил Ю. Дроков, Ирина А. Лукьянова, Вера В. Троицкая, Евгений Е. Звонков, Алла М. Ковригина, Валерий Г. Савченко
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28569" ["VALUE"]=> array(2) { ["TEXT"]=> string(163) "<p>Национальный медицинский исследовательский центр гематологии, Москва, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(151) "Национальный медицинский исследовательский центр гематологии, Москва, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_RU"]=> array(36) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28570" ["VALUE"]=> array(2) { ["TEXT"]=> string(2918) "<p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток. </p> <p style="text-align: justify;">Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2840) "Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток.
Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.
Ключевые слова
Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28571" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-50-57" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-50-57" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28572" ["VALUE"]=> array(2) { ["TEXT"]=> string(340) "<p>Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina, Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, <span style="border: 1px solid black; margin: 0; padding: 2px 2px;">Valery G. Savchenko</span> </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(306) "Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina, Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, Valery G. Savchenko
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28573" ["VALUE"]=> array(2) { ["TEXT"]=> string(760) "<p>National Medical Research Center for Hematology, Moscow, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia<br> Phone: +7 (916) 262-23-16<br> E-mail: vasilievaVA4@mail.ru</p> <br> <p><b>Citation:</b> Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(670) "National Medical Research Center for Hematology, Moscow, Russia
Correspondence:
Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia
Phone: +7 (916) 262-23-16
E-mail: vasilievaVA4@mail.ru
Citation: Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28574" ["VALUE"]=> array(2) { ["TEXT"]=> string(1569) "<p style="text-align: justify;">Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells. </p> <p style="text-align: justify;">We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.</p> <h2>Keywords</h2> <p style="text-align: justify;">Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1491) "Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells.
We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.
Keywords
Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28575" ["VALUE"]=> string(188) "A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(188) "A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28576" ["VALUE"]=> string(4) "2807" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2807" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28577" ["VALUE"]=> string(4) "2808" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2808" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(10) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28572" ["VALUE"]=> array(2) { ["TEXT"]=> string(340) "<p>Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina, Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, <span style="border: 1px solid black; margin: 0; padding: 2px 2px;">Valery G. Savchenko</span> </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(306) "Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina, Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, Valery G. Savchenko
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(306) "Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina, Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, Valery G. Savchenko
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28574" ["VALUE"]=> array(2) { ["TEXT"]=> string(1569) "<p style="text-align: justify;">Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells. </p> <p style="text-align: justify;">We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.</p> <h2>Keywords</h2> <p style="text-align: justify;">Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1491) "Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells.
We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.
Keywords
Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(1491) "Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells.
We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.
Keywords
Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28571" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-50-57" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-50-57" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-50-57" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28575" ["VALUE"]=> string(188) "A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(188) "A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(188) "A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28573" ["VALUE"]=> array(2) { ["TEXT"]=> string(760) "<p>National Medical Research Center for Hematology, Moscow, Russia</p><br> <p><b>Correspondence:</b><br> Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia<br> Phone: +7 (916) 262-23-16<br> E-mail: vasilievaVA4@mail.ru</p> <br> <p><b>Citation:</b> Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(670) "National Medical Research Center for Hematology, Moscow, Russia
Correspondence:
Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia
Phone: +7 (916) 262-23-16
E-mail: vasilievaVA4@mail.ru
Citation: Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(670) "National Medical Research Center for Hematology, Moscow, Russia
Correspondence:
Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia
Phone: +7 (916) 262-23-16
E-mail: vasilievaVA4@mail.ru
Citation: Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28568" ["VALUE"]=> array(2) { ["TEXT"]=> string(495) "<p>Елена Н. Паровичникова, Вера А. Васильева, Ольга А. Алешина, Мария В. Довыденко, Лариса А. Кузьмина, Михаил Ю. Дроков, Ирина А. Лукьянова, Вера В. Троицкая, Евгений Е. Звонков, Алла М. Ковригина, <span style="border: 1px solid black; margin: 0; padding: 2px 2px;">Валерий Г. Савченко</span></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(461) "Елена Н. Паровичникова, Вера А. Васильева, Ольга А. Алешина, Мария В. Довыденко, Лариса А. Кузьмина, Михаил Ю. Дроков, Ирина А. Лукьянова, Вера В. Троицкая, Евгений Е. Звонков, Алла М. Ковригина, Валерий Г. Савченко
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(461) "Елена Н. Паровичникова, Вера А. Васильева, Ольга А. Алешина, Мария В. Довыденко, Лариса А. Кузьмина, Михаил Ю. Дроков, Ирина А. Лукьянова, Вера В. Троицкая, Евгений Е. Звонков, Алла М. Ковригина, Валерий Г. Савченко
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28566" ["VALUE"]=> string(22) "01/25/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/25/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "01/25/2022 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28567" ["VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "03/18/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "03/18/2022 12:00:00 am" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28570" ["VALUE"]=> array(2) { ["TEXT"]=> string(2918) "<p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток. </p> <p style="text-align: justify;">Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(2840) "Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток.
Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.
Ключевые слова
Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(2840) "Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток.
Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.
Ключевые слова
Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28569" ["VALUE"]=> array(2) { ["TEXT"]=> string(163) "<p>Национальный медицинский исследовательский центр гематологии, Москва, Россия</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(151) "Национальный медицинский исследовательский центр гематологии, Москва, Россия
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(22) "Организации" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(151) "Национальный медицинский исследовательский центр гематологии, Москва, Россия
" } } } [7]=> array(49) { ["IBLOCK_SECTION_ID"]=> string(3) "209" ["~IBLOCK_SECTION_ID"]=> string(3) "209" ["ID"]=> string(4) "2056" ["~ID"]=> string(4) "2056" ["IBLOCK_ID"]=> string(1) "2" ["~IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["~NAME"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["ACTIVE_FROM"]=> NULL ["~ACTIVE_FROM"]=> NULL ["TIMESTAMP_X"]=> string(22) "04/19/2022 02:09:28 pm" ["~TIMESTAMP_X"]=> string(22) "04/19/2022 02:09:28 pm" ["DETAIL_PAGE_URL"]=> string(159) "/en/archive/tom-11-nomer-1/eksperimentalnye-issledovaniya/terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen/" ["~DETAIL_PAGE_URL"]=> string(159) "/en/archive/tom-11-nomer-1/eksperimentalnye-issledovaniya/terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen/" ["LIST_PAGE_URL"]=> string(12) "/en/archive/" ["~LIST_PAGE_URL"]=> string(12) "/en/archive/" ["DETAIL_TEXT"]=> string(53759) "Introduction
Although the liver has a considerable inherent regenerative capacity, a sufficient and prolonged may result into liver damage and onset of hepatic fibrosis [1]. For severe hepatic diseases, liver transplantation is one of the more effective treatments [2]. However, the tremendous gap between offered donor organs and those required for transplantation is the major limitation of liver replacement therapy [3]. High cost and transplant rejection following liver transplantation, have also largely limited its clinical application [4]. Therefore, alternative or adjuvant therapies are urgently needed [3].
Recently, regenerative medicine using different stem cells has been considered an attractive therapy for treating patients with severe liver disease [5], since these cells have the ability of self-renewal and maturation [6]. Stem cells are defined as undifferentiated cells from an embryo, fetus or an adult, which have the potential to produce various differentiated tissue cells under appropriate stimuli [5]. Bone marrow (BM) provides a more readily available source of cells [7]. Bone marrow cells are presently considered to be the most promising cell source for the cell therapy of various diseases [8]. Mesenchymal stromal cells (MSCs) have been documented as a promising technique for cell therapy and have been successfully applied in the treatment of various diseases [3]. Multipotent MSCs represent a remarkable stem cell population for application in liver-directed cell transplantation, since they are readily obtained from bone marrow aspirates and can be expanded in culture [9], through as many as 50 population doublings in about 10 weeks [10], thus producing a large number of potent cells [9]. In addition, BM-MSCs possess many advantages such as autologous sources, abundance of cells, an immune-modulatory capacity, secretion of cytokines and growth factors, homing to injury sites, and hepatic differentiation [11].
The present study aimed to investigate the therapeutic effect of bone marrow-derived mesenchymal stromal cells MSC(M) transplantation in alleviation of CCl4-induced liver damage in mice.
Materials and methods
Experimental Animals
Healthy male mice (Balb/c, 4-6 weeks) were used in this study. Mice were housed in clean cages of 65×25×15 cm containing woodchip bedding. Mice were housed in a temperature (temperature 24±2°C) and light-controlled room (12h light/dark cycle), with free access to food and water. The animals were left for two weeks to acclimatize to their surroundings before starting the experiment. All procedures were performed according to the Guide for the Care and Use of Laboratory Animals and the ethical standards of our institution.
Liver damage induction and MSC(M) preparation
To establish the liver-injury mice model, male Balb/c mice were intraperitoneally injected with (1 ml/kg body weight) of CCl4 dissolved in olive oil twice a week for 7 consecutive weeks.
In the current study, 4-6 weeks male healthy BALB/c mice were used as donors of MSC(M). Mice were sacrificed by cervical dislocation. MSC(M) were flushed from the medullary cavities of the tibia and femur using a needle with complete media (Dulbecco’s modified Eagle’s medium (DMEM) (Euroclone, Italy). The cells were grown in (4-5 ml) of DMEM medium supplemented with (20% FBS, 1% L-glutamine, 1% penicillin/streptomycin and 1.5 µg/ml amphotericin B) (Euroclone, Italy), in a 25 cm2 culture flask, and incubated at 37°C with 5% CO2. 24 h later, the culture medium was replaced to remove non-adherent cells and tissue debris. MSC(M) at passage 0 (P0) were used for transplantation.
Experimental Protocol
The mice were divided into the following groups:
• Control group (Group I): This group included healthy normal mice, which were not exposed and did not receive any treatment.
• Experimental group: mice were intraperitoneally injected with CCl4 (1 ml/kg body weight) of dissolved in olive oil twice a week for 7 consecutive weeks. After the last injection of CCl4, three mice were randomly selected from this group, blood samples were collected and serum ALT level was determined to ensure that liver damage had been induced before continuing the experiment. Mice in this group were randomly divided into two groups, as follows:
• PBS-treated group (Group II): mice were intravenously injected into the tail vein with 0.5 ml of phosphate buffer saline (PBS 1X).
• MSC(M) treated group (Group III): mice were intravenously injected with MSC(M). MSC(M) were washed with PBS (1X) and trypsinized with 0.25% trypsin, then (approximately 3×106 of MSC(M) per mouse) were re-suspended in (0.5 ml) of PBS and injected into the tail vein.
The mice from all studied groups (I, II, III) were sacrificed 4 weeks after transplantation. Venous blood and liver tissue samples were collected for further analyses. At the end of the experiment, the body weight and liver weight of the animals in all studied groups were determined. The liver to body weights ratio was determined as follows:
Liver to body Ratio = (liver weight (g)/(mouse body weight (g)-liver weight (g))) *100.
Laboratory analyses
Venous blood was collected, and blood samples were centrifuged at 3000 rpm for 5 minutes. Serum samples were subsequently analyzed to evaluate the activities of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and albumin.
Liver histology was performed to assess liver damage 4 weeks after MSC(M) transplantation. For light microscopic examination, the liver from each animal was carefully dissected and the specimens were fixed in 10% formalin for 48 hours. Paraffin sections were prepared and stained with hematoxylin and eosin (H&E) to display the histological details. Histological damage was evaluated by a pathologist who was blinded to the experimental groups.
At the end of the experiment, blood samples were collected and centrifuged at 3000 rpm for 5 min. The serum levels of interleukin-4 (IL-4) and IFN-γ cytokines were measured by ELISA assay kits according to the manufacturer’s instructions (Sun Red, China).
Results
The cultured MSCs were injected into syngeneic mice treated with hepatotoxic agent CCl4.
The results of this study showed remarkable significant increase in the liver weight and the liver weight to body weight ratio in PBS group compared with the normal control group. MSC(M) transplantation alleviated the increase in the liver weight and even decreased the ratio to a level closer to that of normal mice. There was no significant difference in the ratio between the MSC(M) treated group and the normal control group (Table 1).
Table 1. Body mass, liver weight and liver-to-body weight ratios of all studied groups
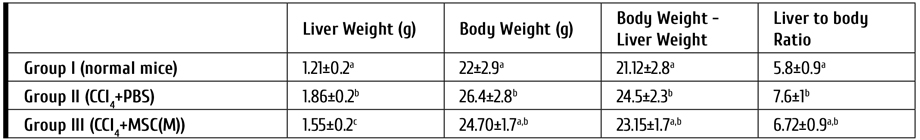
Note: All values are represented as mean ± SD. Mean values with different letters over the same column are significantly different at (P<0.05)
Serum levels of ALT, AST, ALP, and albumin were evaluated. After intraperitoneal injection of CCl4 for consecutive 7 weeks, serum levels of ALT were markedly increased in the experimental group (120±5.3), as compared to control group. PBS group exhibited markedly increased serum levels of ALT and ALP compared with control normal mice. The levels of ALT and ALP in the MSC(M)-treated group were significantly reduced compared to the PBS group being close to the normal control group. In addition, there was a significant decrease in serum levels of albumin in PBS group when compared with the control group. Significantly increased serum albumin levels were noticed in MSC(M)-treated group when compared to the PBS group. The levels of these parameters in control and MSC(M) treated group did not show any significant differences. Nearly similar AST levels were observed in MSC(M) and PBS groups (Table 2).
Table 2. Serum levels of ALT, AST, ALP, and albumin in the studied groups

Note: All values are represented as mean ± SD. Mean values marked with different letters (a,b) over the same column are significantly different at (P<0.05)
Histopathological analysis of liver sections
The liver of the control group was reddish-brown, with smooth and glossy surface. The liver of the PBS group was pale-brown, overtly swollen with coarse surface and necrotic spots. In MSC(M)-treated group, the liver surface was slightly coarse, less swollen, more reddish, and glossy compared with livers from the PBS group. Necrotic spots on the surface were noticeably reduced (Fig. 1).

Figure 1. Morphologic examination of the livers of the study groups. (A). The liver of the normal control group was smooth, lustrous, and reddish. (B) In the PBS group, the liver was pale-brown with coarse surface and overtly swollen. (C) In the mice receiving MSC(M) transplantation, the liver surface was slightly coarse, less swollen, more reddish, and lustrous than those of PBS group
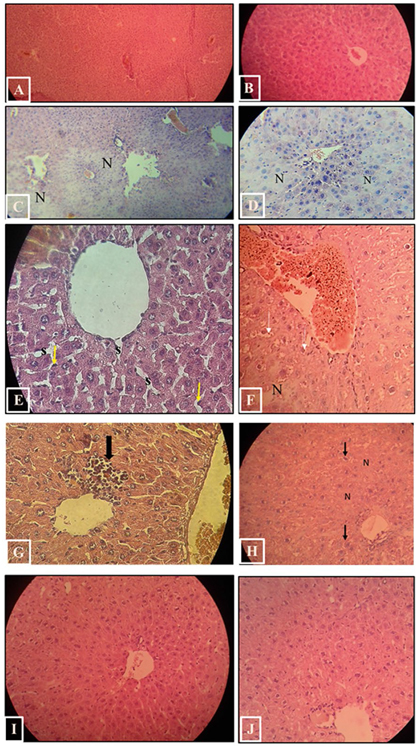
Figure 2. H&E-stained sections in Balb/c mice’s liver of the study groups. A, B. Control group. C–H. PBS group. C-D. Marked damage with disorganization of hepatic architecture, hepatocytes necrosis (N) can be seen. E. The blood sinusoids (s) are dilated and surrounded by Kupffer cells (arrows) with prominent nuclei. F. Vascular dilatation and congestion can be seen, some hepatocytes showed vacuolated cytoplasm (arrows). G. Inflammatory cell infiltration (arrow). H. hepatocytes with vacuolated cytoplasm (arrows). I, J. MSC(M) treated group. nearly normal organization of hepatic lobules. Hepatocytes appeared nearly similar to that of the control mice
Light microscope examination of normal liver tissue sections (control group) showed classical hepatic architecture (Fig. 2. A,B). Hepatocytes are arranged in cords that radiate from the central veins and separated by blood sinusoids. They had rounded nuclei and well-preserved cytoplasm. Some hepatocytes were binucleated. Blood sinusoids are lined by Kupffer cells and endothelial cells. Normal blood vessels and bile ducts were observed in Portal areas. PBS group showed marked affection with disorganization of hepatic architecture. Cellular necrosis was observed. Some hepatocytes appeared swollen with extensively vacuolated cytoplasm. Liver sections also revealed vascular dilatation and congestion in the portal areas and in the central veins. Some parts showed dilated blood sinusoids, which were lined by many Kupffer cells with prominent nuclei. Inflammatory cell infiltration was also detected (Fig. 2. C-H). The histopathological lesions were effectively attenuated to varying extents, in the MSC(M) treated group. Examination of H&E-stained sections showed nearly normal organization of hepatic lobules. A marked reduction of cellular necrosis was observed (Fig. 2, I, J). Hepatocytes appeared nearly similar to that of the control mice. Most hepatocytes had rounded nuclei and well-preserved cytoplasm, they were arranged around slightly dilated and congested central veins and separated by hepatic blood sinusoids. Few hepatocytes appeared with vacuolated cytoplasm. Liver sections demonstrated slight inflammatory cell infiltration. Portal areas appeared nearly normal with slightly congested blood vessels.
Serum Interleukin-4 (IL-4) and Interferon-γ (IFN-γ) Levels
To determine if MSC(M) transplantation affects the cytokine release, the serum levels of IL-4 and IFN-γ were measured by ELISA. As shown in Fig. 3, IL-4 level declined in the PBS group compared to the control group, and this effect was blocked by MSC(M) transfusion. Serum IL-4 level was elevated in MSC(M) treated group, as compared with the PBS group. Serum IFN-γ level was elevated in PBS group compared with the control group. The secretion of IFN-γ was higher in the MSC(M) treated group than in the control group and PBS group, at one month post transplantation.

Figure 3. Serum levels of IL-4, and IFN-γ cytokines. Sera were collected one month after MSC(M) transplantation, and cytokines were measured with enzyme-linked immunosorbent assay (ELISA). After MSC(M) transplantation, the IL-4, and IFN-γ levels were increased compared to PBS group
Discussion
Liver disease causes approximately two million deaths annually worldwide [12]. Therefore, there is an urgent need to develop new techniques to stimulate liver regeneration. In this regard, the potential of MSC therapy is of great interest in regard of liver regeneration [13]. Cell transplantation programs may provide a hopeful technology to replace organ transplantation [3].
Since CCl4 is toxic and may cause death, establishment of liver damage model in mouse is challenging [14]. When metabolized in liver by the cytochrome P450 monooxygenases, CCl4 produces free oxygen species [15, 16]. CCl4 activation to trichloromethyl and trichloromethyl peroxy radicals is stimulates lipid peroxidation and protein oxidation in the liver, causing membrane damage and liver injury [17].
Bone marrow mesenchymal stromal cells were isolated, cultured, and characterized in our previous study (data not shown). Although the isolated cells showed the characteristics of mesenchymal stromal cells, we guess that the population also contained a low proportion of hematopoietic stem cells, since we used the cells at the zero passage (P0), since hematopoietic stem cells have been reported to exist in MSC cultures even after nine in vitro passages [18].
In the current study, MSC(M) at passage 0 were used for transplantation, thus being different from the earlier experiments with MSC(M) therapy published so far, where MSC(M) were mostly injected at passage 3 (P3 MSC(M)).
The in vitro expansion is always required for MSC-based therapies in order to generate sufficient MSC(M) numbers for transplantation. Clinical recommendations for medical MSC usage usually apply cells from 3-5 passages. However, unexpected risks may occur during cell growth, including lack of phenotype, contamination and reduction in efficacy, possibly leading to therapy failure. It has also been reported that additional expansion might attenuate the stemness property of MSCs, thus contributing to reduction of therapeutic potential [19].
Previous report demonstrated that human MSCs subjected to extensive passaging may undergo morphological, phenotypic, and genetic changes [20]. It has been shown that the monolayer cultures significantly affect cell behavior, e.g., leading to cell senescence and impairment of multi-potency [19].
We have also studied the effects of MSC(M) transplantation upon body weight and liver weight. CCl4 is known to be a potent toxicant associated with the liver damage [21]. Determination of the liver weight to body weight ratio of mice may reflect structural and functional changes of the liver after CCl4 injury [22]. Since the body mass measures include the liver weight, it was subtracted from body weight to obtain a "liver-free" estimate of the body weight. Subtraction the liver weight is necessary because otherwise the measurable body weight will always reflect changes in the liver weight. It may make little difference in practice, because the liver weight is small, as compared with total body weight [23]. Significant increase in the liver weight was observed in PBS group compared with control group. This elevation in liver weight after CCl4 intoxication has been well supported by previous research [21, 24]. However, MSC(M) treatment seems to significantly reduce liver inflammation and hence, the liver weight. The ratio of liver weight to body mass was higher in PBS group with significant difference compared to the normal control group. MSC(M) treatment caused a non-significant decrease in this ratio compared to the PBS-treated group, but it became closer to the values of normal control group.
Estimation of biochemical indexes is widely accepted as a biomarker of liver damage [25]. Enzymes represent sensitive metabolic markers, thus even slight changes in enzyme activities would affect the organism [26]. Serum ALT level is usually elevated in case of serious liver damage and the extent of organ damage depends on the type of toxin, its mechanism of action and duration of exposure [26]. Serum ALT activity is a reliable and sensitive marker of liver disease [27].
The present study revealed a marked increase in the level of ALT upon exposure to CCl4 for 7 weeks (experimental group), which indicates considerable hepatocellular injury [28].
Exposure to CCl4 leads to liver injury [15]. Oxidative stress is considered to be the major pathogenic process of CCl4-induced liver injury [29]. This process causes changes in the of cell membrane permeability [15]. As a result, cytoplasmic ALT can leak into the bloodstream, and serum ALT level is increased [29], and can be determined [30]. In this study, we did not use liver toxin after transplantation of MSC(M). During treatment, it is important to eliminate the pathogen, in order to treat the disease efficiently without causing unnecessary complications. Such a strategy has the advantage of enhancing the recipient’s therapy regimen [31].
The results showed a decrease in ALT level in the PBS group compared to experimental group, which is explained by self-recovery and regeneration of mouse livers after CCl4 injection was discontinued. However, alleviation of liver damage occurred significantly faster in mice treated with MSC(M) than in untreated mice. MSC(M)-treated mice showed statistically significant improvement when compared to the PBS-treated group. These results reflect the important role of MSC(M) and show that MSC(M) transplantation can enhance regenerative capacity of the liver and improve affected tissues.
Alkaline phosphatase activity is a very useful serum biochemical marker of liver disease [32]. The present study revealed a significant increase in ALP level of PBS-treated group compared with MSC(M)-treated group. Liver ALP is synthesized by the bile duct. Previously, ALP was thought to be increased, due to inability of liver cells to release the enzyme with bile. It is, however, accepted that ALP activity is increased due to higher enzyme synthesis [33], with involvement of biliary ways [34]. The increased hepatic enzyme activity clearly parallels the rise in serum alkaline phosphatase activity, which is primarily caused by increased ALP mRNA translation (mediated by elevated bile acid concentration), and increased secretion of ALP into serum via canalicular leakage into the hepatic sinusoids by still unclear mechanisms [35].
Albumin synthesis is highly sensitive to CCl4 effects [36]. Albumin and other hepatic secretory proteins are synthesized by polysomes bound to the endoplasmic reticulum. CCl4 causes damage to hepatocytes, including disruption of hepatic cells with polysome disaggregation and decrease in protein synthesis [37].
On the other hand, it was thought that CCl4 toxicity leads to damage of Golgi apparatus, which, in turn, negatively affects protein packaging and release from hepatocytes [36]. One month after MSC(M) transplantation, liver injury markers (ALT and ALP) showed positive changes compared with PBS group. A significant increase in serum albumin level was noticed in MSC(M)-treated group compared to the PBS group, which suggests that transplantation of MSC(M) results in significant restoration of specific liver function.
The liver histology studies were consistent with biochemical results, suggesting an improvement in MSC(M) treated group compared with PBS group. In the current study, CCl4 intoxication resulted in disorganization of hepatic architecture, necrosis of hepatocytes, cytoplasm vacuolation, vascular congestion and dilation, dilatation of sinusoids and infiltration with inflammatory cell, as revealed by light microscope examination of livers from PBS group. Carbon tetrachloride is metabolized by cytochrome to reactive oxygen species, resulting in membrane lipid peroxidation and oxidative stress injury, and, finally, hepatocyte necrosis and dysfunction [38]. Necrosis is viewed as a largely unregulated sequence of physicochemical stress, characterized by mitochondrial impairment, adenosine triphosphate (ATP) depletion, and subsequent failure of ATP-dependent ion pumps. These changes result in rapid swelling of cells and cell organelles ("oncosis") accompanied by the formation of membrane "blebs" and eventual cell rupture [39].
Microscopical examination of liver sections in PBS group showed vascular dilatation and congestion. Dilatation may be caused by increase levels of prostaglandin synthesis that leads to smooth muscle relaxation and vasodilatation [40]. The congestion may be due to fluid loss from the dilated vessels, so they become filled with red blood cells [40]. This congestion, as suggested by Hong et al., (1991) and Wijetunga et al., (2003), is a typical early index of hepatotoxicity [17]. The liver sections of PBS group exhibited cytoplasmic vacuolation and increase in cell volume which are due to the loss of the cell's regulating mechanism for pumping out water from the inside. Cell swelling in CCl4 intoxication is due to altered cell membrane permeability. CCl4 is a non-polar lipophilic substance, thus leading to changes in the physical and chemical properties of both cytoplasmic and mitochondrial lipid membranes, and resulting in disruption of Na+/K+ pump and migration of interstitial fluids to the hepatocytes [40].
After MSC(M) transplantation, marked reduction in liver damage was observed, as compared to PBS group, thus suggesting heterogeneous response to cell therapy in distinct animals. Microscopic examination showed improvement in the histopathological changes induced by CCl4, and in hepatic lobular architecture. Previous study has shown that MSCs secrete several factors, i.e., nitric oxide and prostaglandin E2, which enhance antioxidant protection, inhibit oxidative factors, and reduce the hepatocyte necrosis [11]. However, the mechanism by which MSC(M) repair liver damage remain unclear [41].
The studies of IL4 and IFN-γ serum levels by ELISA have shown some differences in IL-4 between CCl4-treated animals and controls. Cytokines are a class of polypeptide micro-molecules secreted by various cells, which are able to regulate cell growth and differentiation, immune function, inflammation and wound healing [15]. E.g., interferon-γ (IFN-γ) is the hallmark cytokine of T helper 1 (Th1) cells, whereas interleukin 4 (IL-4) has the same role in Th2 cells [42]. The results showed that the serum level of IL-4 decreased in PBS treated mice compared to the control group (intact mice). After MSC(M) transplantation, the IL-4 level increased.
Differences in IL-4 levels between serum of mice treated and those not treated with MSC(M) proved that MSC(M) had a therapeutic effect. IL-4 is one of the widely recognized immune regulatory cytokines capable of suppressing inflammation [43]. It has been used successfully in the treatment of inflammatory diseases in animal models, and in experimental studies, IL-4 injections significantly improved the condition of psoriatic dermatitis [44]. Several studies suggest that treatments that act to increase the concentration of interleukin-4 in tissues may be beneficial in treating inflammation [45, 46].
However, the exact mechanisms by which IL-4 exerts its anti-inflammatory effects are not well understood [44]. The lower levels of the anti-inflammatory cytokine IL-4 found in the injured group compared to control is in accordance with previous studies showing suppression of this cytokine during acute injury [47-49].
Our results are consistent with prior studies that showed that the IL-4 level was higher in the MSC-treated group compared to the untreated mice [43, 49, 50]. It has been demonstrated that MSCs caused the TH2 cells to increase secretion of IL-4 [51, 52]. Chai et al., (2016) have shown that MSC(M) may increase IL-4 secretion in rats with liver fibrosis induced by dimethyl nitrosamine (DMN) both in vitro and in vivo [49]. Jia et al., (2018) indicated that the IL-4 mRNA expression was significantly higher in corneal grafts from MSCs-treated groups when compared with controls (PBS group) [50]. Our data showed that anti-inflammatory cytokine IL-4 exhibited remarkable increase in the MSC(M)-treated group. These findings may explain how MSC(M) mediate the cell repair in the damaged liver which could be partially associated with increased IL-4 production.
IFN-γ is an important Th1 cytokine [48]. It is produced predominantly by natural killer and Th1 cells, regulates their activity, and is critical for innate and adaptive immunity [47]. Our results demonstrated that serum IFN-γ level increased after CCl4-induced liver injury (PBS group) compared to the control group. Our results are consistent with previous studies showing that CCl4 injury caused elevation of serum IFN-γ levels [22, 53]. Previous study demonstrated that CCl4 injection into mice activated type 1 innate lymphoid cells (ILC1s), which, in turn, produced IFN- γ and protected mice from CCl4-induced acute liver injury. IFN-γ released from activated ILC1s promoted survival of the hepatocytes via upregulation of Bcl-xL [53]. Interestingly, IFN-γ followed the trend of the Th2 cytokine (IL-4), since its level increased after intravenous infusion of MSC(M). One may propose more than one explanation for this finding.
In the current study, experimental animals received syngeneic MSC(M) without prior immunosuppression with cyclosporine. Syngeneic transplantation is still believed to be the safest way of MSCs administration and does not cause any immune reaction [54]. It is possible that the immune system responds to infused MSC(M) as the cells are produced in culture and differ in size and protein expression patterns from the non-cultured MSC(M). Moreover, only low numbers of mesenchymal stromal cells are normally present in the circulation. Meanwhile, higher MSC numbers are present after MSC(M) infusion, thus, probably, activating the response. It is thus likely that the immune reaction induced after MSCs transplantation represented a response to cells perceived as foreign objects and/or presented at an unusual location, rather than a MSC-specific response [55].
It has also been reported that Th1 cytokines are involved into the graft rejection [56]. A previous work indicated that this cytokine may be a useful predictor of acute graft-versus-host disease (GvHD) [57]. Some murine studies reported high serum IFN- levels in acute GvHD [57-59]. Our in vivo study demonstrated that syngeneic MSCs are not fully immuneprivileged. Along with their therapeutic effects, they cause an immune response and may be rejected. The transplanted cells may become immunogenic during extracorporeal manipulations, despite identical genotypes of donor and recipient. It has been shown that the in vitro cultures of cells may alter their phenotype through epigenetic changes [54]. The opinion that syngeneic transplantation is safe comes from organ and tissue transplantology, where the biological material is transferred without any additional in vitro processing which is not the case in majority of experimental MSC transplants [54]. The strategies that reduce MSC immunogenicity can potentially prolong their in vivo persistence and improve the therapeutic effects. Thus, the modulation of immune responses is a prerequisite for preclinical and clinical studies in MSC therapy.
On the other hand, MSC-mediated immunosuppression was also reported to depend on prior activation by pro-inflammatory cytokines [60]. Previous studies also suggested that the immunosuppressive ability of MSC(M) require preliminary activation by IFN-γ alone, or in combination with other chemokines [61]. However, once MSC is activated, they can release several soluble factors, such as prostaglandin E2 (PGE2), inducible nitric-oxide synthase (iNOS), indoleamine 2,3-deoxigenase (IDO), and IL-6 that exert immunomodulatory effects on other cell types [60]. Therefore, elevated IFN-γ in the MSC(M) group may play a role in the immunomodulatory properties of MSC(M) [61]. Expression of IDO and other anti-inflammatory factors by MSCs is strongly stimulated under inflammatory conditions, suggesting that the immunomodulatory effects of MSCs act as a feedback mechanism to control ongoing immune responses [55]. However, further studies are required in order to elucidate the mechanism of immune response upon intravenous injection of syngeneic MSC(M).
Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Several mechanisms could explain the therapeutic effects of MSC(M) in liver injury [62], as follows: 1) potential migration of MSC(M) to damaged liver with possible differentiation into hepatocytes and promoted recovery from chemically induced liver damage [15]; 2) secretion of paracrine factors such as cytokines, hormones and growth factors, thus promoting tissue repair; 3) transfer of organelles (e.g., mitochondria) and/or molecules through tunneling nanotubes. 4) MSC-mediated transfer of proteins/peptides, hormones, RNA, and/or chemicals by extracellular vesicles, such as exosomes or microvesicles [63]. The contribution of paracrine effects has been further supported by recent studies reporting the therapeutic benefit of MSC-derived biomolecules for treatment of acute liver injury [62].
Conclusion
We presented that transplantation of MSC(M) could successfully promote liver regeneration and ameliorate CCl4-induced liver damage, but elicits an immune response upon intravenous injection in murine model. However, further investigations are needed to increase the reliability of the clinical efficacy of MSC(M), to evaluate safety of MSC(M) therapy, as well as clarify the exact therapeutic mechanism of MSC(M), determine optimal injection route, timing and dosage of MSC administration, optimal stem cell source, and, possibly, to develop therapeutic strategies aiming for improved effectiveness of MSC(M) transplantation. We hope that our findings will contribute to the improvement of MSC(M)-based therapies for liver disease.
Conflicts of interest
None declared.
References
-
Eom Y, Shim K, Baik S. Mesenchymal stem cell therapy for liver fibrosis. Korean J Intern Med. 2014; 30, 580-589.
doi: 10.3904/kjim.2015.30.5.580 - Chang Y, Liu J, Lin P, Sun L, Peng C, Luo G, Chen T, Lee R, Lin S, Harn H, Chiou T. Mesenchymal stem cells facilitate recovery from chemically induced liver damage and decrease liver fibrosis. Life Sciences, 85, 517-525 (2009). doi: 10.1016/j.lfs.2009.08.003
- Hegab M, Abd-Allah S, Badawey M, Saleh A, Metwally A, Fathy G, Nada S, Abdel-Rahman S, Saleh A, Fawzy A, Abu El-Magd M. Therapeutic potential effect of bone marrow-derived mesenchymal stem cells on chronic liver disease in murine Schistosomiasis Mansoni. J Parasit Dis, 42(2), 277-286 (2018). doi: 10.1007/s12639-018-0997-8
- Hao T, Chen J, Zhi S, Zhang Q, Chen G, Yu F. Comparison of bone marrow-vs. adipose tissue-derived mesenchymal stem cells for attenuating liver fibrosis. Exp Ther Med. 2017 Dec;14(6):5956-5964. doi: 10.3892/etm.2017.5333
- Haraguchi T, Tani K, Takagishi R, Oda Y, Itamoto K, Yamamoto N, Terai S, Sakaida I, Nakazawa H, Taura Y. Therapeutic potential of canine bone marrow stromal cells (BMSCs) in the carbon tetrachloride (CCl4) induced chronic liver dysfunction mouse model. J Vet Med Sci. 2012 May;74(5): 607-611. doi: 10.1292/jvms.11-0505
- Farouk S, Sabet S, Abu Zahra FA, El-Ghor AA. Bone marrow derived-mesenchymal stem cells downregulate IL17A dependent IL6/STAT3 signaling pathway in CCl4-induced rat liver fibrosis. PLoS One. 2018 Oct 22;13(10):e0206130.
doi: 10.1371/journal.pone.0206130 - Buck NE, Cheah DM, Elwood NJ, Wright PF, Allen KJ. Correction of copper metabolism is not sustained long term in Wilson's disease mice post bone marrow transplantation. Hepatol Int. 2008;2(1):72-79. doi: 10.1007/s12072-007-9039-9
- Oyagi S, Hirose M, Kojima M, Okuyama M, Kawase M, Nakamura T, Ohgushi H, Yagi K. Therapeutic effect of transplanting HGF-treated bone marrow mesenchymal cells into CCl4-injured rats. J Hepatol. 2006 Apr;44(4):742-748. doi: 10.1016/j.jhep.2005.10.026
- Popp FC, Slowik P, Eggenhofer E, Renner P, Lang SA, Stoeltzing O, Geissler EK, Piso P, Schlitt HJ, Dahlke MH. No contribution of multipotent mesenchymal stromal cells to liver regeneration in a rat model of prolonged hepatic injury. Stem Cells. 2007 Mar;25(3):639-645. doi: 10.1634/stemcells.2006-0515
- Abdel Aziz MT, Atta HM, Mahfouz S, Fouad HH, Roshdy NK, Ahmed HH, Rashed LA, Sabry D, Hassouna AA, Hasan NM. Therapeutic potential of bone marrow-derived mesenchymal stem cells on experimental liver fibrosis. Clin Biochem. 2007 Aug;40(12):893-899. doi: 10.1016/j.clinbiochem.2007.04.017
- Truong NH, Nguyen NH, Le TV, Vu NB, Huynh N, Nguyen TV, Le HM, Phan NK, Pham PV. Comparison of the treatment efficiency of bone marrow-derived mesenchymal stem cell transplantation via tail and portal veins in CCl4-Induced mouse liver fibrosis. Stem Cells Int. 2016;2016: 5720413. doi: 10.1155/2016/5720413
- Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019 Jan;70(1):151-171.
doi: 10.1016/j.jhep.2018.09.014 - Margini C, Vukotic R, Brodosi L, Bernardi M, Andreone P. Bone marrow derived stem cells for the treatment of end-stage liver disease. World J Gastroenterol. 2014;20(27):9098-9105. doi: 10.3748/wjg.v20.i27.9098
- Truong H, Nguyen H, Nguyen T, Le, Tran HG, Huynh N, Nguyen TV. Establishment of a standardized mouse model of hepatic fibrosis for biomedical research. Biomed Res Ther. 2014); 1, 9. doi: 10.7603/s40730-014-0009-2
- Wang M, Zhang X, Xiong XI, Yang Z, Li P, Wang J, Sun YU, Yang Z, Hoffman RM. Bone marrow mesenchymal stem cells reverse liver damage in a carbon tetrachloride-induced mouse model of chronic liver injury. In Vivo. 2016 May-Jun;30(3):187-193. PMID: 27107074
- Scholten D, Trebicka J, Liedtke C, Weiskirchen R. The carbon tetrachloride model in mice. Lab Anim. 2015; 49(1 Suppl):4-11.
doi: 10.1177/0023677215571192 - Adekomi DA, Oyesomi TO, Ajao MS, Ojo OA, Onikanni SA. Impact of liver damage on the histoarchitectural profile of the cerebellar cortex in rats. African J. Cell. Pathol. 2013. 1(1): 1-8. doi: 10.5897/AJCPATH13.005
- Zhu H, Guo ZK, Jiang XX, Li H, Wang XY, Yao HY, Zhang Y, Mao N. A protocol for isolation and culture of mesenchymal stem cells from mouse compact bone. Nat Protoc. 2010; 5(3):550-560. doi: 10.1038/nprot.2009.238
- Jiang T, Xu G, Wang Q, Yang L, Zheng L, Zhao J, Zhang X. In vitro expansion impaired the stemness of early passage mesenchymal stem cells for treatment of cartilage defects. Cell Death Dis. 8 (2017). doi: 10.1038/cddis.2017.215
- Yang YK, Ogando CR, Wang See C, Chang TY, Barabino GA. Changes in phenotype and differentiation potential of human mesenchymal stem cells aging in vitro. Stem Cell Res Ther. 2018; 9(1):131. doi: 10.1186/s13287-018-0876-3
- Ullah H, Khan A, Baig MW, Ullah N, Ahmed N, Tipu MK, Ali H, Khan S. Poncirin attenuates CCL4-induced liver injury through inhibition of oxidative stress and inflammatory cytokines in mice. BMC Complement Med Ther. 2020; 20(1):115. doi: 10.1186/s12906-020-02906-7
- Liu B, Fang Y, Yi R, Zhao X. Preventive Effect of Blueberry Extract on Liver Injury Induced by Carbon Tetrachloride in Mice. Foods. 2019 Feb 1;8(2):48. doi: 10.3390/foods8020048
- Lazic SE, Semenova E, Williams DP. Determining organ weight toxicity with Bayesian causal models: Improving on the analysis of relative organ weights. Sci Rep. 2020 Apr 20;10(1):6625. doi: 10.1038/s41598-020-63465-y
- Bencheikh N, Bouhrim M, Kharchoufa L, Choukri M, Bnouham M, Elachouri M. Protective Effect of Zizyphus lotus L. (Desf.) Fruit against CCl4-Induced Acute Liver Injury in Rat. Evid Based Complement Alternat Med. 2019 Dec 25;2019:6161593. doi: 10.1155/2019/6161593
- Shittu OK, Lawal B, Haruna GM, Berinyuy EB, Yusuf AA, Ibrahim AM. Hepato-curative effects of methanol extract from Nigerian Bee Propolis in carbon tetrachloride (CCl4) intoxicated rats. Eur. J. Biotechnol. Biosci. 2015; 3: 1-4.
- Gaim K, Gebru G, Abba S. The effect of arsenic on liver tissue of experimental animals (fishes and mice) – A review article. Int J Sci Res Publ. 2015; 5, 1-9.
- Kim WR, Flamm SL, Di Bisceglie AM, Bodenheimer HC. Public Policy Committee of the American Association for the Study of Liver Disease. Serum activity of alanine aminotransferase (ALT) as an indicator of health and disease. Hepatology. 2008; 47(4):1363-1370. doi: 10.1002/hep.22109
- Ebaid H, Bashandy SA, Alhazza IM, Rady A, El-Shehry S. Folic acid and melatonin ameliorate carbon tetrachloride-induced hepatic injury, oxidative stress and inflammation in rats. Nutr Metab (Lond). 2013; 10(1):20. doi: 10.1186/1743-7075-10-20
- Han CY, Sun TT, Xv GP, Wang SS, Gu JG, Liu CY. Berberine ameliorates CCl4 induced liver injury in rats through regulation of the Nrf2 Keap1 ARE and p53 signaling pathways. Mol Med Rep. 2019;20(4):3095-3102. doi: 10.3892/mmr.2019.10551
- Adewale OB, Adekomi DA, Muhameed OA. Neuronal alterations in the prefrontal cortex of rats with carbon tetrachloride (CCl4) induced hepatic damage. J. Clin. Pathol. Forensic Med. 2013; 4: 6-14. doi: 10.5897/JCPFM2013.0045
- Nguyen N, Le T, Do H, Ngo D, Le H, Truong N. Comparative treatment efficiency of adipose and bone marrow derived allogenic mesenchymal stem cell transplantation in mouse models of liver fibrosis. Biomed Res Ther. 2017; 4(6): 1374-1387.
doi: 10.15419/bmrat.v4i06.179 - Fernandez NJ, Kidney BA. Alkaline phosphatase: beyond the liver. Vet Clin Pathol. 2007; 36(3):223-233.
doi: 10.1111/j.1939-165x.2007.tb00216.x - Lazarov L. Markers for hepatocellular damage and affecting the biliary tract in the course of acute pancreatitis in dogs. Tradit. Mod. Vet. Med. 2021; 6: 3-10.
- Ibrahim EI, Enafie E, Farid AS. Star Anise (Illiciumverum) oil administration alleviates carbon tetrachloride-induced hepatotoxicity in rats. Benha Vet. Med. J. 2020; 39: 100-104. doi: 10.21608/bvmj.2020.51053.1303
- Lowe D, Sanvictores T, John S. Alkaline Phosphatase. In: StatPearls. Treasure Island (FL): StatPearls Publishing. 2022 Jan. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459201/
- Amer MA, El-missiry MA, El-nabi AAR. The Role of Ficus carica leaf extract in modulation of the experimentally induced hepatotoxic damage in male rats. Int J Adv Res. 2015; 3: 572-585.
- Oratz M, Rothschild MA, Schreiber SS, Lane BP. Spermine stimulation of CCl4 depressed protein synthesis in rabbits. Gastroenterology. 1980 Dec;79(6):1165-1173. PMID: 7439626
- Yuchong Z, Xinyun Z, Yao W, Huijiao L, Chunyan Y, Shu J, Wenyue Z, Chunmei W, Jinghui S, He L, Jianguang C. Anwulignan alleviates carbon tetrachloride-induced acute liver injury in mice. Nat. Prod. Commun. 2020; 15: 1-8. doi: 10.1177/1934578X20962679
- Luedde T, Kaplowitz N, Schwabe RF. Cell death and cell death responses in liver disease: mechanisms and clinical relevance. Gastroenterology. 2014;147(4):765-783.e4. doi: 10.1053/j.gastro.2014.07.018
- Hassan SS, Elbakry MH, Mangoura SA, Omar ZM. Evaluation of the effect of Gallic acid against carbon tetrachloride- induced liver injury in albino rats: histological, immunohistochemical and biochemical study. J Med Histol. 2018; 1(2): 202-215.
doi: 10.21608/JMH.2017.7928 - Ayatollahi M, Hesami Z, Jamshidzadeh A, Gramizadeh B. Antioxidant effects of bone marrow mesenchymal stem cell against carbon tetrachloride-induced oxidative damage in rat livers. Int J Organ Transplant Med. 2014;5(4):166-173. PMID: 25426285
- Lai HY, Chou TY, Tzeng CH, Lee OK. Cytokine profiles in various graft-versus-host disease target organs following hematopoietic stem cell transplantation. Cell Transplant. 2012;21(9):2033-2045. doi: 10.3727/096368912X653110
- Ma T, Gong K, Ao Q, Yan Y, Song B, Huang H, Zhang X, Gong Y. Intracerebral transplantation of adipose-derived mesenchymal stem cells alternatively activates microglia and ameliorates neuropathological deficits in Alzheimer's disease mice. Cell Transplant. 2013;22 Suppl 1:S113-126. doi: 10.3727/096368913X672181
- Woodward EA, Prêle CM, Nicholson SE, Kolesnik TB, Hart PH. The anti-inflammatory effects of interleukin-4 are not mediated by suppressor of cytokine signalling-1 (SOCS1). Immunology. 2010; 131(1):118-127. doi: 10.1111/j.1365-2567.2010.03281.x
- Clarke RM, Lyons A, O'Connell F, Deighan BF, Barry CE, Anyakoha NG, Nicolaou A, Lynch MA. A pivotal role for interleukin-4 in atorvastatin-associated neuroprotection in rat brain. J Biol Chem. 2008;283(4):1808-1817. doi: 10.1074/jbc.M707442200
- Ponomarev ED, Maresz K, Tan Y, Dittel BN. CNS-derived interleukin-4 is essential for the regulation of autoimmune inflammation and induces a state of alternative activation in microglial cells. J Neurosci. 2007; 27(40):10714-10721.
doi: 10.1523/JNEUROSCI.1922-07.2007 - Volpin G, Cohen M, Assaf M, Meir T, Katz R, Pollack S. Cytokine levels (IL-4, IL-6, IL-8 and TGFβ) as potential biomarkers of systemic inflammatory response in trauma patients. Int Orthop. 2014; 38(6):1303-1309. doi: 10.1007/s00264-013-2261-2
- Li JF, Zhang DJ, Geng T, Chen L, Huang H, Yin HL, Zhang YZ, Lou JY, Cao B, Wang YL. The potential of human umbilical cord-derived mesenchymal stem cells as a novel cellular therapy for multiple sclerosis. Cell Transplant. 2014; 23 Suppl 1:S113-22.
doi: 10.3727/096368914X685005 - Chai NL, Zhang XB, Chen SW, Fan KX, Linghu EQ. Umbilical cord-derived mesenchymal stem cells alleviate liver fibrosis in rats. World J Gastroenterol. 2016; 22(26):6036-6048. doi: 10.3748/wjg.v22.i26.6036
- Jia Z, Li F, Zeng X, Lv Y, Zhao S. The effects of local administration of mesenchymal stem cells on rat corneal allograft rejection. BMC Ophthalmol. 2018;18(1):139. doi: 10.1186/s12886-018-0802-6
- Cantarelli E, Pellegrini S, Citro A, Sordi V, Piemonti L. Bone marrow- and cord blood-derived stem cell transplantation for diabetes therapy. CellR4. 2015. 3: 1-21. doi: 10.1.1.683.1503&rep=rep1&type=pdf
- Singh G, Korkaya H. Cytokine regulation of stem cells. Peer J Prepr. 2016. 4:e2347v1. doi: 10.7287/peerj.preprints.2347v1
- Nabekura T, Riggan L, Hildreth AD, O'Sullivan TE, Shibuya A. Type 1 Innate Lymphoid Cells Protect Mice from Acute Liver Injury via Interferon-γ Secretion for Upregulating Bcl-xL Expression in Hepatocytes. Immunity. 2020; 52(1):96-108.e9.
doi: 10.1016/j.immuni.2019.11.004 - Gala K, Burdzińska A, Idziak M, Wilczek E, Pączek L. Transplantation of mesenchymal stem cells into the skeletal muscle induces cytokine generation. Cytokine. 2013; 64(1):243-50. doi: 10.1016/j.cyto.2013.06.314
- Hoogduijn MJ, Roemeling-van Rhijn M, Engela AU, Korevaar SS, Mensah FK, Franquesa M, de Bruin RW, Betjes MG, Weimar W, Baan CC. Mesenchymal stem cells induce an inflammatory response after intravenous infusion. Stem Cells Dev. 2013; 22(21):2825-35.
doi: 10.1089/scd.2013.0193 - Lu X, Cui J, Cui L, Luo Q, Cao Q, Yuan W, Zhang H. The effects of human umbilical cord-derived mesenchymal stem cell transplantation on endometrial receptivity are associated with Th1/Th2 balance change and uNK cell expression of uterine in autoimmune premature ovarian failure mice. Stem Cell Res Ther. 2019; 10(1):214. doi: 10.1186/s13287-019-1313-y
- Resende RG, Correia-Silva JD, Silva TA, Xavier SG, Bittencourt H, Gomez RS, Abreu MH. Saliva and blood interferon gamma levels and IFNG genotypes in acute graft-versus-host disease. Oral Dis. 2012; 18(8):816-22. doi: 10.1111/j.1601-0825.2012.01955.x
- Nakamura H, Komatsu K, Ayaki M, Kawamoto S, Murakami M, Uoshima N, Yagi T, Hasegawa T, Yasumi M, Karasuno T, Teshima H, Hiraoka A, Masaoka T, Serum levels of soluble IL-2 receptor, IL-12, IL-18, and IFN-gamma in patients with acute graft-versus-host disease after allogeneic bone marrow transplantation. J Allergy Clin Immunol. 2000; 106:45-50. doi: 10.1067/MAI.2000.106774
- Xu J, Wei J, Zhu X, Zhang X, Guan J, Wang J, Yin J, Xiao Y, Zhang Y. Interferon- g Levels Correlate with the Severity of Acute Stem Cell Transplantation. Biol Blood Marrow Transplant. 2013; 19: 196-201.
- Larocca RA, Moraes-Vieira PM, Bassi EJ, Semedo P, de Almeida DC, da Silva MB, Thornley T, Pacheco-Silva A, Câmara NO. Adipose tissue-derived mesenchymal stem cells increase skin allograft survival and inhibit Th-17 immune response. PLoS One. 2013; 8(10):e76396. doi: 10.1371/journal.pone.0076396
- Wu J, Wang Q, Fu X, Wu X, Gu C, Bi J, Xie F, Kang N, Liu X, Yan L, Cao Y, Xiao R. Influence of Immunogenicity of Allogeneic Bone Marrow Mesenchymal Stem Cells on Bone Tissue Engineering. Cell Transplant. 2016;25(2):229-42. doi: 10.3727/096368915X687967
- Piryaei A, Valojerdi M, Shahsavani M, Baharvand H. differentiation of bone marrow-derived mesenchymal stem cells into hepatocyte-like cells on nanofibers and their transplantation into a carbon tetrachloride-induced liver fibrosis. Stem Cell Rev Rep. 7, 103-118 (2011). doi: 10.1007/s12015-010-9126-5
- Spees JL, Lee RH, Gregory CA, Mechanisms of mesenchymal stem / stromal cell function. Stem Cell Res. Ther. 7, 1=13 (2016).
doi: 10.1186/s13287-016-0363-7
" ["~DETAIL_TEXT"]=> string(53759) "
Introduction
Although the liver has a considerable inherent regenerative capacity, a sufficient and prolonged may result into liver damage and onset of hepatic fibrosis [1]. For severe hepatic diseases, liver transplantation is one of the more effective treatments [2]. However, the tremendous gap between offered donor organs and those required for transplantation is the major limitation of liver replacement therapy [3]. High cost and transplant rejection following liver transplantation, have also largely limited its clinical application [4]. Therefore, alternative or adjuvant therapies are urgently needed [3].
Recently, regenerative medicine using different stem cells has been considered an attractive therapy for treating patients with severe liver disease [5], since these cells have the ability of self-renewal and maturation [6]. Stem cells are defined as undifferentiated cells from an embryo, fetus or an adult, which have the potential to produce various differentiated tissue cells under appropriate stimuli [5]. Bone marrow (BM) provides a more readily available source of cells [7]. Bone marrow cells are presently considered to be the most promising cell source for the cell therapy of various diseases [8]. Mesenchymal stromal cells (MSCs) have been documented as a promising technique for cell therapy and have been successfully applied in the treatment of various diseases [3]. Multipotent MSCs represent a remarkable stem cell population for application in liver-directed cell transplantation, since they are readily obtained from bone marrow aspirates and can be expanded in culture [9], through as many as 50 population doublings in about 10 weeks [10], thus producing a large number of potent cells [9]. In addition, BM-MSCs possess many advantages such as autologous sources, abundance of cells, an immune-modulatory capacity, secretion of cytokines and growth factors, homing to injury sites, and hepatic differentiation [11].
The present study aimed to investigate the therapeutic effect of bone marrow-derived mesenchymal stromal cells MSC(M) transplantation in alleviation of CCl4-induced liver damage in mice.
Materials and methods
Experimental Animals
Healthy male mice (Balb/c, 4-6 weeks) were used in this study. Mice were housed in clean cages of 65×25×15 cm containing woodchip bedding. Mice were housed in a temperature (temperature 24±2°C) and light-controlled room (12h light/dark cycle), with free access to food and water. The animals were left for two weeks to acclimatize to their surroundings before starting the experiment. All procedures were performed according to the Guide for the Care and Use of Laboratory Animals and the ethical standards of our institution.
Liver damage induction and MSC(M) preparation
To establish the liver-injury mice model, male Balb/c mice were intraperitoneally injected with (1 ml/kg body weight) of CCl4 dissolved in olive oil twice a week for 7 consecutive weeks.
In the current study, 4-6 weeks male healthy BALB/c mice were used as donors of MSC(M). Mice were sacrificed by cervical dislocation. MSC(M) were flushed from the medullary cavities of the tibia and femur using a needle with complete media (Dulbecco’s modified Eagle’s medium (DMEM) (Euroclone, Italy). The cells were grown in (4-5 ml) of DMEM medium supplemented with (20% FBS, 1% L-glutamine, 1% penicillin/streptomycin and 1.5 µg/ml amphotericin B) (Euroclone, Italy), in a 25 cm2 culture flask, and incubated at 37°C with 5% CO2. 24 h later, the culture medium was replaced to remove non-adherent cells and tissue debris. MSC(M) at passage 0 (P0) were used for transplantation.
Experimental Protocol
The mice were divided into the following groups:
• Control group (Group I): This group included healthy normal mice, which were not exposed and did not receive any treatment.
• Experimental group: mice were intraperitoneally injected with CCl4 (1 ml/kg body weight) of dissolved in olive oil twice a week for 7 consecutive weeks. After the last injection of CCl4, three mice were randomly selected from this group, blood samples were collected and serum ALT level was determined to ensure that liver damage had been induced before continuing the experiment. Mice in this group were randomly divided into two groups, as follows:
• PBS-treated group (Group II): mice were intravenously injected into the tail vein with 0.5 ml of phosphate buffer saline (PBS 1X).
• MSC(M) treated group (Group III): mice were intravenously injected with MSC(M). MSC(M) were washed with PBS (1X) and trypsinized with 0.25% trypsin, then (approximately 3×106 of MSC(M) per mouse) were re-suspended in (0.5 ml) of PBS and injected into the tail vein.
The mice from all studied groups (I, II, III) were sacrificed 4 weeks after transplantation. Venous blood and liver tissue samples were collected for further analyses. At the end of the experiment, the body weight and liver weight of the animals in all studied groups were determined. The liver to body weights ratio was determined as follows:
Liver to body Ratio = (liver weight (g)/(mouse body weight (g)-liver weight (g))) *100.
Laboratory analyses
Venous blood was collected, and blood samples were centrifuged at 3000 rpm for 5 minutes. Serum samples were subsequently analyzed to evaluate the activities of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and albumin.
Liver histology was performed to assess liver damage 4 weeks after MSC(M) transplantation. For light microscopic examination, the liver from each animal was carefully dissected and the specimens were fixed in 10% formalin for 48 hours. Paraffin sections were prepared and stained with hematoxylin and eosin (H&E) to display the histological details. Histological damage was evaluated by a pathologist who was blinded to the experimental groups.
At the end of the experiment, blood samples were collected and centrifuged at 3000 rpm for 5 min. The serum levels of interleukin-4 (IL-4) and IFN-γ cytokines were measured by ELISA assay kits according to the manufacturer’s instructions (Sun Red, China).
Results
The cultured MSCs were injected into syngeneic mice treated with hepatotoxic agent CCl4.
The results of this study showed remarkable significant increase in the liver weight and the liver weight to body weight ratio in PBS group compared with the normal control group. MSC(M) transplantation alleviated the increase in the liver weight and even decreased the ratio to a level closer to that of normal mice. There was no significant difference in the ratio between the MSC(M) treated group and the normal control group (Table 1).
Table 1. Body mass, liver weight and liver-to-body weight ratios of all studied groups
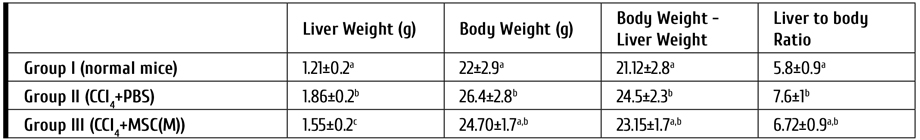
Note: All values are represented as mean ± SD. Mean values with different letters over the same column are significantly different at (P<0.05)
Serum levels of ALT, AST, ALP, and albumin were evaluated. After intraperitoneal injection of CCl4 for consecutive 7 weeks, serum levels of ALT were markedly increased in the experimental group (120±5.3), as compared to control group. PBS group exhibited markedly increased serum levels of ALT and ALP compared with control normal mice. The levels of ALT and ALP in the MSC(M)-treated group were significantly reduced compared to the PBS group being close to the normal control group. In addition, there was a significant decrease in serum levels of albumin in PBS group when compared with the control group. Significantly increased serum albumin levels were noticed in MSC(M)-treated group when compared to the PBS group. The levels of these parameters in control and MSC(M) treated group did not show any significant differences. Nearly similar AST levels were observed in MSC(M) and PBS groups (Table 2).
Table 2. Serum levels of ALT, AST, ALP, and albumin in the studied groups

Note: All values are represented as mean ± SD. Mean values marked with different letters (a,b) over the same column are significantly different at (P<0.05)
Histopathological analysis of liver sections
The liver of the control group was reddish-brown, with smooth and glossy surface. The liver of the PBS group was pale-brown, overtly swollen with coarse surface and necrotic spots. In MSC(M)-treated group, the liver surface was slightly coarse, less swollen, more reddish, and glossy compared with livers from the PBS group. Necrotic spots on the surface were noticeably reduced (Fig. 1).

Figure 1. Morphologic examination of the livers of the study groups. (A). The liver of the normal control group was smooth, lustrous, and reddish. (B) In the PBS group, the liver was pale-brown with coarse surface and overtly swollen. (C) In the mice receiving MSC(M) transplantation, the liver surface was slightly coarse, less swollen, more reddish, and lustrous than those of PBS group
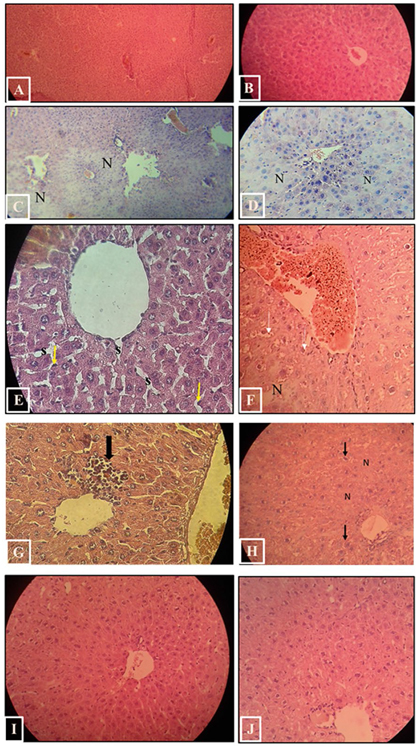
Figure 2. H&E-stained sections in Balb/c mice’s liver of the study groups. A, B. Control group. C–H. PBS group. C-D. Marked damage with disorganization of hepatic architecture, hepatocytes necrosis (N) can be seen. E. The blood sinusoids (s) are dilated and surrounded by Kupffer cells (arrows) with prominent nuclei. F. Vascular dilatation and congestion can be seen, some hepatocytes showed vacuolated cytoplasm (arrows). G. Inflammatory cell infiltration (arrow). H. hepatocytes with vacuolated cytoplasm (arrows). I, J. MSC(M) treated group. nearly normal organization of hepatic lobules. Hepatocytes appeared nearly similar to that of the control mice
Light microscope examination of normal liver tissue sections (control group) showed classical hepatic architecture (Fig. 2. A,B). Hepatocytes are arranged in cords that radiate from the central veins and separated by blood sinusoids. They had rounded nuclei and well-preserved cytoplasm. Some hepatocytes were binucleated. Blood sinusoids are lined by Kupffer cells and endothelial cells. Normal blood vessels and bile ducts were observed in Portal areas. PBS group showed marked affection with disorganization of hepatic architecture. Cellular necrosis was observed. Some hepatocytes appeared swollen with extensively vacuolated cytoplasm. Liver sections also revealed vascular dilatation and congestion in the portal areas and in the central veins. Some parts showed dilated blood sinusoids, which were lined by many Kupffer cells with prominent nuclei. Inflammatory cell infiltration was also detected (Fig. 2. C-H). The histopathological lesions were effectively attenuated to varying extents, in the MSC(M) treated group. Examination of H&E-stained sections showed nearly normal organization of hepatic lobules. A marked reduction of cellular necrosis was observed (Fig. 2, I, J). Hepatocytes appeared nearly similar to that of the control mice. Most hepatocytes had rounded nuclei and well-preserved cytoplasm, they were arranged around slightly dilated and congested central veins and separated by hepatic blood sinusoids. Few hepatocytes appeared with vacuolated cytoplasm. Liver sections demonstrated slight inflammatory cell infiltration. Portal areas appeared nearly normal with slightly congested blood vessels.
Serum Interleukin-4 (IL-4) and Interferon-γ (IFN-γ) Levels
To determine if MSC(M) transplantation affects the cytokine release, the serum levels of IL-4 and IFN-γ were measured by ELISA. As shown in Fig. 3, IL-4 level declined in the PBS group compared to the control group, and this effect was blocked by MSC(M) transfusion. Serum IL-4 level was elevated in MSC(M) treated group, as compared with the PBS group. Serum IFN-γ level was elevated in PBS group compared with the control group. The secretion of IFN-γ was higher in the MSC(M) treated group than in the control group and PBS group, at one month post transplantation.

Figure 3. Serum levels of IL-4, and IFN-γ cytokines. Sera were collected one month after MSC(M) transplantation, and cytokines were measured with enzyme-linked immunosorbent assay (ELISA). After MSC(M) transplantation, the IL-4, and IFN-γ levels were increased compared to PBS group
Discussion
Liver disease causes approximately two million deaths annually worldwide [12]. Therefore, there is an urgent need to develop new techniques to stimulate liver regeneration. In this regard, the potential of MSC therapy is of great interest in regard of liver regeneration [13]. Cell transplantation programs may provide a hopeful technology to replace organ transplantation [3].
Since CCl4 is toxic and may cause death, establishment of liver damage model in mouse is challenging [14]. When metabolized in liver by the cytochrome P450 monooxygenases, CCl4 produces free oxygen species [15, 16]. CCl4 activation to trichloromethyl and trichloromethyl peroxy radicals is stimulates lipid peroxidation and protein oxidation in the liver, causing membrane damage and liver injury [17].
Bone marrow mesenchymal stromal cells were isolated, cultured, and characterized in our previous study (data not shown). Although the isolated cells showed the characteristics of mesenchymal stromal cells, we guess that the population also contained a low proportion of hematopoietic stem cells, since we used the cells at the zero passage (P0), since hematopoietic stem cells have been reported to exist in MSC cultures even after nine in vitro passages [18].
In the current study, MSC(M) at passage 0 were used for transplantation, thus being different from the earlier experiments with MSC(M) therapy published so far, where MSC(M) were mostly injected at passage 3 (P3 MSC(M)).
The in vitro expansion is always required for MSC-based therapies in order to generate sufficient MSC(M) numbers for transplantation. Clinical recommendations for medical MSC usage usually apply cells from 3-5 passages. However, unexpected risks may occur during cell growth, including lack of phenotype, contamination and reduction in efficacy, possibly leading to therapy failure. It has also been reported that additional expansion might attenuate the stemness property of MSCs, thus contributing to reduction of therapeutic potential [19].
Previous report demonstrated that human MSCs subjected to extensive passaging may undergo morphological, phenotypic, and genetic changes [20]. It has been shown that the monolayer cultures significantly affect cell behavior, e.g., leading to cell senescence and impairment of multi-potency [19].
We have also studied the effects of MSC(M) transplantation upon body weight and liver weight. CCl4 is known to be a potent toxicant associated with the liver damage [21]. Determination of the liver weight to body weight ratio of mice may reflect structural and functional changes of the liver after CCl4 injury [22]. Since the body mass measures include the liver weight, it was subtracted from body weight to obtain a "liver-free" estimate of the body weight. Subtraction the liver weight is necessary because otherwise the measurable body weight will always reflect changes in the liver weight. It may make little difference in practice, because the liver weight is small, as compared with total body weight [23]. Significant increase in the liver weight was observed in PBS group compared with control group. This elevation in liver weight after CCl4 intoxication has been well supported by previous research [21, 24]. However, MSC(M) treatment seems to significantly reduce liver inflammation and hence, the liver weight. The ratio of liver weight to body mass was higher in PBS group with significant difference compared to the normal control group. MSC(M) treatment caused a non-significant decrease in this ratio compared to the PBS-treated group, but it became closer to the values of normal control group.
Estimation of biochemical indexes is widely accepted as a biomarker of liver damage [25]. Enzymes represent sensitive metabolic markers, thus even slight changes in enzyme activities would affect the organism [26]. Serum ALT level is usually elevated in case of serious liver damage and the extent of organ damage depends on the type of toxin, its mechanism of action and duration of exposure [26]. Serum ALT activity is a reliable and sensitive marker of liver disease [27].
The present study revealed a marked increase in the level of ALT upon exposure to CCl4 for 7 weeks (experimental group), which indicates considerable hepatocellular injury [28].
Exposure to CCl4 leads to liver injury [15]. Oxidative stress is considered to be the major pathogenic process of CCl4-induced liver injury [29]. This process causes changes in the of cell membrane permeability [15]. As a result, cytoplasmic ALT can leak into the bloodstream, and serum ALT level is increased [29], and can be determined [30]. In this study, we did not use liver toxin after transplantation of MSC(M). During treatment, it is important to eliminate the pathogen, in order to treat the disease efficiently without causing unnecessary complications. Such a strategy has the advantage of enhancing the recipient’s therapy regimen [31].
The results showed a decrease in ALT level in the PBS group compared to experimental group, which is explained by self-recovery and regeneration of mouse livers after CCl4 injection was discontinued. However, alleviation of liver damage occurred significantly faster in mice treated with MSC(M) than in untreated mice. MSC(M)-treated mice showed statistically significant improvement when compared to the PBS-treated group. These results reflect the important role of MSC(M) and show that MSC(M) transplantation can enhance regenerative capacity of the liver and improve affected tissues.
Alkaline phosphatase activity is a very useful serum biochemical marker of liver disease [32]. The present study revealed a significant increase in ALP level of PBS-treated group compared with MSC(M)-treated group. Liver ALP is synthesized by the bile duct. Previously, ALP was thought to be increased, due to inability of liver cells to release the enzyme with bile. It is, however, accepted that ALP activity is increased due to higher enzyme synthesis [33], with involvement of biliary ways [34]. The increased hepatic enzyme activity clearly parallels the rise in serum alkaline phosphatase activity, which is primarily caused by increased ALP mRNA translation (mediated by elevated bile acid concentration), and increased secretion of ALP into serum via canalicular leakage into the hepatic sinusoids by still unclear mechanisms [35].
Albumin synthesis is highly sensitive to CCl4 effects [36]. Albumin and other hepatic secretory proteins are synthesized by polysomes bound to the endoplasmic reticulum. CCl4 causes damage to hepatocytes, including disruption of hepatic cells with polysome disaggregation and decrease in protein synthesis [37].
On the other hand, it was thought that CCl4 toxicity leads to damage of Golgi apparatus, which, in turn, negatively affects protein packaging and release from hepatocytes [36]. One month after MSC(M) transplantation, liver injury markers (ALT and ALP) showed positive changes compared with PBS group. A significant increase in serum albumin level was noticed in MSC(M)-treated group compared to the PBS group, which suggests that transplantation of MSC(M) results in significant restoration of specific liver function.
The liver histology studies were consistent with biochemical results, suggesting an improvement in MSC(M) treated group compared with PBS group. In the current study, CCl4 intoxication resulted in disorganization of hepatic architecture, necrosis of hepatocytes, cytoplasm vacuolation, vascular congestion and dilation, dilatation of sinusoids and infiltration with inflammatory cell, as revealed by light microscope examination of livers from PBS group. Carbon tetrachloride is metabolized by cytochrome to reactive oxygen species, resulting in membrane lipid peroxidation and oxidative stress injury, and, finally, hepatocyte necrosis and dysfunction [38]. Necrosis is viewed as a largely unregulated sequence of physicochemical stress, characterized by mitochondrial impairment, adenosine triphosphate (ATP) depletion, and subsequent failure of ATP-dependent ion pumps. These changes result in rapid swelling of cells and cell organelles ("oncosis") accompanied by the formation of membrane "blebs" and eventual cell rupture [39].
Microscopical examination of liver sections in PBS group showed vascular dilatation and congestion. Dilatation may be caused by increase levels of prostaglandin synthesis that leads to smooth muscle relaxation and vasodilatation [40]. The congestion may be due to fluid loss from the dilated vessels, so they become filled with red blood cells [40]. This congestion, as suggested by Hong et al., (1991) and Wijetunga et al., (2003), is a typical early index of hepatotoxicity [17]. The liver sections of PBS group exhibited cytoplasmic vacuolation and increase in cell volume which are due to the loss of the cell's regulating mechanism for pumping out water from the inside. Cell swelling in CCl4 intoxication is due to altered cell membrane permeability. CCl4 is a non-polar lipophilic substance, thus leading to changes in the physical and chemical properties of both cytoplasmic and mitochondrial lipid membranes, and resulting in disruption of Na+/K+ pump and migration of interstitial fluids to the hepatocytes [40].
After MSC(M) transplantation, marked reduction in liver damage was observed, as compared to PBS group, thus suggesting heterogeneous response to cell therapy in distinct animals. Microscopic examination showed improvement in the histopathological changes induced by CCl4, and in hepatic lobular architecture. Previous study has shown that MSCs secrete several factors, i.e., nitric oxide and prostaglandin E2, which enhance antioxidant protection, inhibit oxidative factors, and reduce the hepatocyte necrosis [11]. However, the mechanism by which MSC(M) repair liver damage remain unclear [41].
The studies of IL4 and IFN-γ serum levels by ELISA have shown some differences in IL-4 between CCl4-treated animals and controls. Cytokines are a class of polypeptide micro-molecules secreted by various cells, which are able to regulate cell growth and differentiation, immune function, inflammation and wound healing [15]. E.g., interferon-γ (IFN-γ) is the hallmark cytokine of T helper 1 (Th1) cells, whereas interleukin 4 (IL-4) has the same role in Th2 cells [42]. The results showed that the serum level of IL-4 decreased in PBS treated mice compared to the control group (intact mice). After MSC(M) transplantation, the IL-4 level increased.
Differences in IL-4 levels between serum of mice treated and those not treated with MSC(M) proved that MSC(M) had a therapeutic effect. IL-4 is one of the widely recognized immune regulatory cytokines capable of suppressing inflammation [43]. It has been used successfully in the treatment of inflammatory diseases in animal models, and in experimental studies, IL-4 injections significantly improved the condition of psoriatic dermatitis [44]. Several studies suggest that treatments that act to increase the concentration of interleukin-4 in tissues may be beneficial in treating inflammation [45, 46].
However, the exact mechanisms by which IL-4 exerts its anti-inflammatory effects are not well understood [44]. The lower levels of the anti-inflammatory cytokine IL-4 found in the injured group compared to control is in accordance with previous studies showing suppression of this cytokine during acute injury [47-49].
Our results are consistent with prior studies that showed that the IL-4 level was higher in the MSC-treated group compared to the untreated mice [43, 49, 50]. It has been demonstrated that MSCs caused the TH2 cells to increase secretion of IL-4 [51, 52]. Chai et al., (2016) have shown that MSC(M) may increase IL-4 secretion in rats with liver fibrosis induced by dimethyl nitrosamine (DMN) both in vitro and in vivo [49]. Jia et al., (2018) indicated that the IL-4 mRNA expression was significantly higher in corneal grafts from MSCs-treated groups when compared with controls (PBS group) [50]. Our data showed that anti-inflammatory cytokine IL-4 exhibited remarkable increase in the MSC(M)-treated group. These findings may explain how MSC(M) mediate the cell repair in the damaged liver which could be partially associated with increased IL-4 production.
IFN-γ is an important Th1 cytokine [48]. It is produced predominantly by natural killer and Th1 cells, regulates their activity, and is critical for innate and adaptive immunity [47]. Our results demonstrated that serum IFN-γ level increased after CCl4-induced liver injury (PBS group) compared to the control group. Our results are consistent with previous studies showing that CCl4 injury caused elevation of serum IFN-γ levels [22, 53]. Previous study demonstrated that CCl4 injection into mice activated type 1 innate lymphoid cells (ILC1s), which, in turn, produced IFN- γ and protected mice from CCl4-induced acute liver injury. IFN-γ released from activated ILC1s promoted survival of the hepatocytes via upregulation of Bcl-xL [53]. Interestingly, IFN-γ followed the trend of the Th2 cytokine (IL-4), since its level increased after intravenous infusion of MSC(M). One may propose more than one explanation for this finding.
In the current study, experimental animals received syngeneic MSC(M) without prior immunosuppression with cyclosporine. Syngeneic transplantation is still believed to be the safest way of MSCs administration and does not cause any immune reaction [54]. It is possible that the immune system responds to infused MSC(M) as the cells are produced in culture and differ in size and protein expression patterns from the non-cultured MSC(M). Moreover, only low numbers of mesenchymal stromal cells are normally present in the circulation. Meanwhile, higher MSC numbers are present after MSC(M) infusion, thus, probably, activating the response. It is thus likely that the immune reaction induced after MSCs transplantation represented a response to cells perceived as foreign objects and/or presented at an unusual location, rather than a MSC-specific response [55].
It has also been reported that Th1 cytokines are involved into the graft rejection [56]. A previous work indicated that this cytokine may be a useful predictor of acute graft-versus-host disease (GvHD) [57]. Some murine studies reported high serum IFN- levels in acute GvHD [57-59]. Our in vivo study demonstrated that syngeneic MSCs are not fully immuneprivileged. Along with their therapeutic effects, they cause an immune response and may be rejected. The transplanted cells may become immunogenic during extracorporeal manipulations, despite identical genotypes of donor and recipient. It has been shown that the in vitro cultures of cells may alter their phenotype through epigenetic changes [54]. The opinion that syngeneic transplantation is safe comes from organ and tissue transplantology, where the biological material is transferred without any additional in vitro processing which is not the case in majority of experimental MSC transplants [54]. The strategies that reduce MSC immunogenicity can potentially prolong their in vivo persistence and improve the therapeutic effects. Thus, the modulation of immune responses is a prerequisite for preclinical and clinical studies in MSC therapy.
On the other hand, MSC-mediated immunosuppression was also reported to depend on prior activation by pro-inflammatory cytokines [60]. Previous studies also suggested that the immunosuppressive ability of MSC(M) require preliminary activation by IFN-γ alone, or in combination with other chemokines [61]. However, once MSC is activated, they can release several soluble factors, such as prostaglandin E2 (PGE2), inducible nitric-oxide synthase (iNOS), indoleamine 2,3-deoxigenase (IDO), and IL-6 that exert immunomodulatory effects on other cell types [60]. Therefore, elevated IFN-γ in the MSC(M) group may play a role in the immunomodulatory properties of MSC(M) [61]. Expression of IDO and other anti-inflammatory factors by MSCs is strongly stimulated under inflammatory conditions, suggesting that the immunomodulatory effects of MSCs act as a feedback mechanism to control ongoing immune responses [55]. However, further studies are required in order to elucidate the mechanism of immune response upon intravenous injection of syngeneic MSC(M).
Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Several mechanisms could explain the therapeutic effects of MSC(M) in liver injury [62], as follows: 1) potential migration of MSC(M) to damaged liver with possible differentiation into hepatocytes and promoted recovery from chemically induced liver damage [15]; 2) secretion of paracrine factors such as cytokines, hormones and growth factors, thus promoting tissue repair; 3) transfer of organelles (e.g., mitochondria) and/or molecules through tunneling nanotubes. 4) MSC-mediated transfer of proteins/peptides, hormones, RNA, and/or chemicals by extracellular vesicles, such as exosomes or microvesicles [63]. The contribution of paracrine effects has been further supported by recent studies reporting the therapeutic benefit of MSC-derived biomolecules for treatment of acute liver injury [62].
Conclusion
We presented that transplantation of MSC(M) could successfully promote liver regeneration and ameliorate CCl4-induced liver damage, but elicits an immune response upon intravenous injection in murine model. However, further investigations are needed to increase the reliability of the clinical efficacy of MSC(M), to evaluate safety of MSC(M) therapy, as well as clarify the exact therapeutic mechanism of MSC(M), determine optimal injection route, timing and dosage of MSC administration, optimal stem cell source, and, possibly, to develop therapeutic strategies aiming for improved effectiveness of MSC(M) transplantation. We hope that our findings will contribute to the improvement of MSC(M)-based therapies for liver disease.
Conflicts of interest
None declared.
References
-
Eom Y, Shim K, Baik S. Mesenchymal stem cell therapy for liver fibrosis. Korean J Intern Med. 2014; 30, 580-589.
doi: 10.3904/kjim.2015.30.5.580 - Chang Y, Liu J, Lin P, Sun L, Peng C, Luo G, Chen T, Lee R, Lin S, Harn H, Chiou T. Mesenchymal stem cells facilitate recovery from chemically induced liver damage and decrease liver fibrosis. Life Sciences, 85, 517-525 (2009). doi: 10.1016/j.lfs.2009.08.003
- Hegab M, Abd-Allah S, Badawey M, Saleh A, Metwally A, Fathy G, Nada S, Abdel-Rahman S, Saleh A, Fawzy A, Abu El-Magd M. Therapeutic potential effect of bone marrow-derived mesenchymal stem cells on chronic liver disease in murine Schistosomiasis Mansoni. J Parasit Dis, 42(2), 277-286 (2018). doi: 10.1007/s12639-018-0997-8
- Hao T, Chen J, Zhi S, Zhang Q, Chen G, Yu F. Comparison of bone marrow-vs. adipose tissue-derived mesenchymal stem cells for attenuating liver fibrosis. Exp Ther Med. 2017 Dec;14(6):5956-5964. doi: 10.3892/etm.2017.5333
- Haraguchi T, Tani K, Takagishi R, Oda Y, Itamoto K, Yamamoto N, Terai S, Sakaida I, Nakazawa H, Taura Y. Therapeutic potential of canine bone marrow stromal cells (BMSCs) in the carbon tetrachloride (CCl4) induced chronic liver dysfunction mouse model. J Vet Med Sci. 2012 May;74(5): 607-611. doi: 10.1292/jvms.11-0505
- Farouk S, Sabet S, Abu Zahra FA, El-Ghor AA. Bone marrow derived-mesenchymal stem cells downregulate IL17A dependent IL6/STAT3 signaling pathway in CCl4-induced rat liver fibrosis. PLoS One. 2018 Oct 22;13(10):e0206130.
doi: 10.1371/journal.pone.0206130 - Buck NE, Cheah DM, Elwood NJ, Wright PF, Allen KJ. Correction of copper metabolism is not sustained long term in Wilson's disease mice post bone marrow transplantation. Hepatol Int. 2008;2(1):72-79. doi: 10.1007/s12072-007-9039-9
- Oyagi S, Hirose M, Kojima M, Okuyama M, Kawase M, Nakamura T, Ohgushi H, Yagi K. Therapeutic effect of transplanting HGF-treated bone marrow mesenchymal cells into CCl4-injured rats. J Hepatol. 2006 Apr;44(4):742-748. doi: 10.1016/j.jhep.2005.10.026
- Popp FC, Slowik P, Eggenhofer E, Renner P, Lang SA, Stoeltzing O, Geissler EK, Piso P, Schlitt HJ, Dahlke MH. No contribution of multipotent mesenchymal stromal cells to liver regeneration in a rat model of prolonged hepatic injury. Stem Cells. 2007 Mar;25(3):639-645. doi: 10.1634/stemcells.2006-0515
- Abdel Aziz MT, Atta HM, Mahfouz S, Fouad HH, Roshdy NK, Ahmed HH, Rashed LA, Sabry D, Hassouna AA, Hasan NM. Therapeutic potential of bone marrow-derived mesenchymal stem cells on experimental liver fibrosis. Clin Biochem. 2007 Aug;40(12):893-899. doi: 10.1016/j.clinbiochem.2007.04.017
- Truong NH, Nguyen NH, Le TV, Vu NB, Huynh N, Nguyen TV, Le HM, Phan NK, Pham PV. Comparison of the treatment efficiency of bone marrow-derived mesenchymal stem cell transplantation via tail and portal veins in CCl4-Induced mouse liver fibrosis. Stem Cells Int. 2016;2016: 5720413. doi: 10.1155/2016/5720413
- Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019 Jan;70(1):151-171.
doi: 10.1016/j.jhep.2018.09.014 - Margini C, Vukotic R, Brodosi L, Bernardi M, Andreone P. Bone marrow derived stem cells for the treatment of end-stage liver disease. World J Gastroenterol. 2014;20(27):9098-9105. doi: 10.3748/wjg.v20.i27.9098
- Truong H, Nguyen H, Nguyen T, Le, Tran HG, Huynh N, Nguyen TV. Establishment of a standardized mouse model of hepatic fibrosis for biomedical research. Biomed Res Ther. 2014); 1, 9. doi: 10.7603/s40730-014-0009-2
- Wang M, Zhang X, Xiong XI, Yang Z, Li P, Wang J, Sun YU, Yang Z, Hoffman RM. Bone marrow mesenchymal stem cells reverse liver damage in a carbon tetrachloride-induced mouse model of chronic liver injury. In Vivo. 2016 May-Jun;30(3):187-193. PMID: 27107074
- Scholten D, Trebicka J, Liedtke C, Weiskirchen R. The carbon tetrachloride model in mice. Lab Anim. 2015; 49(1 Suppl):4-11.
doi: 10.1177/0023677215571192 - Adekomi DA, Oyesomi TO, Ajao MS, Ojo OA, Onikanni SA. Impact of liver damage on the histoarchitectural profile of the cerebellar cortex in rats. African J. Cell. Pathol. 2013. 1(1): 1-8. doi: 10.5897/AJCPATH13.005
- Zhu H, Guo ZK, Jiang XX, Li H, Wang XY, Yao HY, Zhang Y, Mao N. A protocol for isolation and culture of mesenchymal stem cells from mouse compact bone. Nat Protoc. 2010; 5(3):550-560. doi: 10.1038/nprot.2009.238
- Jiang T, Xu G, Wang Q, Yang L, Zheng L, Zhao J, Zhang X. In vitro expansion impaired the stemness of early passage mesenchymal stem cells for treatment of cartilage defects. Cell Death Dis. 8 (2017). doi: 10.1038/cddis.2017.215
- Yang YK, Ogando CR, Wang See C, Chang TY, Barabino GA. Changes in phenotype and differentiation potential of human mesenchymal stem cells aging in vitro. Stem Cell Res Ther. 2018; 9(1):131. doi: 10.1186/s13287-018-0876-3
- Ullah H, Khan A, Baig MW, Ullah N, Ahmed N, Tipu MK, Ali H, Khan S. Poncirin attenuates CCL4-induced liver injury through inhibition of oxidative stress and inflammatory cytokines in mice. BMC Complement Med Ther. 2020; 20(1):115. doi: 10.1186/s12906-020-02906-7
- Liu B, Fang Y, Yi R, Zhao X. Preventive Effect of Blueberry Extract on Liver Injury Induced by Carbon Tetrachloride in Mice. Foods. 2019 Feb 1;8(2):48. doi: 10.3390/foods8020048
- Lazic SE, Semenova E, Williams DP. Determining organ weight toxicity with Bayesian causal models: Improving on the analysis of relative organ weights. Sci Rep. 2020 Apr 20;10(1):6625. doi: 10.1038/s41598-020-63465-y
- Bencheikh N, Bouhrim M, Kharchoufa L, Choukri M, Bnouham M, Elachouri M. Protective Effect of Zizyphus lotus L. (Desf.) Fruit against CCl4-Induced Acute Liver Injury in Rat. Evid Based Complement Alternat Med. 2019 Dec 25;2019:6161593. doi: 10.1155/2019/6161593
- Shittu OK, Lawal B, Haruna GM, Berinyuy EB, Yusuf AA, Ibrahim AM. Hepato-curative effects of methanol extract from Nigerian Bee Propolis in carbon tetrachloride (CCl4) intoxicated rats. Eur. J. Biotechnol. Biosci. 2015; 3: 1-4.
- Gaim K, Gebru G, Abba S. The effect of arsenic on liver tissue of experimental animals (fishes and mice) – A review article. Int J Sci Res Publ. 2015; 5, 1-9.
- Kim WR, Flamm SL, Di Bisceglie AM, Bodenheimer HC. Public Policy Committee of the American Association for the Study of Liver Disease. Serum activity of alanine aminotransferase (ALT) as an indicator of health and disease. Hepatology. 2008; 47(4):1363-1370. doi: 10.1002/hep.22109
- Ebaid H, Bashandy SA, Alhazza IM, Rady A, El-Shehry S. Folic acid and melatonin ameliorate carbon tetrachloride-induced hepatic injury, oxidative stress and inflammation in rats. Nutr Metab (Lond). 2013; 10(1):20. doi: 10.1186/1743-7075-10-20
- Han CY, Sun TT, Xv GP, Wang SS, Gu JG, Liu CY. Berberine ameliorates CCl4 induced liver injury in rats through regulation of the Nrf2 Keap1 ARE and p53 signaling pathways. Mol Med Rep. 2019;20(4):3095-3102. doi: 10.3892/mmr.2019.10551
- Adewale OB, Adekomi DA, Muhameed OA. Neuronal alterations in the prefrontal cortex of rats with carbon tetrachloride (CCl4) induced hepatic damage. J. Clin. Pathol. Forensic Med. 2013; 4: 6-14. doi: 10.5897/JCPFM2013.0045
- Nguyen N, Le T, Do H, Ngo D, Le H, Truong N. Comparative treatment efficiency of adipose and bone marrow derived allogenic mesenchymal stem cell transplantation in mouse models of liver fibrosis. Biomed Res Ther. 2017; 4(6): 1374-1387.
doi: 10.15419/bmrat.v4i06.179 - Fernandez NJ, Kidney BA. Alkaline phosphatase: beyond the liver. Vet Clin Pathol. 2007; 36(3):223-233.
doi: 10.1111/j.1939-165x.2007.tb00216.x - Lazarov L. Markers for hepatocellular damage and affecting the biliary tract in the course of acute pancreatitis in dogs. Tradit. Mod. Vet. Med. 2021; 6: 3-10.
- Ibrahim EI, Enafie E, Farid AS. Star Anise (Illiciumverum) oil administration alleviates carbon tetrachloride-induced hepatotoxicity in rats. Benha Vet. Med. J. 2020; 39: 100-104. doi: 10.21608/bvmj.2020.51053.1303
- Lowe D, Sanvictores T, John S. Alkaline Phosphatase. In: StatPearls. Treasure Island (FL): StatPearls Publishing. 2022 Jan. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459201/
- Amer MA, El-missiry MA, El-nabi AAR. The Role of Ficus carica leaf extract in modulation of the experimentally induced hepatotoxic damage in male rats. Int J Adv Res. 2015; 3: 572-585.
- Oratz M, Rothschild MA, Schreiber SS, Lane BP. Spermine stimulation of CCl4 depressed protein synthesis in rabbits. Gastroenterology. 1980 Dec;79(6):1165-1173. PMID: 7439626
- Yuchong Z, Xinyun Z, Yao W, Huijiao L, Chunyan Y, Shu J, Wenyue Z, Chunmei W, Jinghui S, He L, Jianguang C. Anwulignan alleviates carbon tetrachloride-induced acute liver injury in mice. Nat. Prod. Commun. 2020; 15: 1-8. doi: 10.1177/1934578X20962679
- Luedde T, Kaplowitz N, Schwabe RF. Cell death and cell death responses in liver disease: mechanisms and clinical relevance. Gastroenterology. 2014;147(4):765-783.e4. doi: 10.1053/j.gastro.2014.07.018
- Hassan SS, Elbakry MH, Mangoura SA, Omar ZM. Evaluation of the effect of Gallic acid against carbon tetrachloride- induced liver injury in albino rats: histological, immunohistochemical and biochemical study. J Med Histol. 2018; 1(2): 202-215.
doi: 10.21608/JMH.2017.7928 - Ayatollahi M, Hesami Z, Jamshidzadeh A, Gramizadeh B. Antioxidant effects of bone marrow mesenchymal stem cell against carbon tetrachloride-induced oxidative damage in rat livers. Int J Organ Transplant Med. 2014;5(4):166-173. PMID: 25426285
- Lai HY, Chou TY, Tzeng CH, Lee OK. Cytokine profiles in various graft-versus-host disease target organs following hematopoietic stem cell transplantation. Cell Transplant. 2012;21(9):2033-2045. doi: 10.3727/096368912X653110
- Ma T, Gong K, Ao Q, Yan Y, Song B, Huang H, Zhang X, Gong Y. Intracerebral transplantation of adipose-derived mesenchymal stem cells alternatively activates microglia and ameliorates neuropathological deficits in Alzheimer's disease mice. Cell Transplant. 2013;22 Suppl 1:S113-126. doi: 10.3727/096368913X672181
- Woodward EA, Prêle CM, Nicholson SE, Kolesnik TB, Hart PH. The anti-inflammatory effects of interleukin-4 are not mediated by suppressor of cytokine signalling-1 (SOCS1). Immunology. 2010; 131(1):118-127. doi: 10.1111/j.1365-2567.2010.03281.x
- Clarke RM, Lyons A, O'Connell F, Deighan BF, Barry CE, Anyakoha NG, Nicolaou A, Lynch MA. A pivotal role for interleukin-4 in atorvastatin-associated neuroprotection in rat brain. J Biol Chem. 2008;283(4):1808-1817. doi: 10.1074/jbc.M707442200
- Ponomarev ED, Maresz K, Tan Y, Dittel BN. CNS-derived interleukin-4 is essential for the regulation of autoimmune inflammation and induces a state of alternative activation in microglial cells. J Neurosci. 2007; 27(40):10714-10721.
doi: 10.1523/JNEUROSCI.1922-07.2007 - Volpin G, Cohen M, Assaf M, Meir T, Katz R, Pollack S. Cytokine levels (IL-4, IL-6, IL-8 and TGFβ) as potential biomarkers of systemic inflammatory response in trauma patients. Int Orthop. 2014; 38(6):1303-1309. doi: 10.1007/s00264-013-2261-2
- Li JF, Zhang DJ, Geng T, Chen L, Huang H, Yin HL, Zhang YZ, Lou JY, Cao B, Wang YL. The potential of human umbilical cord-derived mesenchymal stem cells as a novel cellular therapy for multiple sclerosis. Cell Transplant. 2014; 23 Suppl 1:S113-22.
doi: 10.3727/096368914X685005 - Chai NL, Zhang XB, Chen SW, Fan KX, Linghu EQ. Umbilical cord-derived mesenchymal stem cells alleviate liver fibrosis in rats. World J Gastroenterol. 2016; 22(26):6036-6048. doi: 10.3748/wjg.v22.i26.6036
- Jia Z, Li F, Zeng X, Lv Y, Zhao S. The effects of local administration of mesenchymal stem cells on rat corneal allograft rejection. BMC Ophthalmol. 2018;18(1):139. doi: 10.1186/s12886-018-0802-6
- Cantarelli E, Pellegrini S, Citro A, Sordi V, Piemonti L. Bone marrow- and cord blood-derived stem cell transplantation for diabetes therapy. CellR4. 2015. 3: 1-21. doi: 10.1.1.683.1503&rep=rep1&type=pdf
- Singh G, Korkaya H. Cytokine regulation of stem cells. Peer J Prepr. 2016. 4:e2347v1. doi: 10.7287/peerj.preprints.2347v1
- Nabekura T, Riggan L, Hildreth AD, O'Sullivan TE, Shibuya A. Type 1 Innate Lymphoid Cells Protect Mice from Acute Liver Injury via Interferon-γ Secretion for Upregulating Bcl-xL Expression in Hepatocytes. Immunity. 2020; 52(1):96-108.e9.
doi: 10.1016/j.immuni.2019.11.004 - Gala K, Burdzińska A, Idziak M, Wilczek E, Pączek L. Transplantation of mesenchymal stem cells into the skeletal muscle induces cytokine generation. Cytokine. 2013; 64(1):243-50. doi: 10.1016/j.cyto.2013.06.314
- Hoogduijn MJ, Roemeling-van Rhijn M, Engela AU, Korevaar SS, Mensah FK, Franquesa M, de Bruin RW, Betjes MG, Weimar W, Baan CC. Mesenchymal stem cells induce an inflammatory response after intravenous infusion. Stem Cells Dev. 2013; 22(21):2825-35.
doi: 10.1089/scd.2013.0193 - Lu X, Cui J, Cui L, Luo Q, Cao Q, Yuan W, Zhang H. The effects of human umbilical cord-derived mesenchymal stem cell transplantation on endometrial receptivity are associated with Th1/Th2 balance change and uNK cell expression of uterine in autoimmune premature ovarian failure mice. Stem Cell Res Ther. 2019; 10(1):214. doi: 10.1186/s13287-019-1313-y
- Resende RG, Correia-Silva JD, Silva TA, Xavier SG, Bittencourt H, Gomez RS, Abreu MH. Saliva and blood interferon gamma levels and IFNG genotypes in acute graft-versus-host disease. Oral Dis. 2012; 18(8):816-22. doi: 10.1111/j.1601-0825.2012.01955.x
- Nakamura H, Komatsu K, Ayaki M, Kawamoto S, Murakami M, Uoshima N, Yagi T, Hasegawa T, Yasumi M, Karasuno T, Teshima H, Hiraoka A, Masaoka T, Serum levels of soluble IL-2 receptor, IL-12, IL-18, and IFN-gamma in patients with acute graft-versus-host disease after allogeneic bone marrow transplantation. J Allergy Clin Immunol. 2000; 106:45-50. doi: 10.1067/MAI.2000.106774
- Xu J, Wei J, Zhu X, Zhang X, Guan J, Wang J, Yin J, Xiao Y, Zhang Y. Interferon- g Levels Correlate with the Severity of Acute Stem Cell Transplantation. Biol Blood Marrow Transplant. 2013; 19: 196-201.
- Larocca RA, Moraes-Vieira PM, Bassi EJ, Semedo P, de Almeida DC, da Silva MB, Thornley T, Pacheco-Silva A, Câmara NO. Adipose tissue-derived mesenchymal stem cells increase skin allograft survival and inhibit Th-17 immune response. PLoS One. 2013; 8(10):e76396. doi: 10.1371/journal.pone.0076396
- Wu J, Wang Q, Fu X, Wu X, Gu C, Bi J, Xie F, Kang N, Liu X, Yan L, Cao Y, Xiao R. Influence of Immunogenicity of Allogeneic Bone Marrow Mesenchymal Stem Cells on Bone Tissue Engineering. Cell Transplant. 2016;25(2):229-42. doi: 10.3727/096368915X687967
- Piryaei A, Valojerdi M, Shahsavani M, Baharvand H. differentiation of bone marrow-derived mesenchymal stem cells into hepatocyte-like cells on nanofibers and their transplantation into a carbon tetrachloride-induced liver fibrosis. Stem Cell Rev Rep. 7, 103-118 (2011). doi: 10.1007/s12015-010-9126-5
- Spees JL, Lee RH, Gregory CA, Mechanisms of mesenchymal stem / stromal cell function. Stem Cell Res. Ther. 7, 1=13 (2016).
doi: 10.1186/s13287-016-0363-7
" ["DETAIL_TEXT_TYPE"]=> string(4) "html" ["~DETAIL_TEXT_TYPE"]=> string(4) "html" ["PREVIEW_TEXT"]=> string(0) "" ["~PREVIEW_TEXT"]=> string(0) "" ["PREVIEW_TEXT_TYPE"]=> string(4) "text" ["~PREVIEW_TEXT_TYPE"]=> string(4) "text" ["PREVIEW_PICTURE"]=> NULL ["~PREVIEW_PICTURE"]=> NULL ["LANG_DIR"]=> string(4) "/ru/" ["~LANG_DIR"]=> string(4) "/ru/" ["SORT"]=> string(2) "10" ["~SORT"]=> string(2) "10" ["CODE"]=> string(100) "terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen" ["~CODE"]=> string(100) "terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen" ["EXTERNAL_ID"]=> string(4) "2056" ["~EXTERNAL_ID"]=> string(4) "2056" ["IBLOCK_TYPE_ID"]=> string(7) "journal" ["~IBLOCK_TYPE_ID"]=> string(7) "journal" ["IBLOCK_CODE"]=> string(7) "volumes" ["~IBLOCK_CODE"]=> string(7) "volumes" ["IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["~IBLOCK_EXTERNAL_ID"]=> string(1) "2" ["LID"]=> string(2) "s2" ["~LID"]=> string(2) "s2" ["EDIT_LINK"]=> NULL ["DELETE_LINK"]=> NULL ["DISPLAY_ACTIVE_FROM"]=> string(0) "" ["IPROPERTY_VALUES"]=> array(18) { ["ELEMENT_META_TITLE"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["ELEMENT_META_KEYWORDS"]=> string(0) "" ["ELEMENT_META_DESCRIPTION"]=> string(424) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)" ["ELEMENT_PREVIEW_PICTURE_FILE_ALT"]=> string(3244) "<p style="text-align: justify;">Терапия стволовыми клетками является перспективнмым видом лечения болезней печени. В данной работе изучали эффект мезенхимных стволовых клеток (МСК), полученных из костного мозга, для лечения повреждения печени, вызванного CCl<sub>4</sub>. </p> <h3>Материалы и методы</h3> <p style="text-align: justify;">Мышам Balb/c вводили CCl<sub>4</sub> (1 мл/кг массы тела) или физиологический раствор (в качестве контроля) дважды в неделю на протяжении 7 недель. Затем животным вводили внутривенно МСК с пассажа 0. Через 4 нед. после трансплантации определяли уровни АЛаТ, АСаТ, щелочной фосфатазы и альбумина в сыворотке крови, проводили гистологическое исследование печени, и измеряли уровни IL-4 и IFN-γ посредством методики ИФА.</> <h3>Результаты</h3> <p style="text-align: justify;">По сравнению с группой контроля (с введением физ.раствора), в группе, леченной МСК, были показаны более низкие уровни АЛаТ и АСаТ. Были также выявлены позитивные изменения сывороточного альбумина. Данные гистологического исследования согласовывались с данными биохимических анализов, указывая на лучшие показатели в группе, леченной МСК, по сравнению с контрольной группой. Кроме того, трансплантация МСК сопровождалась повышением продукции IL-4 и IFN-γ по сравнению с контролем.</p> <h3>Выводы</h3> <p style="text-align: justify;">Наши результаты показали, что трансплантация сингенных МСК может облегчить восстановление после химической индукции повреждения печени, несмотря на вызванный иммунный ответ. Поэтому трансплантация МСК может быть основой для новой концепции лечения заболеваний печени.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Мыши, повреждение печени, CCl<sub>4</sub>, стволовые клетки костного мозга, мезенхимные, трансплантация клеток.</p>" ["ELEMENT_PREVIEW_PICTURE_FILE_TITLE"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["ELEMENT_DETAIL_PICTURE_FILE_ALT"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["ELEMENT_DETAIL_PICTURE_FILE_TITLE"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_META_TITLE"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_META_KEYWORDS"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_META_DESCRIPTION"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_PICTURE_FILE_ALT"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_PICTURE_FILE_TITLE"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_PICTURE_FILE_NAME"]=> string(100) "terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen" ["SECTION_DETAIL_PICTURE_FILE_ALT"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_DETAIL_PICTURE_FILE_TITLE"]=> string(279) "Терапевтический потенциал трансплантации мышам мезенхимных клеток костного мозга для ослабления повреждения печени, вызванного CCL4 (исследование in vivo)" ["SECTION_DETAIL_PICTURE_FILE_NAME"]=> string(100) "terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen" ["ELEMENT_PREVIEW_PICTURE_FILE_NAME"]=> string(100) "terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen" ["ELEMENT_DETAIL_PICTURE_FILE_NAME"]=> string(100) "terapevticheskiy-potentsial-transplantatsii-mysham-mezenkhimnykh-kletok-kostnogo-mozga-dlya-oslablen" } ["FIELDS"]=> array(1) { ["IBLOCK_SECTION_ID"]=> string(3) "209" } ["PROPERTIES"]=> array(18) { ["KEYWORDS"]=> array(36) { ["ID"]=> string(2) "19" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:46:01" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(27) "Ключевые слова" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "KEYWORDS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "19" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "4" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "Y" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "Y" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(27) "Ключевые слова" ["~DEFAULT_VALUE"]=> string(0) "" } ["SUBMITTED"]=> array(36) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28578" ["VALUE"]=> string(22) "10/13/2021 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "10/13/2021 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL } ["ACCEPTED"]=> array(36) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28579" ["VALUE"]=> string(22) "01/28/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/28/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL } ["PUBLISHED"]=> array(36) { ["ID"]=> string(2) "22" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Дата публикации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "PUBLISHED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "22" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Дата публикации" ["~DEFAULT_VALUE"]=> NULL } ["CONTACT"]=> array(36) { ["ID"]=> string(2) "23" ["TIMESTAMP_X"]=> string(19) "2015-09-03 14:43:05" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(14) "Контакт" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "CONTACT" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "23" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(14) "Контакт" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHORS"]=> array(36) { ["ID"]=> string(2) "24" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:45:07" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "AUTHORS" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "E" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "Y" ["XML_ID"]=> string(2) "24" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "3" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(13) "EAutocomplete" ["USER_TYPE_SETTINGS"]=> array(9) { ["VIEW"]=> string(1) "E" ["SHOW_ADD"]=> string(1) "Y" ["MAX_WIDTH"]=> int(0) ["MIN_HEIGHT"]=> int(24) ["MAX_HEIGHT"]=> int(1000) ["BAN_SYM"]=> string(2) ",;" ["REP_SYM"]=> string(1) " " ["OTHER_REP_SYM"]=> string(0) "" ["IBLOCK_MESS"]=> string(1) "N" } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> bool(false) ["VALUE"]=> bool(false) ["DESCRIPTION"]=> bool(false) ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> bool(false) ["~DESCRIPTION"]=> bool(false) ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_RU"]=> array(36) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28580" ["VALUE"]=> array(2) { ["TEXT"]=> string(302) "<p>Дима Джуджех<sup>1</sup>, Абдулджалил Гревати<sup>1</sup>, Чади Суккариех<sup>2</sup>, Аднан Альмаррави<sup>1</sup>, Джамал А. Н. Дарвича<sup>3</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(230) "
Дима Джуджех1, Абдулджалил Гревати1, Чади Суккариех2, Аднан Альмаррави1, Джамал А. Н. Дарвича3
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_RU"]=> array(36) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28581" ["VALUE"]=> array(2) { ["TEXT"]=> string(636) "<p><sup>1</sup> Департамент биотехнологической инженерии, Факультет технической инженерии, Университет Алеппо, Сирия<br> <sup>2</sup> Департамент биологии животных, Факультет наук, Университет Дамаска, Сирия<br> <sup>3</sup> Департамент фармакологии и токсикологии, Факультет фармации, Арабский международный университет, Сирия </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(576) "1 Департамент биотехнологической инженерии, Факультет технической инженерии, Университет Алеппо, Сирия
2 Департамент биологии животных, Факультет наук, Университет Дамаска, Сирия
3 Департамент фармакологии и токсикологии, Факультет фармации, Арабский международный университет, Сирия
Терапия стволовыми клетками является перспективнмым видом лечения болезней печени. В данной работе изучали эффект мезенхимных стволовых клеток (МСК), полученных из костного мозга, для лечения повреждения печени, вызванного CCl4.
Материалы и методы
Мышам Balb/c вводили CCl4 (1 мл/кг массы тела) или физиологический раствор (в качестве контроля) дважды в неделю на протяжении 7 недель. Затем животным вводили внутривенно МСК с пассажа 0. Через 4 нед. после трансплантации определяли уровни АЛаТ, АСаТ, щелочной фосфатазы и альбумина в сыворотке крови, проводили гистологическое исследование печени, и измеряли уровни IL-4 и IFN-γ посредством методики ИФА.
Результаты
По сравнению с группой контроля (с введением физ.раствора), в группе, леченной МСК, были показаны более низкие уровни АЛаТ и АСаТ. Были также выявлены позитивные изменения сывороточного альбумина. Данные гистологического исследования согласовывались с данными биохимических анализов, указывая на лучшие показатели в группе, леченной МСК, по сравнению с контрольной группой. Кроме того, трансплантация МСК сопровождалась повышением продукции IL-4 и IFN-γ по сравнению с контролем.
Выводы
Наши результаты показали, что трансплантация сингенных МСК может облегчить восстановление после химической индукции повреждения печени, несмотря на вызванный иммунный ответ. Поэтому трансплантация МСК может быть основой для новой концепции лечения заболеваний печени.
Ключевые слова
Мыши, повреждение печени, CCl4, стволовые клетки костного мозга, мезенхимные, трансплантация клеток.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["DOI"]=> array(36) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28583" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-58-68" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-58-68" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" } ["AUTHOR_EN"]=> array(36) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28584" ["VALUE"]=> array(2) { ["TEXT"]=> string(234) "<p>Dima Joujeh<sup>1</sup>, Abduljalil Ghrewaty<sup>1</sup>, Chadi Soukkarieh<sup>2</sup>, Adnan Almarrawi<sup>1</sup>, Jamal Abdul Naser Darwicha<sup>3</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(162) "Dima Joujeh1, Abduljalil Ghrewaty1, Chadi Soukkarieh2, Adnan Almarrawi1, Jamal Abdul Naser Darwicha3
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["ORGANIZATION_EN"]=> array(36) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28585" ["VALUE"]=> array(2) { ["TEXT"]=> string(992) "<p><sup>1</sup> Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria<br> <sup>2</sup> Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria<br> <sup>3</sup> Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria</p><br> <p><b>Correspondence:</b><br> Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria<br> Phone: (+963) 994-046-745<br> E-mail: dimajoujeh@gmail.com</p><br> <p><b>Citation:</b> Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL<sub>4</sub>-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(842) "1 Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
2 Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria
3 Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria
Correspondence:
Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
Phone: (+963) 994-046-745
E-mail: dimajoujeh@gmail.com
Citation: Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["SUMMARY_EN"]=> array(36) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28586" ["VALUE"]=> array(2) { ["TEXT"]=> string(1807) "<p style="text-align: justify;">Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl<sub>4</sub> treatment was investigated.</p> <h3>Materials and methods</h3> <p style="text-align: justify;">Balb/c mice were injected by (1 ml/kg body weight) of CCl<sub>4</sub> twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ. </p> <h3>Results</h3> <p style="text-align: justify;">As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.</p> <h3>Conclusion</h3> <p style="text-align: justify;">Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.</p> <h2>Keywords</h2> <p style="text-align: justify;">Mice, liver damage, CCl<sub>4</sub>, bone marrow stromal cells, mesenchymal, cell transplantation.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1613) "Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl4 treatment was investigated.
Materials and methods
Balb/c mice were injected by (1 ml/kg body weight) of CCl4 twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ.
Results
As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.
Conclusion
Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.
Keywords
Mice, liver damage, CCl4, bone marrow stromal cells, mesenchymal, cell transplantation.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["NAME_EN"]=> array(36) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28587" ["VALUE"]=> string(145) "Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(145) "Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" } ["FULL_TEXT_RU"]=> array(36) { ["ID"]=> string(2) "42" ["TIMESTAMP_X"]=> string(19) "2015-09-07 20:29:18" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(23) "Полный текст" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(12) "FULL_TEXT_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "42" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(23) "Полный текст" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } } ["PDF_RU"]=> array(36) { ["ID"]=> string(2) "43" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF RUS" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_RU" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "43" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28588" ["VALUE"]=> string(4) "2813" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2813" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF RUS" ["~DEFAULT_VALUE"]=> string(0) "" } ["PDF_EN"]=> array(36) { ["ID"]=> string(2) "44" ["TIMESTAMP_X"]=> string(19) "2015-09-09 16:05:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(7) "PDF ENG" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(6) "PDF_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "F" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "44" ["FILE_TYPE"]=> string(18) "doc, txt, rtf, pdf" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28589" ["VALUE"]=> string(4) "2814" ["DESCRIPTION"]=> NULL ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(4) "2814" ["~DESCRIPTION"]=> NULL ["~NAME"]=> string(7) "PDF ENG" ["~DEFAULT_VALUE"]=> string(0) "" } ["NAME_LONG"]=> array(36) { ["ID"]=> string(2) "45" ["TIMESTAMP_X"]=> string(19) "2023-04-13 00:55:00" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(72) "Название (для очень длинных заголовков)" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "NAME_LONG" ["DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "45" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(80) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> NULL ["VALUE"]=> string(0) "" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(0) "" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(72) "Название (для очень длинных заголовков)" ["~DEFAULT_VALUE"]=> array(2) { ["TYPE"]=> string(4) "HTML" ["TEXT"]=> string(0) "" } } } ["DISPLAY_PROPERTIES"]=> array(10) { ["AUTHOR_EN"]=> array(37) { ["ID"]=> string(2) "37" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(6) "Author" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "37" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28584" ["VALUE"]=> array(2) { ["TEXT"]=> string(234) "<p>Dima Joujeh<sup>1</sup>, Abduljalil Ghrewaty<sup>1</sup>, Chadi Soukkarieh<sup>2</sup>, Adnan Almarrawi<sup>1</sup>, Jamal Abdul Naser Darwicha<sup>3</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(162) "Dima Joujeh1, Abduljalil Ghrewaty1, Chadi Soukkarieh2, Adnan Almarrawi1, Jamal Abdul Naser Darwicha3
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(6) "Author" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(162) "Dima Joujeh1, Abduljalil Ghrewaty1, Chadi Soukkarieh2, Adnan Almarrawi1, Jamal Abdul Naser Darwicha3
" } ["SUMMARY_EN"]=> array(37) { ["ID"]=> string(2) "39" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Description / Summary" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "39" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28586" ["VALUE"]=> array(2) { ["TEXT"]=> string(1807) "<p style="text-align: justify;">Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl<sub>4</sub> treatment was investigated.</p> <h3>Materials and methods</h3> <p style="text-align: justify;">Balb/c mice were injected by (1 ml/kg body weight) of CCl<sub>4</sub> twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ. </p> <h3>Results</h3> <p style="text-align: justify;">As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.</p> <h3>Conclusion</h3> <p style="text-align: justify;">Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.</p> <h2>Keywords</h2> <p style="text-align: justify;">Mice, liver damage, CCl<sub>4</sub>, bone marrow stromal cells, mesenchymal, cell transplantation.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(1613) "Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl4 treatment was investigated.
Materials and methods
Balb/c mice were injected by (1 ml/kg body weight) of CCl4 twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ.
Results
As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.
Conclusion
Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.
Keywords
Mice, liver damage, CCl4, bone marrow stromal cells, mesenchymal, cell transplantation.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Description / Summary" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(1613) "Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl4 treatment was investigated.
Materials and methods
Balb/c mice were injected by (1 ml/kg body weight) of CCl4 twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ.
Results
As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.
Conclusion
Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.
Keywords
Mice, liver damage, CCl4, bone marrow stromal cells, mesenchymal, cell transplantation.
" } ["DOI"]=> array(37) { ["ID"]=> string(2) "28" ["TIMESTAMP_X"]=> string(19) "2016-04-06 14:11:12" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(3) "DOI" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(3) "DOI" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "28" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28583" ["VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-58-68" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-58-68" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(3) "DOI" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(38) "10.18620/ctt-1866-8836-2022-11-1-58-68" } ["NAME_EN"]=> array(37) { ["ID"]=> string(2) "40" ["TIMESTAMP_X"]=> string(19) "2015-09-03 10:49:47" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(4) "Name" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(7) "NAME_EN" ["DEFAULT_VALUE"]=> string(0) "" ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "80" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "40" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "Y" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> NULL ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28587" ["VALUE"]=> string(145) "Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(145) "Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(4) "Name" ["~DEFAULT_VALUE"]=> string(0) "" ["DISPLAY_VALUE"]=> string(145) "Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)" } ["ORGANIZATION_EN"]=> array(37) { ["ID"]=> string(2) "38" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:02:59" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Organization" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_EN" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "38" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28585" ["VALUE"]=> array(2) { ["TEXT"]=> string(992) "<p><sup>1</sup> Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria<br> <sup>2</sup> Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria<br> <sup>3</sup> Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria</p><br> <p><b>Correspondence:</b><br> Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria<br> Phone: (+963) 994-046-745<br> E-mail: dimajoujeh@gmail.com</p><br> <p><b>Citation:</b> Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL<sub>4</sub>-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(842) "1 Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
2 Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria
3 Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria
Correspondence:
Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
Phone: (+963) 994-046-745
E-mail: dimajoujeh@gmail.com
Citation: Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Organization" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(842) "1 Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
2 Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria
3 Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria
Correspondence:
Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
Phone: (+963) 994-046-745
E-mail: dimajoujeh@gmail.com
Citation: Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.
" } ["AUTHOR_RU"]=> array(37) { ["ID"]=> string(2) "25" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(12) "Авторы" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "AUTHOR_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "25" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28580" ["VALUE"]=> array(2) { ["TEXT"]=> string(302) "<p>Дима Джуджех<sup>1</sup>, Абдулджалил Гревати<sup>1</sup>, Чади Суккариех<sup>2</sup>, Аднан Альмаррави<sup>1</sup>, Джамал А. Н. Дарвича<sup>3</sup></p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(230) "Дима Джуджех1, Абдулджалил Гревати1, Чади Суккариех2, Аднан Альмаррави1, Джамал А. Н. Дарвича3
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(12) "Авторы" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(230) "Дима Джуджех1, Абдулджалил Гревати1, Чади Суккариех2, Аднан Альмаррави1, Джамал А. Н. Дарвича3
" } ["SUBMITTED"]=> array(37) { ["ID"]=> string(2) "20" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(21) "Дата подачи" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(9) "SUBMITTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "20" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28578" ["VALUE"]=> string(22) "10/13/2021 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "10/13/2021 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(21) "Дата подачи" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "10/13/2021 12:00:00 am" } ["ACCEPTED"]=> array(37) { ["ID"]=> string(2) "21" ["TIMESTAMP_X"]=> string(19) "2015-09-02 17:21:42" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(25) "Дата принятия" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(8) "ACCEPTED" ["DEFAULT_VALUE"]=> NULL ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "21" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(8) "DateTime" ["USER_TYPE_SETTINGS"]=> NULL ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28579" ["VALUE"]=> string(22) "01/28/2022 12:00:00 am" ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> string(22) "01/28/2022 12:00:00 am" ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(25) "Дата принятия" ["~DEFAULT_VALUE"]=> NULL ["DISPLAY_VALUE"]=> string(32) "01/28/2022 12:00:00 am" } ["SUMMARY_RU"]=> array(37) { ["ID"]=> string(2) "27" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(29) "Описание/Резюме" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(10) "SUMMARY_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "27" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28582" ["VALUE"]=> array(2) { ["TEXT"]=> string(3244) "<p style="text-align: justify;">Терапия стволовыми клетками является перспективнмым видом лечения болезней печени. В данной работе изучали эффект мезенхимных стволовых клеток (МСК), полученных из костного мозга, для лечения повреждения печени, вызванного CCl<sub>4</sub>. </p> <h3>Материалы и методы</h3> <p style="text-align: justify;">Мышам Balb/c вводили CCl<sub>4</sub> (1 мл/кг массы тела) или физиологический раствор (в качестве контроля) дважды в неделю на протяжении 7 недель. Затем животным вводили внутривенно МСК с пассажа 0. Через 4 нед. после трансплантации определяли уровни АЛаТ, АСаТ, щелочной фосфатазы и альбумина в сыворотке крови, проводили гистологическое исследование печени, и измеряли уровни IL-4 и IFN-γ посредством методики ИФА.</> <h3>Результаты</h3> <p style="text-align: justify;">По сравнению с группой контроля (с введением физ.раствора), в группе, леченной МСК, были показаны более низкие уровни АЛаТ и АСаТ. Были также выявлены позитивные изменения сывороточного альбумина. Данные гистологического исследования согласовывались с данными биохимических анализов, указывая на лучшие показатели в группе, леченной МСК, по сравнению с контрольной группой. Кроме того, трансплантация МСК сопровождалась повышением продукции IL-4 и IFN-γ по сравнению с контролем.</p> <h3>Выводы</h3> <p style="text-align: justify;">Наши результаты показали, что трансплантация сингенных МСК может облегчить восстановление после химической индукции повреждения печени, несмотря на вызванный иммунный ответ. Поэтому трансплантация МСК может быть основой для новой концепции лечения заболеваний печени.</p> <h2>Ключевые слова</h2> <p style="text-align: justify;">Мыши, повреждение печени, CCl<sub>4</sub>, стволовые клетки костного мозга, мезенхимные, трансплантация клеток.</p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(3050) "Терапия стволовыми клетками является перспективнмым видом лечения болезней печени. В данной работе изучали эффект мезенхимных стволовых клеток (МСК), полученных из костного мозга, для лечения повреждения печени, вызванного CCl4.
Материалы и методы
Мышам Balb/c вводили CCl4 (1 мл/кг массы тела) или физиологический раствор (в качестве контроля) дважды в неделю на протяжении 7 недель. Затем животным вводили внутривенно МСК с пассажа 0. Через 4 нед. после трансплантации определяли уровни АЛаТ, АСаТ, щелочной фосфатазы и альбумина в сыворотке крови, проводили гистологическое исследование печени, и измеряли уровни IL-4 и IFN-γ посредством методики ИФА.
Результаты
По сравнению с группой контроля (с введением физ.раствора), в группе, леченной МСК, были показаны более низкие уровни АЛаТ и АСаТ. Были также выявлены позитивные изменения сывороточного альбумина. Данные гистологического исследования согласовывались с данными биохимических анализов, указывая на лучшие показатели в группе, леченной МСК, по сравнению с контрольной группой. Кроме того, трансплантация МСК сопровождалась повышением продукции IL-4 и IFN-γ по сравнению с контролем.
Выводы
Наши результаты показали, что трансплантация сингенных МСК может облегчить восстановление после химической индукции повреждения печени, несмотря на вызванный иммунный ответ. Поэтому трансплантация МСК может быть основой для новой концепции лечения заболеваний печени.
Ключевые слова
Мыши, повреждение печени, CCl4, стволовые клетки костного мозга, мезенхимные, трансплантация клеток.
" ["TYPE"]=> string(4) "HTML" } ["~DESCRIPTION"]=> string(0) "" ["~NAME"]=> string(29) "Описание/Резюме" ["~DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["DISPLAY_VALUE"]=> string(3050) "Терапия стволовыми клетками является перспективнмым видом лечения болезней печени. В данной работе изучали эффект мезенхимных стволовых клеток (МСК), полученных из костного мозга, для лечения повреждения печени, вызванного CCl4.
Материалы и методы
Мышам Balb/c вводили CCl4 (1 мл/кг массы тела) или физиологический раствор (в качестве контроля) дважды в неделю на протяжении 7 недель. Затем животным вводили внутривенно МСК с пассажа 0. Через 4 нед. после трансплантации определяли уровни АЛаТ, АСаТ, щелочной фосфатазы и альбумина в сыворотке крови, проводили гистологическое исследование печени, и измеряли уровни IL-4 и IFN-γ посредством методики ИФА.
Результаты
По сравнению с группой контроля (с введением физ.раствора), в группе, леченной МСК, были показаны более низкие уровни АЛаТ и АСаТ. Были также выявлены позитивные изменения сывороточного альбумина. Данные гистологического исследования согласовывались с данными биохимических анализов, указывая на лучшие показатели в группе, леченной МСК, по сравнению с контрольной группой. Кроме того, трансплантация МСК сопровождалась повышением продукции IL-4 и IFN-γ по сравнению с контролем.
Выводы
Наши результаты показали, что трансплантация сингенных МСК может облегчить восстановление после химической индукции повреждения печени, несмотря на вызванный иммунный ответ. Поэтому трансплантация МСК может быть основой для новой концепции лечения заболеваний печени.
Ключевые слова
Мыши, повреждение печени, CCl4, стволовые клетки костного мозга, мезенхимные, трансплантация клеток.
" } ["ORGANIZATION_RU"]=> array(37) { ["ID"]=> string(2) "26" ["TIMESTAMP_X"]=> string(19) "2015-09-02 18:01:20" ["IBLOCK_ID"]=> string(1) "2" ["NAME"]=> string(22) "Организации" ["ACTIVE"]=> string(1) "Y" ["SORT"]=> string(3) "500" ["CODE"]=> string(15) "ORGANIZATION_RU" ["DEFAULT_VALUE"]=> array(2) { ["TEXT"]=> string(0) "" ["TYPE"]=> string(4) "HTML" } ["PROPERTY_TYPE"]=> string(1) "S" ["ROW_COUNT"]=> string(1) "1" ["COL_COUNT"]=> string(2) "30" ["LIST_TYPE"]=> string(1) "L" ["MULTIPLE"]=> string(1) "N" ["XML_ID"]=> string(2) "26" ["FILE_TYPE"]=> string(0) "" ["MULTIPLE_CNT"]=> string(1) "5" ["TMP_ID"]=> NULL ["LINK_IBLOCK_ID"]=> string(1) "0" ["WITH_DESCRIPTION"]=> string(1) "N" ["SEARCHABLE"]=> string(1) "N" ["FILTRABLE"]=> string(1) "N" ["IS_REQUIRED"]=> string(1) "N" ["VERSION"]=> string(1) "1" ["USER_TYPE"]=> string(4) "HTML" ["USER_TYPE_SETTINGS"]=> array(1) { ["height"]=> int(200) } ["HINT"]=> string(0) "" ["PROPERTY_VALUE_ID"]=> string(5) "28581" ["VALUE"]=> array(2) { ["TEXT"]=> string(636) "<p><sup>1</sup> Департамент биотехнологической инженерии, Факультет технической инженерии, Университет Алеппо, Сирия<br> <sup>2</sup> Департамент биологии животных, Факультет наук, Университет Дамаска, Сирия<br> <sup>3</sup> Департамент фармакологии и токсикологии, Факультет фармации, Арабский международный университет, Сирия </p>" ["TYPE"]=> string(4) "HTML" } ["DESCRIPTION"]=> string(0) "" ["VALUE_ENUM"]=> NULL ["VALUE_XML_ID"]=> NULL ["VALUE_SORT"]=> NULL ["~VALUE"]=> array(2) { ["TEXT"]=> string(576) "1 Департамент биотехнологической инженерии, Факультет технической инженерии, Университет Алеппо, Сирия
2 Департамент биологии животных, Факультет наук, Университет Дамаска, Сирия
3 Департамент фармакологии и токсикологии, Факультет фармации, Арабский международный университет, Сирия
1 Департамент биотехнологической инженерии, Факультет технической инженерии, Университет Алеппо, Сирия
2 Департамент биологии животных, Факультет наук, Университет Дамаска, Сирия
3 Департамент фармакологии и токсикологии, Факультет фармации, Арабский международный университет, Сирия
04/15/2022 03:53:21 pm

Kulagin A. D. (St. Petersburg, Russia)
Wagemaker G. (Rotterdam, Netherlands)
Zander A. R. (Hamburg, Germany)
Fehse B. (Hamburg, Germany)
Chukhlovin A. B. (St. Petersburg, Russia)
Aleynikova O. V. (Minsk, Belarus)
Borset M. (Trondheim, Norway)
Chechetkin A. V. (St. Petersburg, Russia)
Fibbe W. (Leiden, Netherlands)
Gale R. P. (Los Angeles, USA)
Galibin O. V. (St. Petersburg, Russia)
Hehlmann R. (Mannheim, Germany)
Hölzer D. (Frankfurt a.M., Germany)
Klimko N. N. (St. Petersburg, Russia)
Kolb H.-J. (München, Germany)
Kröger N. (Hamburg, Germany)
Lange C. (Hamburg, Germany)
Mamaev N. N. (St. Petersburg, Russia)
Mikhailova N. B. (St. Petersburg, Russia)
Moiseev I. S. (St. Petersburg, Russia)
Nagler A. (Tel-Aviv, Israel)
Nemkov A. S. (St. Petersburg, Russia)
Paramonov I. V. (Kirov, Russia)
Roumiantsev A. G. (Moscow, Russia)
Savchenko V. G. (Moscow, Russia)
Smirnov A. V. (St. Petersburg, Russia)
Uss A. L. (Minsk, Belarus)
Zubarovskaya L. S. (St. Petersburg, Russia)
Editorial
Professor Alexander D. Kulagin, Editor-in-Chief, Cellular Therapy and Transplantation Journal
Review articles
Karina A. Sergeenko1,3, Yana Yu. Dokuchaeva1, Irina O. Kostareva1, Tim Z. Aliev1, Anna Yu. Elfimova1, Nikolay G. Stepanian1, Yury V. Lozovan1, Natalya A. Burlaka1, Natalya V. Sidorova2, Elena B. Machneva1,2, Tatyana V. Gorbunova1,5, Tatyana L. Ushakova1,3, Vladimir G. Polyakov1,3,4,5, Kirill I. Kirgizov1,5, Svetlana R. Varfolomeeva1,2,5
Clinical studies
Tahereh Rostami1, Mohammad R. Rostami2, Azadeh Kiumarsi1, Amir Kasaeian3, Neda Alijani4, Hosein K. Fumani2, Soroush Rad2, Davood Babakhani2, Tanaz Bahri2, Mohammad Vaezi2, Maryam Barkhordar2, Seied A. Mirhosseini2, Seied A. Mousavi2
Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina, Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin
Mohamed R. Abdelfattah, Hussein Elsiesy
Oleg I. Dolgov1, Sergey A. Karpishchenko1, Ekaterina S. Utimisheva1, Diana A. Grigoryanz1, Anna A. Spiridonova1,2, Ivan S. Moiseev1, Ludmila S. Zubarovskaya1, Alexei B. Chukhlovin1, Alexander D. Kulagin1
Clinical case
Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina, Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, Valery G. Savchenko
Experimental studies
Dima Joujeh1, Abduljalil Ghrewaty1, Chadi Soukkarieh2, Adnan Almarrawi1, Jamal Abdul Naser Darwicha3
Editorial
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28495
[VALUE] => Array
(
[TEXT] => <p>Профессор Александр Д. Кулагин, главный редактор журнала <i>«Клеточная Терапия и Трансплантация» (СТТ)</i></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Профессор Александр Д. Кулагин, главный редактор журнала «Клеточная Терапия и Трансплантация» (СТТ)
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28496
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением <sup>59</sup>Fe и других радиоактивных изотопов.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => В 2022 году Первый Санкт-Петербургский государственный медицинский университет им. И. П. Павлова отмечает свое 125-летие. Работы в области клинической гематологии и иммунологии развивались здесь с начала XX века на кафедре факультетской терапии. Заведующий кафедрой профессор Г. Ф. Ланг, ставший впоследствии выдающимся кардиологом, свою докторскую диссертацию (1901) посвятил изучению осмотической резистентности эритроцитов при раке желудка и других злокачественных новообразованиях, представил оригинальные экспериментальные исследования по регуляции клеток крови и гемолизу. Профессор Т. С. Истаманова, его преемница на этой кафедре, с 20-х гг. продолжала исследования в области физиологии и патологии эритропоэза, была одной из основоположников создания функциональной гематологии. Ее экспериментальные работы касались исследований роли селезенки в разрушении эритроцитов, нейрогенной регуляции кроветворения, функциональной роли ретикулоцитоза в процессе гемопоэза. Профессор Т. С. Истаманова глубоко изучала клинические аспекты полицитемии. Функциональная динамика эритроидных клеток широко изучалась в 40-х и 50-х годах, особенно с использованием передовых методов оценки метаболизма гемоглобина с применением 59Fe и других радиоактивных изотопов.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28497
[VALUE] => Array
(
[TEXT] => <p>Professor Alexander D. Kulagin, Editor-in-Chief, <i>Cellular Therapy and Transplantation Journal</i></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Professor Alexander D. Kulagin, Editor-in-Chief, Cellular Therapy and Transplantation Journal
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28498
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">
In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125<sup>th</sup> anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with <sup>59</sup>Fe and other radionuclides.
</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] =>
In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125th anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with 59Fe and other radionuclides.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28499
[VALUE] => Pavlov University: 125 years in blood research
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Pavlov University: 125 years in blood research
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28500
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">С 70-х годов кафедру возглавил проф. В. А. Алмазов.
С этого времени здесь началось изучение лейкогенеза и регуляции кроветворения новым поколением клинических гематологов во главе с Б. В. Афанасьевым. Культивирование колониеобразующих единиц клеток-предшественников грануло-моноцитопоэза позволили получить первые данные о внутренних факторах регуляции грануломоноцитопоэза при острых лейкозах, хроническом миелолейкозе, особенно при различных типах бластных кризов, миелодиспластическом синдроме у взрослых и, впервые – при апластической анемии у детей. Эти данные были обобщены в первой монографии в этой области «Родоначальные стволовые кроветворные клетки человека» (1985). </p>
<p style="text-align: justify;">Трагически известная Чернобыльская ядерная авария (1986 г.) способствовала развитию исследований в области острого цитостатического синдрома в СССР и за рубежом. Борис Владимирович Афанасьев, сотрудник 1-го Ленинградского медицинского института им. И. П. Павлова, был направлен в Сиэттл (США) для стажировки в знаменитую клинику Э. Доннела Томаса, в последующем лауреата Нобелевской премии 1990 г. за успешную трансплантацию гемопоэтических клеток в клинике. Через несколько лет, по инициативе профессора Б. В. Афанасьева, руководство Университета организовало отделение трансплантации костного мозга (1997 г.), где была начата программа по широкому внедрению различных видов трансплантации гемопоэтических стволовых клеток у детей и взрослых.</p>
<p style="text-align: justify;">Следует отметить обширную клиническую помощь и консультационные усилия наших зарубежных друзей и коллег в области принципов лечения лейкозов, иммунологического типирования, диагностики лейкозов и схем лечения. Эта поддержка была чрезвычайно важной в 1990-1996 гг., на ранних этапах нашей работы по трансплантации костного мозга. Отделения гематологии, онкологии и ТГСК университета не смогли бы добиться успеха в этой области без устойчивых профессиональных контактов с выдающимися специалистами из Европы и США. Прежде всего, следует отметить тесное сотрудничество с Университетскими клиниками Гамбурга и другими университетами Германии при непосредственном участии проф. Р. Нета, А. Цандера, Т. Бюхнера, других ведущих германских специалистов – Х. И. Кольба, Д. Хёльцера, Б. Фезе. В эту совместную работу были вовлечены и ведущие специалисты из других стран, например, проф. Р. Гэйл, (США), Г. Вагемакер (Нидерланды), А. Бачигалупо (Италия) и многие другие известные клиницисты. Проф. Аксель Цандер, Аксель Фаузер, Герард Вaгемaкер, Дитер Хёльцер были удостоены звания почетных докторов ПСПбГМУ им. И. П. Павлова за заслуги в сотрудничестве с российскими специалистами в этой области. </p>
<p style="text-align: justify;">В последние 15 лет развитие гематологии в Университете связано с организованным проф. Б. В. Афанасьевым НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, который входит в число крупнейших центров ТКМ в Европе. За этот период выполнено более 4500 аллогенных и аутологичных трансплантаций детям и взрослым с лейкозами, лимфомами, множественной миеломой, апластическими анемиями, солидными опухолями, иммунодефицитами заболеваниями и нарушениями обмена веществ. В Институте проводятся экспериментальные и клинические исследования в области лейкемий, миелопролиферативных заболеваний, лимфом, миеломы, костномозговой недостаточности и других областях гематологии.</p><p style="text-align: justify;">
Журнал «Клеточная терапия и трансплантация» (СТТ) –
совместный проект немецких и российских специалистов в области ТКМ и онкогематологии, издается с 2008 года. Журнал публикует оригинальные данные по трансплантации гемопоэтических стволовых клеток, иммунотерапии, клеточной и генной терапии, а также смежным вопросам медицины и биологии. Мы надеемся, что клиническая, исследовательская и издательская деятельность в этой области будет и дальше развиваться в Первом Санкт-Петербургском государственном медицинском университете им. И. П. Павлова в тесном сотрудничестве с нашими российскими и зарубежными коллегами на благо пациентов с лейкозами и другими тяжелыми заболеваниями, которые сейчас могут быть излечены с помощью современных терапевтических подходов. </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => С 70-х годов кафедру возглавил проф. В. А. Алмазов.
С этого времени здесь началось изучение лейкогенеза и регуляции кроветворения новым поколением клинических гематологов во главе с Б. В. Афанасьевым. Культивирование колониеобразующих единиц клеток-предшественников грануло-моноцитопоэза позволили получить первые данные о внутренних факторах регуляции грануломоноцитопоэза при острых лейкозах, хроническом миелолейкозе, особенно при различных типах бластных кризов, миелодиспластическом синдроме у взрослых и, впервые – при апластической анемии у детей. Эти данные были обобщены в первой монографии в этой области «Родоначальные стволовые кроветворные клетки человека» (1985).
Трагически известная Чернобыльская ядерная авария (1986 г.) способствовала развитию исследований в области острого цитостатического синдрома в СССР и за рубежом. Борис Владимирович Афанасьев, сотрудник 1-го Ленинградского медицинского института им. И. П. Павлова, был направлен в Сиэттл (США) для стажировки в знаменитую клинику Э. Доннела Томаса, в последующем лауреата Нобелевской премии 1990 г. за успешную трансплантацию гемопоэтических клеток в клинике. Через несколько лет, по инициативе профессора Б. В. Афанасьева, руководство Университета организовало отделение трансплантации костного мозга (1997 г.), где была начата программа по широкому внедрению различных видов трансплантации гемопоэтических стволовых клеток у детей и взрослых.
Следует отметить обширную клиническую помощь и консультационные усилия наших зарубежных друзей и коллег в области принципов лечения лейкозов, иммунологического типирования, диагностики лейкозов и схем лечения. Эта поддержка была чрезвычайно важной в 1990-1996 гг., на ранних этапах нашей работы по трансплантации костного мозга. Отделения гематологии, онкологии и ТГСК университета не смогли бы добиться успеха в этой области без устойчивых профессиональных контактов с выдающимися специалистами из Европы и США. Прежде всего, следует отметить тесное сотрудничество с Университетскими клиниками Гамбурга и другими университетами Германии при непосредственном участии проф. Р. Нета, А. Цандера, Т. Бюхнера, других ведущих германских специалистов – Х. И. Кольба, Д. Хёльцера, Б. Фезе. В эту совместную работу были вовлечены и ведущие специалисты из других стран, например, проф. Р. Гэйл, (США), Г. Вагемакер (Нидерланды), А. Бачигалупо (Италия) и многие другие известные клиницисты. Проф. Аксель Цандер, Аксель Фаузер, Герард Вaгемaкер, Дитер Хёльцер были удостоены звания почетных докторов ПСПбГМУ им. И. П. Павлова за заслуги в сотрудничестве с российскими специалистами в этой области.
В последние 15 лет развитие гематологии в Университете связано с организованным проф. Б. В. Афанасьевым НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, который входит в число крупнейших центров ТКМ в Европе. За этот период выполнено более 4500 аллогенных и аутологичных трансплантаций детям и взрослым с лейкозами, лимфомами, множественной миеломой, апластическими анемиями, солидными опухолями, иммунодефицитами заболеваниями и нарушениями обмена веществ. В Институте проводятся экспериментальные и клинические исследования в области лейкемий, миелопролиферативных заболеваний, лимфом, миеломы, костномозговой недостаточности и других областях гематологии.
Журнал «Клеточная терапия и трансплантация» (СТТ) –
совместный проект немецких и российских специалистов в области ТКМ и онкогематологии, издается с 2008 года. Журнал публикует оригинальные данные по трансплантации гемопоэтических стволовых клеток, иммунотерапии, клеточной и генной терапии, а также смежным вопросам медицины и биологии. Мы надеемся, что клиническая, исследовательская и издательская деятельность в этой области будет и дальше развиваться в Первом Санкт-Петербургском государственном медицинском университете им. И. П. Павлова в тесном сотрудничестве с нашими российскими и зарубежными коллегами на благо пациентов с лейкозами и другими тяжелыми заболеваниями, которые сейчас могут быть излечены с помощью современных терапевтических подходов.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28501
[VALUE] => 2759
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2759
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28502
[VALUE] => 2760
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2760
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Professor Alexander D. Kulagin, Editor-in-Chief, Cellular Therapy and Transplantation Journal
In 2022, the First St. Petersburg State Medical University (Pavlov University) is celebrating its 125th anniversary. The studies in clinical hematology and immunology developed here since early XX century at the Chair of Faculty Therapy. Its future head, Prof. Georg F. Lang later became a famous cardiologist. However, his Doctor’s Thesis (1901) was dedicated to osmotic resistance of red blood cells in stomach cancer and other malignancies. He presented original experimental studies on regulation of red blood cells and hemolysis. Later on, professor T. S. Istamanova headed the chair, being the best successor of his school. She was among founders of functional hematology, proceeded with studies in physiology and pathology of erythropoiesis performed since 20s. Her experimental works concerned the role of spleen in red blood cell destruction, neurogenic regulation of hematopoiesis, functional significance of reticulocytosis in hematopoietic function. Prof. T. S. Istamanova was deeply involved into clinical aspects of polycythemia. Functional dynamics of erythroid cells was extensively studied over 40s and 50s, especially, using innovative assays of hemoglobin metabolism with 59Fe and other radionuclides.
Review articles
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28503
[VALUE] => 01/15/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 01/15/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28504
[VALUE] => 02/18/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 02/18/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28505
[VALUE] => Array
(
[TEXT] => <p>Карина А. Сергеенко<sup>1,3</sup>, Яна Ю. Докучаева<sup>1</sup>, Ирина О. Костарева<sup>1</sup>, Тим З. Алиев<sup>1</sup>, Анна Ю. Елфимова<sup>1</sup>,
Николай Г. Степанян<sup>1</sup>, Юрий В. Лозован<sup>1</sup>, Наталья А. Бурлака<sup>1</sup>, Наталья В. Сидорова<sup>2</sup>, Елена Б. Мачнева<sup>1,2</sup>,
Татьяна В. Горбунова<sup>1,5</sup>, Татьяна Л. Ушакова<sup>1,3</sup>, Владимир Г. Поляков<sup>1,3,4,5</sup>, Кирилл И. Киргизов<sup>1,5</sup>,
Светлана Р. Варфоломеева<sup>1,2,5</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Карина А. Сергеенко1,3, Яна Ю. Докучаева1, Ирина О. Костарева1, Тим З. Алиев1, Анна Ю. Елфимова1,
Николай Г. Степанян1, Юрий В. Лозован1, Наталья А. Бурлака1, Наталья В. Сидорова2, Елена Б. Мачнева1,2,
Татьяна В. Горбунова1,5, Татьяна Л. Ушакова1,3, Владимир Г. Поляков1,3,4,5, Кирилл И. Киргизов1,5,
Светлана Р. Варфоломеева1,2,5
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28506
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> ФГБУ «Национальный медицинский исследовательский центр онкологии им. Н. Н. Блохина» Минздрава России, Москва, Россия<br>
<sup>2</sup> Обособленное структурное подразделение Российская детская клиническая больница ФГАОУ ВО
«РНИМУ им. Н. И. Пирогова» Минздрава России, Москва, Россия<br>
<sup>3</sup> ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования», Москва, Россия<br>
<sup>4</sup> ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н. И. Пирогова» Минздрава России, Москва, Россия<br>
<sup>5</sup> Кафедра последипломного образования врачей НМИЦ онкологии им. Н. Н. Блохина, Москва, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 ФГБУ «Национальный медицинский исследовательский центр онкологии им. Н. Н. Блохина» Минздрава России, Москва, Россия
2 Обособленное структурное подразделение Российская детская клиническая больница ФГАОУ ВО
«РНИМУ им. Н. И. Пирогова» Минздрава России, Москва, Россия
3 ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования», Москва, Россия
4 ФГАОУ ВО «Российский национальный исследовательский медицинский университет им. Н. И. Пирогова» Минздрава России, Москва, Россия
5 Кафедра последипломного образования врачей НМИЦ онкологии им. Н. Н. Блохина, Москва, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28507
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Ретинобластома (РБ) – самое частое злокачественное новообразование (ЗНО) органа зрения у детей, составляет 10-15% от всех ЗНО детей первого года жизни. Несмотря на наличие стандартных подходов к лечению детей с РБ, в ряде случаев стандартные методы могут оказаться неэффективными, что требует поиска новых стратегий для улучшения выживаемости у детей группы высокого риска. В качестве интенсификации может использоваться высокодозная химиотерапия с последующей аутологичной трансплантацией гемопоэтических стволовых клеток (ауто-ТГСК). Цель нашей работы – демонстрация опыта НМИЦ онкологии им. Н. Н. Блохина на примере случаев ауто-ТГСК у пациентов с РБ.</p>
<h3>Материалы и методы</h3>
<p style="text-align: justify;">В 2021 г. в НИИ детской онкологии и гематологии НМИЦ онкологии им. Н. Н. Блохина 3 пациента с РБ высокой группы риска получили в режиме кондиционирования: Карбоплатин 1250 мг/кв.м., Этопозид 1750 мг/кв.м., Циклофосфамид 6 гр/кв.м. с последующей ауто-ТГСК.</p>
<h3>Результаты</h3>
<p style="text-align: justify;">Восстановление гемопоэза произошло на 11, 14 и 17 сутки после ауто-ТГСК. Осложнения раннего посттрансплантационного периода: орофарингеальный мукозит, нейтропенический энтероколит, фебрильная нейтропения. В периоде кондиционирования у одного пациента зафискирован эпизод тонико-клонических судорог на фоне гипонатриемии, эпизод купирован, более не повторялся. У одного пациента констатирована прогрессия заболевания, что привело к летальному исходу. Два пациента – без признаков рецидива. Медиана наблюдения 6 ( 4-10) месяцев.</p>
<h3>Выводы</h3>
<p style="text-align: justify;">Ауто-ТГСК для пациентов с РБ группы высокого риска может рассматриваться как консолидация, в виду хорошей переносимости и эффективности. Требуется включение в исследование большего числа пациентов, длительное наблюдение, а также обмен опытом между трансплантационными центрами.</p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Аутологичная трансплантация гемопоэтических стволовых клеток, ретинобластома, дети, высокодозная химиотерапия.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Ретинобластома (РБ) – самое частое злокачественное новообразование (ЗНО) органа зрения у детей, составляет 10-15% от всех ЗНО детей первого года жизни. Несмотря на наличие стандартных подходов к лечению детей с РБ, в ряде случаев стандартные методы могут оказаться неэффективными, что требует поиска новых стратегий для улучшения выживаемости у детей группы высокого риска. В качестве интенсификации может использоваться высокодозная химиотерапия с последующей аутологичной трансплантацией гемопоэтических стволовых клеток (ауто-ТГСК). Цель нашей работы – демонстрация опыта НМИЦ онкологии им. Н. Н. Блохина на примере случаев ауто-ТГСК у пациентов с РБ.
Материалы и методы
В 2021 г. в НИИ детской онкологии и гематологии НМИЦ онкологии им. Н. Н. Блохина 3 пациента с РБ высокой группы риска получили в режиме кондиционирования: Карбоплатин 1250 мг/кв.м., Этопозид 1750 мг/кв.м., Циклофосфамид 6 гр/кв.м. с последующей ауто-ТГСК.
Результаты
Восстановление гемопоэза произошло на 11, 14 и 17 сутки после ауто-ТГСК. Осложнения раннего посттрансплантационного периода: орофарингеальный мукозит, нейтропенический энтероколит, фебрильная нейтропения. В периоде кондиционирования у одного пациента зафискирован эпизод тонико-клонических судорог на фоне гипонатриемии, эпизод купирован, более не повторялся. У одного пациента констатирована прогрессия заболевания, что привело к летальному исходу. Два пациента – без признаков рецидива. Медиана наблюдения 6 ( 4-10) месяцев.
Выводы
Ауто-ТГСК для пациентов с РБ группы высокого риска может рассматриваться как консолидация, в виду хорошей переносимости и эффективности. Требуется включение в исследование большего числа пациентов, длительное наблюдение, а также обмен опытом между трансплантационными центрами.
Ключевые слова
Аутологичная трансплантация гемопоэтических стволовых клеток, ретинобластома, дети, высокодозная химиотерапия.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28508
[VALUE] => 10.18620/ctt-1866-8836-2022-11-1-6-12
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2022-11-1-6-12
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28511
[VALUE] => Array
(
[TEXT] => <p>Karina A. Sergeenko<sup>1,3</sup>, Yana Yu. Dokuchaeva<sup>1</sup>, Irina O. Kostareva<sup>1</sup>, Tim Z. Aliev<sup>1</sup>, Anna Yu. Elfimova<sup>1</sup>,
Nikolay G. Stepanian<sup>1</sup>, Yury V. Lozovan<sup>1</sup>, Natalya A. Burlaka<sup>1</sup>, Natalya V. Sidorova<sup>2</sup>, Elena B. Machneva<sup>1,2</sup>,
Tatyana V. Gorbunova<sup>1,5</sup>, Tatyana L. Ushakova<sup>1,3</sup>, Vladimir G. Polyakov<sup>1,3,4,5</sup>, Kirill I. Kirgizov<sup>1,5</sup>,
Svetlana R. Varfolomeeva<sup>1,2,5</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Karina A. Sergeenko1,3, Yana Yu. Dokuchaeva1, Irina O. Kostareva1, Tim Z. Aliev1, Anna Yu. Elfimova1,
Nikolay G. Stepanian1, Yury V. Lozovan1, Natalya A. Burlaka1, Natalya V. Sidorova2, Elena B. Machneva1,2,
Tatyana V. Gorbunova1,5, Tatyana L. Ushakova1,3, Vladimir G. Polyakov1,3,4,5, Kirill I. Kirgizov1,5,
Svetlana R. Varfolomeeva1,2,5
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28512
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia<br>
<sup>2</sup> Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia<br>
<sup>3</sup> Russian Medical Academy for Continuous Professional Education, Moscow, Russia <br>
<sup>4</sup> N. I. Pirogov Russian National Medical University, Moscow, Russia <br>
<sup>5</sup> Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia</p><br>
<p><b>Correspondence:</b><br>
Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia<br>
E-mail: karina_s19@mail.ru</p><br>
<p><b>Citation:</b> Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
2 Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia
3 Russian Medical Academy for Continuous Professional Education, Moscow, Russia
4 N. I. Pirogov Russian National Medical University, Moscow, Russia
5 Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
Correspondence:
Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia
E-mail: karina_s19@mail.ru
Citation: Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28513
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.</p>
<h3>Materials and methods</h3>
<p style="text-align: justify;">In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m<sup>2</sup>), etoposide (1750 mg/m<sup>2</sup>), and cyclophosphamide (6000 mg/m<sup>2</sup>) with subsequent auto-HSCT. </p>
<h3>Results</h3>
<p style="text-align: justify;">All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was
complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.</p>
<h3>Conclusions</h3>
<p style="text-align: justify;">The high-dose consolidation with subsequent auto-
HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.</p>
<h2>Keywords</h2>
<p style="text-align: justify;">Autologous hematopoietic stem cell transplantation,
retinoblastoma, children, high-dose chemotherapy.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.
Materials and methods
In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m2), etoposide (1750 mg/m2), and cyclophosphamide (6000 mg/m2) with subsequent auto-HSCT.
Results
All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was
complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.
Conclusions
The high-dose consolidation with subsequent auto-
HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.
Keywords
Autologous hematopoietic stem cell transplantation,
retinoblastoma, children, high-dose chemotherapy.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28509
[VALUE] => High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28510
[VALUE] => 2761
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2761
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28514
[VALUE] => 2764
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2764
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Karina A. Sergeenko1,3, Yana Yu. Dokuchaeva1, Irina O. Kostareva1, Tim Z. Aliev1, Anna Yu. Elfimova1, Nikolay G. Stepanian1, Yury V. Lozovan1, Natalya A. Burlaka1, Natalya V. Sidorova2, Elena B. Machneva1,2, Tatyana V. Gorbunova1,5, Tatyana L. Ushakova1,3, Vladimir G. Polyakov1,3,4,5, Kirill I. Kirgizov1,5, Svetlana R. Varfolomeeva1,2,5
1 N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
2 Russian State Clinical Hospital, N. I. Pirogov Russian National Research Medical University, Moscow Russia
3 Russian Medical Academy for Continuous Professional Education, Moscow, Russia
4 N. I. Pirogov Russian National Medical University, Moscow, Russia
5 Department of Continious Medical Education, N. N. Blokhin National Medical Research Center of Oncology, Moscow, Russia
Correspondence:
Dr. Karina A. Sergeenko, Resident, Department of Pediatric Oncology, Russian Medical Academy for Continuous Professional Education, Moscow, Russia
E-mail: karina_s19@mail.ru
Citation: Sergeenko KA, Dokuchaeva YaYu, Kostareva IO et al. High-dose chemotherapy with autologous hemopoietic stem cell transplantation in children with retinoblastoma. Literature review and case series. Cell Ther Transplant 2022; 11(1): 6-12.
Retinoblastoma (RB) is the most common malignant eye tumor in children accounting for 10-15% of all cancer cases in infants. In spite of generally good standard treatment results there is still a subgroup of high-risk patients with by unfavorable prognosis, which warrants the search for additional treatment strategies. These children may benefit from treatment intensification in form of high-dose consolidation with subsequent autologous hemopoietic stem cell therapy (auto-HSCT). We here describe a case series illustrating N. N. Blokhin Cancer Center experience in this area.
Materials and methods
In 2021 a total of 3 children with high-risk RB were treated in N. N. Blokhin Cancer Center receiving high-dose regimen consisting of carboplatin (total dose of 1250 mg/m2), etoposide (1750 mg/m2), and cyclophosphamide (6000 mg/m2) with subsequent auto-HSCT.
Results
All 3 patients engrafted in day +11, +14, and +17 after auto-HSCT. The early post-transplant period was complicated by oral mucositis, neutropenic enterocolitis, and febrile neutropenia. One patient had a single episode of seizures due to hyponatremia. With a median follow-up of 6 (4-10) months two patients are alive and disease-free, one died due to disease progression.
Conclusions
The high-dose consolidation with subsequent auto- HSCT is a feasible option for high-risk RB patients. It is characterized by acceptable toxicity and is a potentially effective for disease control. In order to further evaluate the long-term results, there is a need for a larger prospective patient cohort. The multicenter study design may be beneficial in these settings.
Keywords
Autologous hematopoietic stem cell transplantation, retinoblastoma, children, high-dose chemotherapy.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28530
[VALUE] => 01/24/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 01/24/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28531
[VALUE] => 02/18/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 02/18/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28532
[VALUE] => Array
(
[TEXT] => <p>Тахерех Ростами<sup>1</sup>, Мохамад Р. Ростами<sup>2</sup>, Азадех Кьюмарси<sup>1</sup>, Амир Казаэйян<sup>3</sup>, Неда Алиджани<sup>4</sup>,
Хосейн К. Фумани<sup>2</sup>, Соруш Рад<sup>2</sup>, Давуд Бабахани<sup>2</sup>, Таназ Бахри<sup>2</sup>, Мохаммад Ваези<sup>2</sup>, Мариам Бахордар<sup>2</sup>,
Сейед А. Мирхоссейни<sup>2</sup>, Сейед А. Моусави<sup>2</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Тахерех Ростами1, Мохамад Р. Ростами2, Азадех Кьюмарси1, Амир Казаэйян3, Неда Алиджани4,
Хосейн К. Фумани2, Соруш Рад2, Давуд Бабахани2, Таназ Бахри2, Мохаммад Ваези2, Мариам Бахордар2,
Сейед А. Мирхоссейни2, Сейед А. Моусави2
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28533
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Отдел клеточной терапии у детей, НИИ онкологии, гематологии и клеточной терапии (RIOHCT), Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br>
<sup>2</sup> НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br>
<sup>3</sup> Отдел биостатистики и эпидемиологии, НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран<br>
<sup>4</sup> Отдел инфекционных болезней, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Отдел клеточной терапии у детей, НИИ онкологии, гематологии и клеточной терапии (RIOHCT), Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
2 НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
3 Отдел биостатистики и эпидемиологии, НИИ онкологии, гематологии и клеточной терапии, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
4 Отдел инфекционных болезней, Шариатский госпиталь, Тегеранский университет медицинских наук (TUMS), Тегеран, Иран
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28534
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Трансплантация аллогенных гематопоэтических клеток (алло-ТГСК) является единственной потенциальной возможностью излечения острого лейкоза. Многие параметры существенно влияют на конечный исход ТГСК, в т.ч. тип донора, источник стволовых клеток и применяемый режим кондиционирования. При отсутствии HLA-совместимого родственного донора, возможными кандидатами могут быть неродственные совместимые или гаплоидентичные доноры для пациентов с показаниями к ТГСК. Для того, чтобы сопоставить исходы ТГСК от доноров различного типа с кондиционированием без облучения, мы сравнили в рамках одноцентрового исследования результаты трансплантации интактных ГСК периферической крови от совместимых и несовместимых, родственных и неродственных доноров, и гаплоидентичных доноров реципиентам детского, подросткового возрастов и молодым взрослым с острыми лейкозами.</p>
<h3>Пациенты и методы</h3>
<p style="text-align: justify;">В данном ретроспективном исследовании, проводившемся с 2014 по 2021 г., мы оценивали исходы ТГСК с реплецией Т-лимфоцитов от гаплоидентичных
доноров или неродственных доноров (совместимость – 10/10 или 9/10), а также в сравнении с неродственными донорами у пациентов с острыми лейкозами этих возрастных групп. Кондиционирование при ТГСК проводили с применением миелоаблативного режима с бусульфаном и циклофосфамидом и без ионизирующего облучения. Профилактика РТПХ включала назначение циклоспорина А всем пациентам, кроличий антитимоцитарный глобулин для неродственных и гаплоидентичных доноров, и циклофосфамид при ТГСК от гаплоидентичных доноров. Статистическую обработку проводили с помощью многовариантного пропорционального анализа рисков по Коксу и анализ конкурирующих рисков.</p>
<h3>Результаты</h3>
<p style="text-align: justify;">Средний срок наблюдения составлял 28,7 мес. (95% CI: 21,9-34,9). Трехлетняя общая выживаемость (ОВ) и выживаемости без РТПХ и рецидивов были, соответственно, 68,81% (95% CI: 60,08%-76,01%) и 44.19% (95% CI: 35,52%-52,49%). Пациенты после ТГСК от неродственных совместимых доноров имели более низкие уровни ОВ и выживаемости без РТПХ и рецидивов по сравнению с другими типами доноров. Трехлетние показатели безрецидивной летальности (NRM) среди всех пациентов составляли 7,84% (95% CI 4,36-12,62). Адаптированное многовариантное моделирование общей выживаемости показало, что риск гибели пациентов после ТГСК от неродственного донора был в 3,6 раза выше, чем у пациентов, получивших ТГСК от гаплоидентичных доноров (P=0.05). Аналогично, риск безрецидивной смертности (NRM) после ТГСК от неродственных доноров был в 6 раз выше, чем при ТГСК от гаплоидентичных доноров (P=0.002). Однако частота рецидивов не различалась существенно между двумя указанными группами.</p>
<h3>Выводы</h3>
<p style="text-align: justify;">В данном исследовании показано, что ТГСК от гаплоидентичных доноров была ассоциирована с более высокими уровнями выживаемости, по сравнению с ТГСК от неродственных совместимых доноров. Таким образом, ТГСК от гаплоидентичных доноров может быть предложена в качестве практичной и ценной клинической опции, для пациентов молодых возрастов с острыми лейкозами в случае отсутствия совместимых доноров.</p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Острый лейкоз, аллогенная трансплантация гемопоэтических клеток, совместимые родственные доноры, неродственные доноры, гаплоидентичные доноры, клинические исходы.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Трансплантация аллогенных гематопоэтических клеток (алло-ТГСК) является единственной потенциальной возможностью излечения острого лейкоза. Многие параметры существенно влияют на конечный исход ТГСК, в т.ч. тип донора, источник стволовых клеток и применяемый режим кондиционирования. При отсутствии HLA-совместимого родственного донора, возможными кандидатами могут быть неродственные совместимые или гаплоидентичные доноры для пациентов с показаниями к ТГСК. Для того, чтобы сопоставить исходы ТГСК от доноров различного типа с кондиционированием без облучения, мы сравнили в рамках одноцентрового исследования результаты трансплантации интактных ГСК периферической крови от совместимых и несовместимых, родственных и неродственных доноров, и гаплоидентичных доноров реципиентам детского, подросткового возрастов и молодым взрослым с острыми лейкозами.
Пациенты и методы
В данном ретроспективном исследовании, проводившемся с 2014 по 2021 г., мы оценивали исходы ТГСК с реплецией Т-лимфоцитов от гаплоидентичных
доноров или неродственных доноров (совместимость – 10/10 или 9/10), а также в сравнении с неродственными донорами у пациентов с острыми лейкозами этих возрастных групп. Кондиционирование при ТГСК проводили с применением миелоаблативного режима с бусульфаном и циклофосфамидом и без ионизирующего облучения. Профилактика РТПХ включала назначение циклоспорина А всем пациентам, кроличий антитимоцитарный глобулин для неродственных и гаплоидентичных доноров, и циклофосфамид при ТГСК от гаплоидентичных доноров. Статистическую обработку проводили с помощью многовариантного пропорционального анализа рисков по Коксу и анализ конкурирующих рисков.
Результаты
Средний срок наблюдения составлял 28,7 мес. (95% CI: 21,9-34,9). Трехлетняя общая выживаемость (ОВ) и выживаемости без РТПХ и рецидивов были, соответственно, 68,81% (95% CI: 60,08%-76,01%) и 44.19% (95% CI: 35,52%-52,49%). Пациенты после ТГСК от неродственных совместимых доноров имели более низкие уровни ОВ и выживаемости без РТПХ и рецидивов по сравнению с другими типами доноров. Трехлетние показатели безрецидивной летальности (NRM) среди всех пациентов составляли 7,84% (95% CI 4,36-12,62). Адаптированное многовариантное моделирование общей выживаемости показало, что риск гибели пациентов после ТГСК от неродственного донора был в 3,6 раза выше, чем у пациентов, получивших ТГСК от гаплоидентичных доноров (P=0.05). Аналогично, риск безрецидивной смертности (NRM) после ТГСК от неродственных доноров был в 6 раз выше, чем при ТГСК от гаплоидентичных доноров (P=0.002). Однако частота рецидивов не различалась существенно между двумя указанными группами.
Выводы
В данном исследовании показано, что ТГСК от гаплоидентичных доноров была ассоциирована с более высокими уровнями выживаемости, по сравнению с ТГСК от неродственных совместимых доноров. Таким образом, ТГСК от гаплоидентичных доноров может быть предложена в качестве практичной и ценной клинической опции, для пациентов молодых возрастов с острыми лейкозами в случае отсутствия совместимых доноров.
Ключевые слова
Острый лейкоз, аллогенная трансплантация гемопоэтических клеток, совместимые родственные доноры, неродственные доноры, гаплоидентичные доноры, клинические исходы.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28535
[VALUE] => 10.18620/ctt-1866-8836-2022-11-1-24-35
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2022-11-1-24-35
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28538
[VALUE] => Array
(
[TEXT] => <p>Tahereh Rostami<sup>1</sup>, Mohammad R. Rostami<sup>2</sup>, Azadeh Kiumarsi<sup>1</sup>, Amir Kasaeian<sup>3</sup>, Neda Alijani<sup>4</sup>, Hosein K. Fumani<sup>2</sup>, Soroush Rad<sup>2</sup>, Davood Babakhani<sup>2</sup>, Tanaz Bahri<sup>2</sup>, Mohammad Vaezi<sup>2</sup>, Maryam Barkhordar<sup>2</sup>, Seied A. Mirhosseini<sup>2</sup>, Seied A. Mousavi<sup>2</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Tahereh Rostami1, Mohammad R. Rostami2, Azadeh Kiumarsi1, Amir Kasaeian3, Neda Alijani4, Hosein K. Fumani2, Soroush Rad2, Davood Babakhani2, Tanaz Bahri2, Mohammad Vaezi2, Maryam Barkhordar2, Seied A. Mirhosseini2, Seied A. Mousavi2
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28539
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br>
<sup>2</sup> Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br>
<sup>3</sup> Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati
Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran<br>
<sup>4</sup> Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran</p><br>
<p><b>Correspondence:</b><br>
Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran<br>
Phone: +98 9121037104<br>
Fax: +98 (21) 8802 9397<br>
Email: akiumarsi@sina.tums.ac.ir</p><br>
<p><b>Citation:</b> Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35. </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
2 Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3 Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati
Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
4 Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
Correspondence:
Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran
Phone: +98 9121037104
Fax: +98 (21) 8802 9397
Email: akiumarsi@sina.tums.ac.ir
Citation: Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28540
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.</p>
<h3>Patients and methods</h3>
<p style="text-align: justify;">In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors <i>versus</i> unrelated donors (including 10/10 or 9/10 HLA-matched), and <i>versus</i> related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.</p>
<h3>Results</h3>
<p style="text-align: justify;">Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.</p>
<h3>Conclusions</h3>
<p style="text-align: justify;">In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.</p>
<h2>Keywords</h2>
<p style="text-align: justify;">Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.
Patients and methods
In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors versus unrelated donors (including 10/10 or 9/10 HLA-matched), and versus related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.
Results
Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.
Conclusions
In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.
Keywords
Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28536
[VALUE] => Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28537
[VALUE] => 2786
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2786
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28541
[VALUE] => 2787
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2787
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Tahereh Rostami1, Mohammad R. Rostami2, Azadeh Kiumarsi1, Amir Kasaeian3, Neda Alijani4, Hosein K. Fumani2, Soroush Rad2, Davood Babakhani2, Tanaz Bahri2, Mohammad Vaezi2, Maryam Barkhordar2, Seied A. Mirhosseini2, Seied A. Mousavi2
1 Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
2 Research Institute for Oncology, Hematology and Cell Therapy (RIOHCT), Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
3 Department of Biostatistics and Epidemiology, Research Institute for Oncology, Hematology and Cell Therapy, Shariati
Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
4 Department of lnfectious Diseases, Shariati Hospital, Tehran University of Medical Sciences (TUMS), Tehran, Iran
Correspondence:
Dr. Azadeh Kiumarsi, MD, Assistant Professor, Pediatric Hematology, Oncology and Stem Cell Transplantation, Department of Pediatric Cell Therapy, Research Institute for Oncology, Hematology and Cell Therapy, Shariati Hospital, Kargar Shomali Street, 1411713131, Tehran, Iran
Phone: +98 9121037104
Fax: +98 (21) 8802 9397
Email: akiumarsi@sina.tums.ac.ir
Citation: Tahereh Rostami, Mohammad R. Rostami, Azadeh Kiumarsi et al. Peripheral blood stem cell transplantation from haploidentical and unrelated versus related donors for acute leukemia in children, adolescents and young adults (CAYA): A competing risk analysis. Cell Ther Transplant 2022; 11(1): 24-35.
Allogeneic hematopoietic stem cell transplantation (HSCT) is the only potentially curative treatment for acute leukemia. Various parameters have significant impact on the final results of HSCT, such as donor type, stem cell source, and the applied conditioning regimen. In the absence of HLA-matched related or unrelated donors, haploidentical donors present a possible alternative for the patients with indications for HSCT. The present single-center study compared the outcomes of HSCT from different donor types using a radiation-free MAC regimen. We compared the results of unmanipulated peripheral blood stem cell transplantation (PBSCT) from matched, or mismatched related, and unrelated donors with those from haploidentical donors in the children, adolescents and young adults (CAYA) treated for acute leukemia.
Patients and methods
In this retrospective study performed since 2014 to 2021, we have evaluated the clinical outcomes among CAYA patients with acute leukemia who underwent peripheral blood T cell-replete HSCT from haploidentical donors versus unrelated donors (including 10/10 or 9/10 HLA-matched), and versus related donors (including 10/10 or 9/10 HLA-matched). The myeloablative conditioning for HSCT was performed as irradiation-free regimen including busulfan and cyclophosphamide. GvHD prophylaxis was based on administration of cyclosporine A in all the patients, accomplished by rabbit anti-human thymocyte globulin in HSCT from unrelated and haploidentical donors, and post-transplant cyclophosphamide in cases of haploidentical donors. For statistical evaluation, an adjusted multivariable proportional hazard Cox and competing risk analyses were used.
Results
Median follow-up time period was 28.7 months (95% CI: 21.9-34.9). Three-year overall survival rate (OS) and GvHD-free/relapse-free survival (GFRFS) rate were 68.81% (95% CI: 60.08%-76.01%) and 44.19% (95% CI: 35.52%-52.49%), respectively. The patients who underwent HSCT from unrelated HLA-matched donors had the lowest OS and GFRFS compared to other donor types. The 3-year non-relapse mortality (NRM) in all patients was 7.84% (95% CI 4.36-12.62). Adjusted multivariable modeling of OS showed that the hazard of death in patients who had undergone HSCT from an unrelated donor, was 3.6 times more than for the patients who underwent HSCT from their haploidentical donors (P=0.05). Likewise, the hazard of NRM after HSCT from unrelated donors was 6 times more than with haploidentical donors (P=0.002). However, the relapse incidence was not significantly different between the two mentioned groups.
Conclusions
In this study, HSCT from haploidentical donors was associated with superior survival rates compared to HSCT from unrelated HLA-matched donors. Hence, haploidentical transplantation with peripheral blood stem cells could be a practical and valuable clinical option that offers a reasonable opportunity for the disease control in CAYA patients with acute leukemia requiring HSCT and lacking matched available donors.
Keywords
Acute leukemia, allogeneic hematopoietic stem cell transplantation, matched related donors, unrelated donors, haploidentical donors, clinical outcomes.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28521
[VALUE] => 03/09/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 03/09/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28522
[VALUE] => 03/18/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 03/18/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28523
[VALUE] => Array
(
[TEXT] => <p>Елена В. Морозова, Татьяна А. Рудакова, Юлия Ю. Власова, Мария В. Барабанщикова, Татьяна Л. Гиндина,
Александр Л. Алянский, Мария Д. Владовская, Иван С. Моисеев, Людмила С. Зубаровская, Александр Д. Кулагин</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Елена В. Морозова, Татьяна А. Рудакова, Юлия Ю. Власова, Мария В. Барабанщикова, Татьяна Л. Гиндина,
Александр Л. Алянский, Мария Д. Владовская, Иван С. Моисеев, Людмила С. Зубаровская, Александр Д. Кулагин
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28524
[VALUE] => Array
(
[TEXT] => <p>НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => НИИ детской онкологии, гематологии и трансплантологии им. Р. М. Горбачевой, Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28525
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.</p>
<h3>Пациенты и методы</h3>
<p style="text-align: justify;">Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев. </p>
<h3>Результаты</h3>
<p style="text-align: justify;">Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.</p>
<h3>Выводы</h3>
<p style="text-align: justify;">Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.</p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Аллогенная трансплантация стволовых клеток (алло-ТГСК) используется во всем мире для долгосрочного контроля и лечения злокачественных новообразований системы крови, по-прежнему оставаясь методом выбора в лечении хронического миелоидного лейкоза (ХМЛ) у пациентов, которые не могут достичь длительного полного цитогенетического ответа после лечения ингибиторами тирозинкиназы (ИТК), а также на поздних стадиях заболевания. Наряду с риском рецидива, неблагоприятные результаты ТГСК могут быть связаны с первичной недостаточностью (ПНТ) или плохой функцией трансплантата (ПФТ). Следовательно, целью нашего исследования было оценить частоту и исход ПНТ и тяжелой плохой функции трансплантата (ПФТ) после алло-ТГСК у пациентов с ХМЛ.
Пациенты и методы
Мы провели ретроспективный анализ 121 случая ХМЛ, которым проводилась алло-ТГСК в НИИ им. Р. М. Горбачевой ПСПбГМУ им. И. Павлова за последние 25 лет. ТГСК была показана в случаях продвинутой фазы заболевания или резистентности/непереносимости ИТК у пациентов с ХМЛ. Уровни транскриптов BCR/ABL и дополнительные хромосомные аномалии использовались в качестве лабораторных маркеров персистирующего заболевания. 80 пациентам (66%) трансплантацию проводили в хронической фазе заболевания (ХФ); 41 пациент (34%) находился в фазе акселерации (ФА) или бластном кризе (БК) на момент ТГСК. Трансплантацию от совместимых неродственных доноров выполняли в 65% случаев; от совместимых родственных доноров – в 28%, и от гаплоидентичных доноров – в 7% случаев.
Результаты
Приживление трансплантата отмечено у 106 пациентов (88%). Посттрансплантационные рецидивы зарегистрированы у 31 пациента в сроки от 15 до 333 дней после ТГСК. ПНТ была зарегистрирована в 8 случаях (7%). У двух пациентов развилась вторичная недостаточность трансплантата в течение двух месяцев после первичного приживления с летальными инфекционными осложнениями. Тяжелое нарушение функции трансплантата (ПФТ) диагностировано в 11 случаях (9%), при кумулятивной частоте 10% в течение 1-го года после трансплантации. Среди различных предтрансплантационных характеристик, фактор возраста и, особенно – наличие дополнительных хромосомных аномалий (ДХА) были связаны с кумулятивной частотой первичной и тяжелой вторичной недостаточности трансплантата после ТГСК. Т.е. ПНТ составил 14% в группе с выявленными ДХА по сравнению с 3% в группе без ДХА, (p=0,02), тогда как частота вторичной недостаточности трансплантата у пациентов с ДХА составила 2% против 12% в группе без АЦА (p=0,09). Частота посттрансплантационных рецидивов у пациентов с ПНТ и ПФТ не различалась.
Выводы
Первичная недостаточность трансплантата (ПНТ) способствует безрецидивной смертности в течение первого года после алло-ТГСК у пациентов с ХМЛ. Возникновение посттрансплантационных рецидивов не было связано с ПНТ И ПФТ при ХМЛ. Для улучшения эффективности технологий ТГСК необходима дальнейшая оценка факторов риска несостоятельности или плохой функции трансплантата.
Ключевые слова
Хронический миелоидный лейкоз, трансплантация гемопоэтических стволовых клеток, показания, несостоятельность трансплантата, факторы риска.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28518
[VALUE] => 10.18620/ctt-1866-8836-2022-11-1-13-23
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2022-11-1-13-23
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28526
[VALUE] => Array
(
[TEXT] => <p>Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina,
Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina,
Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28527
[VALUE] => Array
(
[TEXT] => <p>RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia</p><br>
<p><b>Correspondence:</b><br>
Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia<br>
Phone: +7 (911) 927-82-29<br>
E-mail: dr_morozova@mail.ru</p><br>
<p><b>Citation:</b> Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia
Correspondence:
Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (911) 927-82-29
E-mail: dr_morozova@mail.ru
Citation: Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28528
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">
Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
</p>
<h3>Patients and methods</h3>
<p style="text-align: justify;">
We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases.
</p>
<h3>Results</h3>
<p style="text-align: justify;">
Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA <i>versus </i>3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% <i>versus</i> 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF.
</p>
<h3>Conclusions</h3>
<p style="text-align: justify;">
Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies.
</p>
<h2>Keywords</h2>
<p style="text-align: justify;">
Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors.
</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] =>
Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
Patients and methods
We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases.
Results
Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA versus 3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% versus 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF.
Conclusions
Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies.
Keywords
Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28519
[VALUE] => Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28520
[VALUE] => 2765
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2765
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28529
[VALUE] => 2768
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2768
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Elena V. Morozova, Tatiana A. Rudakova, Julia Ju. Vlasova, Maria V. Barabanshchikova, Tatiana L. Gindina, Alexander L. Alyanskiy, Maria D. Vladovskaya, Ivan S. Moiseev, Ludmila S. Zubarovskaya, Alexander D. Kulagin
RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transplantology, Pavlov University, St. Petersburg, Russia
Correspondence:
Dr. Elena V. Morozova, RM Gorbacheva Research Institute of Pediatric Oncology, Hematology and Transpantology, Pavlov University, 6-8 L.Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (911) 927-82-29
E-mail: dr_morozova@mail.ru
Citation: Morozova EV, Rudakova TA, Vlasova JJ, et al. Pre- and post-transplantation factors associated with primary graft failure and severe poor graft function after allogeneic hematopoietic stem cell transplantation for chronic myeloid leukemia. Cell Ther Transplant 2022; 11(1): 13-23.
Allogeneic stem cell transplantation (allo-HSCT) is used worldwide for long-term management and cure of hematological malignancies, still remaining a valuable option for treatment of chronic myeloid leukemia (CML) in all fit patients who are unable to achieve a durable complete cytogenetic response after treatment with tyrosine kinase inhibitors (TKIs), and in advanced-phase disease. Along with relapse risk, the unfavorable HSCT results may be associated with primary graft failure (PrGF), or poor graft function (PoGF). Hence, the aim of our study was to assess frequency and outcome of PrGF and severe poor graft function (sPGF) after allo-HSCT in CML patients.
Patients and methods
We performed a retrospective analysis of 121 consecutive patients with CML who received allo-HSCT in the RM Gorbacheva Research Institute at the Pavlov University over 25 years. HSCT was indicated in cases of advanced-phase disease, or TKI resistance/intolerance of CML patients. BCR/ABL transcript levels and additional chromosomal abnormalities were used as laboratory markers of advanced disease. 80 patients (66%) were transplanted in chronic phase (CP); 41 patients (34%) were in acceleration phase (AP), or blast crisis (BC) at the time of HSCT. Matched unrelated donors were used in 65% of the cases; matched related donors, in 28%, and haploidentical donors, in 7% of cases.
Results
Engraftment was documented in 106 (88%) patients. Post-transplant relapses were registered in 31 patients within 15-333 days after HSCT. PrGF was documented in 8 cases (7%). Two patients developed secondary graft failure within two months after initial engraftment, with lethal infectious complications. Severe poor graft function (PoGF) was diagnosed in 11 cases (9%) at cumulative incidence of 10% within 1 year post-transplant. Among various pre-transplant characteristics, age factor, and, especially, presence of additional chromosomal abnormalities (ACA) were associated with cumulative incidence of PrGF and sPGF after HSCT. I.e., PrGF was 14% in the group with detectable ACA versus 3% in the group without ACA, (p=0.02), whereas incidence of sPGF in patients with ACA was 2% versus 12% in those without ACA (p=0.09). The incidence of post-transplant relapses did not differ in the patients with PrGF and sPGF.
Conclusions
Primary graft failure (PrGF) contributes to the non-relapse mortality during the first year after allo-HSCT in CML patients. Emergence of post-transplant relapses was not associated with PrGF and sPGF in CML. Further assessment of risk factors for the graft failure or poor graft function is required in order to improve the results of HSCT technologies.
Keywords
Chronic myeloid leukemia, hematopoietic stem cell transplantation, indications, graft failure, risk factors.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28554
[VALUE] => 11/16/2021 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 11/16/2021 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28555
[VALUE] => 12/15/2021 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 12/15/2021 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28558
[VALUE] => Array
(
[TEXT] => <p>Мохамед Р. Абдельфаттах, Хуссейн Эльсиеси</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Мохамед Р. Абдельфаттах, Хуссейн Эльсиеси
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28559
[VALUE] => Array
(
[TEXT] => <p>Отдел хирургии, Факультет медицины, Университет Александрии, Александрия, Египет </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Отдел хирургии, Факультет медицины, Университет Александрии, Александрия, Египет
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28560
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).</p>
<h3?Пациенты и методы</h3>
<p style="text-align: justify;">73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.</p>
<h3>Результаты</h3>
<p style="text-align: justify;">5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6). </p>
<h3>Выводы</h3>
<p style="text-align: justify;">Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.</p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость. </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Целью нашей работы было сравнение общей и безопухолевой заболеваемости у пациентов с гепатоцеллюлярной карциномой (ГЦК), леченных в нашем центре, после трансплантации печени от живых доноров (ЖД) и погибших доноров (ПД).
73 пациентам была выполнена трансплантация печени по поводу ГЦК, стадированной по Миланским критериям (MК). Эти пациенты были распределены по 2 группам: (a) 44 больных трансплантированных от ЖД, и (б) 29 пациентов получидли трансплантаты от ПД. Из исследования были искючены больные, не соответствующие Миланским критериям или пациенты после циторедуктивной локорегионарной терапии.
Результаты
5-летняя выживаемость составила, соответственно, 80,3% и 70,4% среди реципиентов печени от ЖД и ПД, тогда как безопухолевая выживаемость составляла 79,1% и 76%, соответственно, в группах больных, трансплантированных от живых и погибших доноров. Трансплантация печени от живых доноров показала несколько лучшие результаты, нежели трансплантация от погибшиз доноров (P=0.09). Однако разница по безопухолевой выживаемости между этими двумя группами не выявлена (P=0.6).
Выводы
Данное исследование подтвердило, что трансплантация печени от живых доноров, при несколько лучшей общей выживаемости, ассоциирована со сходными сроками безопухолевой выживаемости по сравнению с трансплантацией от погибших доноров. Это сходство особенно выражено при устранении возможных факторов, связанных с особенностями опухолей и анализом данных в хорошо сравнимых группах пациентов с ГЦК, классифицированных по Миланским критериям.
Ключевые слова
Гепатоцеллюлярная карцинома, трансплантация печени, живые доноры, погибшие доноры, выживаемость.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28556
[VALUE] => 10.18620/ctt-1866-8836-2022-11-1-43-49
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2022-11-1-43-49
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28561
[VALUE] => Array
(
[TEXT] => <p>Mohamed R. Abdelfattah, Hussein Elsiesy</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Mohamed R. Abdelfattah, Hussein Elsiesy
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28562
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt</p><br>
<p><b>Correspondence:</b><br>
Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131<br>
Phone: 002010 2306 1111<br>
Email: mohamad.rabie@gmail.com</p><br>
<p><b>Citation:</b> Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt
Correspondence:
Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131
Phone: 002010 2306 1111
Email: mohamad.rabie@gmail.com
Citation: Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28563
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">
Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) <i>versus </i>liver transplantation from deceased donor (DDLT) treated at our center.
</p>
<h3>Patients and methods</h3>
<p style="text-align: justify;">
Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study.
</p>
<h3>Results</h3>
<p style="text-align: justify;">
Overall survival outcomes at 5 years were, respectively, 80.3% <i>vs </i>70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% <i>vs</i> 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6).
<h3>Conclusion</h3>
<p style="text-align: justify;">The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.</p>
<h2>Keywords</h2>
<p style="text-align: justify;">Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival.
</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] =>
Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) versus liver transplantation from deceased donor (DDLT) treated at our center.
Patients and methods
Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study.
Results
Overall survival outcomes at 5 years were, respectively, 80.3% vs 70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% vs 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6).
Conclusion
The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.
Keywords
Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28557
[VALUE] => Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28564
[VALUE] => 2802
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2802
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28565
[VALUE] => 2803
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2803
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Mohamed R. Abdelfattah, Hussein Elsiesy
Department of Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt
Correspondence:
Prof. Dr. Mohamed Rabei Abdelfattah, Associate Professor, Department of Surgery, Faculty of Medicine, University of Alexandria, Azzaritta, Alexandria, Egypt, PO BOX 21131
Phone: 002010 2306 1111
Email: mohamad.rabie@gmail.com
Citation: Abdelfattah MR, Elsiesy H. Outcomes of liver transplantation to the patients with hepatocellular carcinoma from living donors versus transplants from deceased donors. Cell Ther Transplant 2022; 11(1): 43-49.
Our objective was to compare overall and tumor-free survival for the hepatocellular carcinoma (HCC) patients subjected to liver transplantation from living donor (LDLT) versus liver transplantation from deceased donor (DDLT) treated at our center.
Patients and methods
Seventy-three patients underwent liver transplantation for HCC staged according to Milan criteria (MC). The cases have been divided into two groups: (a) forty-four patients transplanted by means of LDLT, and (b) twenty-nine patients underwent DDLT. The patients beyond MC, or those who underwent downstaging locoregional therapy were excluded from the study.
Results
Overall survival outcomes at 5 years were, respectively, 80.3% vs 70.4%, in LDLT and DDLT groups whereas tumor-free survival was 79.1% vs 76% for LDLT and DDLT cases. LT from living donors showed slightly better patients’ survival compared to liver transplantation from deceased donors DDLT (P=0.09). However, the difference in tumor-free survival between both groups was virtually absent (P=0.6).
Conclusion
The present study confirmed that LDLT, while offering a slightly better overall survival, is associated with similar terms of tumor-free survival compared to transplants from deceased donors. This similarity is especially clear when avoiding biases caused by different tumor features and analyzing a perfectly matched cohort of patients presenting with HCC classified according to the Milan criteria.
Keywords
Hepatocellular carcinoma, liver transplant, living donor, deceased donor, survival.
Clinical studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28542
[VALUE] => 02/06/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 02/06/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28543
[VALUE] => 03/18/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 03/18/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28544
[VALUE] => Array
(
[TEXT] => <p>Олег И. Долгов<sup>1</sup>, Сергей А. Карпищенко<sup>1</sup>, Екатерина С. Утимишева<sup>1</sup>, Диана А. Григорьянц<sup>1</sup>, Анна А. Спиридонова<sup>1,2</sup>, Иван С. Моисеев<sup>1</sup>, Людмила С. Зубаровская<sup>1</sup>, Алексей Б. Чухловин<sup>1</sup>, Александр Д. Кулагин<sup>1</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Олег И. Долгов1, Сергей А. Карпищенко1, Екатерина С. Утимишева1, Диана А. Григорьянц1, Анна А. Спиридонова1,2, Иван С. Моисеев1, Людмила С. Зубаровская1, Алексей Б. Чухловин1, Александр Д. Кулагин1
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28545
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия<br>
<sup>2</sup> ФБУН НИИ эпидемиологии и микробиологии имени Пастера, Санкт-Петербург, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Первый Санкт-Петербургский государственный медицинский университет им. акад. И. П. Павлова, Санкт-Петербург, Россия
2 ФБУН НИИ эпидемиологии и микробиологии имени Пастера, Санкт-Петербург, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28546
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">
Трансплантация гемопоэтических стволовых клеток (ТГСК) часто сопровождается инфекционными осложнениями. Целью настоящего исследования была сравнительная оценка состава факультативно-анаэробных представителей микробиоты полости носа и его придаточных пазух при синусите, который нередко развивается у иммунокомпромиссных пациентов после интенсивной химио- и антибиотикотерапии и трансплантации гемопоэтических клеток (ТГСК).
</p>
<h3>Материалы и методы</h3>
<p style="text-align: justify;">
В исследовании участвовали 194 пациента с различными миело- и лимфопролиферативными заболеваниями в возрасте от 1 до 62 лет, проходившие интенсивную химиотерапию и аллогенную ТГСК. При наличии клинических показаний у пациентов забирали биоматериал (смывы из околоносовых пазух и/или назальные мазки) в сроки от -100 до +180 суток после аллогенной ТГСК. Исследовано 124 образца пунктатов верхнечелюстных пазух от 97 пациентов и 973 мазка-соскоба из полости носа. Посев биоматериала и выделение микроорганизмов проводили классическими бактериологическими методами. Чувствительность клинических изолятов к антибиотикам определяли диско-диффузионным методом. Интерпретацию результатов чувствительности осуществляли согласно критериям EUCAST.
</p>
<h3>Результаты</h3>
<p style="text-align: justify;">
В биоматериале из полости носа и околоносовых пазух наиболее часто высевали <i>S.epidermidis</i> – 34,7% (377/1097); <i>S.viridans</i> – 2,2% (24/1097); <i>S. aureus</i> – 1,91% (21/1097); <i>Klebsiella spp</i> – 1% (11/1097). Частота выявления <i>S.epidermidis</i> и <i>S.viridans</i> была минимальной в младшей возрастной группе (до 5 лет) и возрастала в группах от 15 лет и выше. Глубокое подавление роста <i>S.epidermidis</i> отмечалось (в особенности – в околоносовых синусах) в течение 1-го мес. после ТГСК на фоне массивной антибиотикотерапии. Отмечена высокая частота выявления <i>Klebsiella spp</i> в материале из синусов в поздние сроки (2-3 мес.) после ТГСК при малой частоте выявления в материале из полости носа (в среднем 16,3% против 2.1%, р=2×10^14). Кроме того, мы оценили частоту высеваемости бактерий в сроки +30 сут. от постановки диагноза синусита. При этом была выявлена повышенная частота выделения <i>Pseudomonas spp</i> (1/378 <i>vs </i>7/217) в материале из придаточных пазух.
</p>
<h3>Заключение</h3>
<p style="text-align: justify;">
Бактериологические исследование материала из гайморовых пазух имеет ограниченную ценность в течение 1-го мес. после ТГСК в связи с массивной антибиотикотерапией, которая сопровождается селекцией резистентных штаммов <i>Klebsiella spp, Pseudomonas spp, E.coli, S.aureus</i>, главным образом – в сроки 2 и более мес. после ТГСК.
</p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">
Tрансплантация гемопоэтических стволовых клеток, околоносовые пазухи, микробиота, антибиотикорезистентность.
</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] =>
Трансплантация гемопоэтических стволовых клеток (ТГСК) часто сопровождается инфекционными осложнениями. Целью настоящего исследования была сравнительная оценка состава факультативно-анаэробных представителей микробиоты полости носа и его придаточных пазух при синусите, который нередко развивается у иммунокомпромиссных пациентов после интенсивной химио- и антибиотикотерапии и трансплантации гемопоэтических клеток (ТГСК).
Материалы и методы
В исследовании участвовали 194 пациента с различными миело- и лимфопролиферативными заболеваниями в возрасте от 1 до 62 лет, проходившие интенсивную химиотерапию и аллогенную ТГСК. При наличии клинических показаний у пациентов забирали биоматериал (смывы из околоносовых пазух и/или назальные мазки) в сроки от -100 до +180 суток после аллогенной ТГСК. Исследовано 124 образца пунктатов верхнечелюстных пазух от 97 пациентов и 973 мазка-соскоба из полости носа. Посев биоматериала и выделение микроорганизмов проводили классическими бактериологическими методами. Чувствительность клинических изолятов к антибиотикам определяли диско-диффузионным методом. Интерпретацию результатов чувствительности осуществляли согласно критериям EUCAST.
Результаты
В биоматериале из полости носа и околоносовых пазух наиболее часто высевали S.epidermidis – 34,7% (377/1097); S.viridans – 2,2% (24/1097); S. aureus – 1,91% (21/1097); Klebsiella spp – 1% (11/1097). Частота выявления S.epidermidis и S.viridans была минимальной в младшей возрастной группе (до 5 лет) и возрастала в группах от 15 лет и выше. Глубокое подавление роста S.epidermidis отмечалось (в особенности – в околоносовых синусах) в течение 1-го мес. после ТГСК на фоне массивной антибиотикотерапии. Отмечена высокая частота выявления Klebsiella spp в материале из синусов в поздние сроки (2-3 мес.) после ТГСК при малой частоте выявления в материале из полости носа (в среднем 16,3% против 2.1%, р=2×10^14). Кроме того, мы оценили частоту высеваемости бактерий в сроки +30 сут. от постановки диагноза синусита. При этом была выявлена повышенная частота выделения Pseudomonas spp (1/378 vs 7/217) в материале из придаточных пазух.
Заключение
Бактериологические исследование материала из гайморовых пазух имеет ограниченную ценность в течение 1-го мес. после ТГСК в связи с массивной антибиотикотерапией, которая сопровождается селекцией резистентных штаммов Klebsiella spp, Pseudomonas spp, E.coli, S.aureus, главным образом – в сроки 2 и более мес. после ТГСК.
Ключевые слова
Tрансплантация гемопоэтических стволовых клеток, околоносовые пазухи, микробиота, антибиотикорезистентность.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28547
[VALUE] => 10.18620/ctt-1866-8836-2022-11-1-36-42
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2022-11-1-36-42
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28550
[VALUE] => Array
(
[TEXT] => <p>Oleg I. Dolgov<sup>1</sup>, Sergey A. Karpishchenko<sup>1</sup>, Ekaterina S. Utimisheva<sup>1</sup>, Diana A. Grigoryanz<sup>1</sup>, Anna A. Spiridonova<sup>1,2</sup>, Ivan S. Moiseev<sup>1</sup>, Ludmila S. Zubarovskaya<sup>1</sup>, Alexei B. Chukhlovin<sup>1</sup>, Alexander D. Kulagin<sup>1</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Oleg I. Dolgov1, Sergey A. Karpishchenko1, Ekaterina S. Utimisheva1, Diana A. Grigoryanz1, Anna A. Spiridonova1,2, Ivan S. Moiseev1, Ludmila S. Zubarovskaya1, Alexei B. Chukhlovin1, Alexander D. Kulagin1
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28551
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Pavlov University, St. Petersburg, Russia<br>
<sup>2</sup> St. Petersburg Pasteur Institute, St. Petersburg, Russia</p><br>
<p><b>Correspondence:</b><br>
Dr. Oleg I. Dolgov, Department of Otorhinolaryngology,
Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia<br>
Phone: +7 (921) 845-03-51<br>
E-mail: oidolgov@yandex.ru</p><br>
<p><b>Citation:</b> Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Pavlov University, St. Petersburg, Russia
2 St. Petersburg Pasteur Institute, St. Petersburg, Russia
Correspondence:
Dr. Oleg I. Dolgov, Department of Otorhinolaryngology,
Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (921) 845-03-51
E-mail: oidolgov@yandex.ru
Citation: Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28552
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">
Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT).
</p>
<h3>Materials and methods</h3>
<p style="text-align: justify;">
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria.
</p>
<h3>Results</h3>
<p style="text-align: justify;">
In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); <i>S.viridans</i> (2.2%, 24/1097); <i>S. aureus</i> (1.91%, 21/1097); <i>Klebsiella spp</i> (1%, 11/1097). Detection frequency of <i>S.epidermidis</i> and <i>S.viridans</i> was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of <i>S.epidermidis</i> growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of <i>Klebsiella spp</i> detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% <i>vs</i> 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of <i>Pseudomonas spp</i> isolation (1/378 <i>vs </i>7/217) was revealed in the material from paranasal sinuses.
</p>
<h3>Conclusion</h3>
<p style="text-align: justify;">
Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of <i>Klebsiella spp, Pseudomonas spp, E. coli, S. aureus</i>, mainly at the terms of >2 months after HSCT.
</p>
<h2>Keywords</h2>
<p style="text-align: justify;">
Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance.
</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] =>
Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT).
Materials and methods
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria.
Results
In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); S.viridans (2.2%, 24/1097); S. aureus (1.91%, 21/1097); Klebsiella spp (1%, 11/1097). Detection frequency of S.epidermidis and S.viridans was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of S.epidermidis growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of Klebsiella spp detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% vs 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of Pseudomonas spp isolation (1/378 vs 7/217) was revealed in the material from paranasal sinuses.
Conclusion
Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of Klebsiella spp, Pseudomonas spp, E. coli, S. aureus, mainly at the terms of >2 months after HSCT.
Keywords
Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28548
[VALUE] => Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28549
[VALUE] => 2788
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2788
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28553
[VALUE] => 2796
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2796
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Oleg I. Dolgov1, Sergey A. Karpishchenko1, Ekaterina S. Utimisheva1, Diana A. Grigoryanz1, Anna A. Spiridonova1,2, Ivan S. Moiseev1, Ludmila S. Zubarovskaya1, Alexei B. Chukhlovin1, Alexander D. Kulagin1
1 Pavlov University, St. Petersburg, Russia
2 St. Petersburg Pasteur Institute, St. Petersburg, Russia
Correspondence:
Dr. Oleg I. Dolgov, Department of Otorhinolaryngology,
Pavlov University, 6-8 Tolstoy St, 197022, St. Petersburg, Russia
Phone: +7 (921) 845-03-51
E-mail: oidolgov@yandex.ru
Citation: Dolgov OI, Karpishchenko SA, Utimisheva ES, et al. Microbiota of nasal cavity in sinusitis following hematopoietic stem cell transplantation. Cell Ther Transplant 2022; 11(1): 36-42.
Hematopoietic stem cell transplantation (HSCT) is often accompanied by infectious complications. The aim of this study was a comparative evaluation of facultative anaerobic microbiota members of nasal and paranasal cavity in sinusitis, which often develops in immunocompromised patients, due to intensive chemotherapy and massive antibiotic treatment followed by hematopoietic cell transplantation (HSCT).
Materials and methods
The study involved 194 patients with various myelo- and lymphoproliferative diseases aged 1 to 62 years who underwent intensive chemotherapy and allogeneic HSCT. As based on appropriate clinical indications, the biomaterial was taken from patients (washings from the paranasal sinuses and/or nasal swabs) within the time period of +100 to +180 days after allogeneic HSCT. We studied 124 samples from maxillary sinus punctures of 97 patients and 973 scrapings from the nasal cavity. Seeding of biological material and isolation of the microorganisms were performed by classical bacteriological techniques. Antibiotic susceptibility of clinical isolates was determined by disk diffusion methods. The data on microbial sensitivity were interpreted by the EUCAST criteria.
Results
In the samples from nasal cavity and paranasal sinuses, S. epidermidis was most often detected (34.7%, 377/1097); S.viridans (2.2%, 24/1097); S. aureus (1.91%, 21/1097); Klebsiella spp (1%, 11/1097). Detection frequency of S.epidermidis and S.viridans was minimal in the younger age group (up to 5 years), and increased in older groups (>15 years old). Profound suppression of S.epidermidis growth was noted, especially in paranasal sinuses, within 1 month after HSCT in presence of massive antibiotic therapy. High frequency of Klebsiella spp detection was noted in the samples from maxillar sinuses at later terms (2-3 months) after HSCT, at low detection frequency of the pathogen in the specimens from nasal cavity (average 16.3% vs 2.1%, p=2×10^14). In addition, we have estimated frequency of bacterial inoculation within +30 days upon the diagnosis of sinusitis. At the same time, an increased frequency of Pseudomonas spp isolation (1/378 vs 7/217) was revealed in the material from paranasal sinuses.
Conclusion
Bacteriological study of biological samples from maxillary sinuses is of limited value during the 1st month after HSCT accompanied by massive antibiotic therapy which was followed by selection of resistant strains of Klebsiella spp, Pseudomonas spp, E. coli, S. aureus, mainly at the terms of >2 months after HSCT.
Keywords
Hematopoietic stem cell transplantation, paranasal sinuses, microbiota, antibiotic resistance.
Clinical case
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28566
[VALUE] => 01/25/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 01/25/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28567
[VALUE] => 03/18/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 03/18/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28568
[VALUE] => Array
(
[TEXT] => <p>Елена Н. Паровичникова, Вера А. Васильева, Ольга А. Алешина, Мария В. Довыденко, Лариса А. Кузьмина,
Михаил Ю. Дроков, Ирина А. Лукьянова, Вера В. Троицкая, Евгений Е. Звонков, Алла М. Ковригина,
<span style="border: 1px solid black; margin: 0; padding: 2px 2px;">Валерий Г. Савченко</span></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Елена Н. Паровичникова, Вера А. Васильева, Ольга А. Алешина, Мария В. Довыденко, Лариса А. Кузьмина,
Михаил Ю. Дроков, Ирина А. Лукьянова, Вера В. Троицкая, Евгений Е. Звонков, Алла М. Ковригина,
Валерий Г. Савченко
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28569
[VALUE] => Array
(
[TEXT] => <p>Национальный медицинский исследовательский центр гематологии, Москва, Россия</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Национальный медицинский исследовательский центр гематологии, Москва, Россия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28570
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток. </p>
<p style="text-align: justify;">Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.</p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Посттрансплантационное лимфопролиферативное заболевание (ПТЛЗ) одно из частых осложнений после органной трансплантации. Основной целью лечения ПТЛЗ является достижение стойкой ремиссии заболевания и сохранение трансплантированного органа. Однако не редко после проведенной терапии ПТЛЗ требуется возврат проведения иммуносупрессивной терапии трансплантированного органа, что может вновь привести к рецидиву ПТЛЗ. Консолидирующее лечение в виде трансплантации аутологичных гемопоэтических стволовых клеток проводят редко. Роль трансплантации аллогенных гемопоэтических стволовых клеток в терапии ПТЛЗ после трансплантации солидного органа не определена, в связи с высокими рисками токсичности для трансплантированного органа, развитие реакция трансплантат против хозяина может привести к отторжению трансплантированного солидного органа, но и наличие трансплантата солидного может увеличить вероятность отторжения гемопоэтических стволовых клеток.
Нами впервые описан случай выполнения трансплантации гаплоидентичных гемопоэтических стволовых клеток с TCRαβ+/CD19+ деплецией трансплантата у больной во второй ремиссии диффузной B-крупноклеточной лимфомы, ассоциированной с иммуносупрессивной терапией, проводимой по поводу ранее выполненной трансплантации аллогенной трупной почки.
Ключевые слова
Посттрансплантационное лимфопролиферативное заболевание, трансплантация гемопоэтических стволовых клеток, гаплоидентичная, TCRαβ+/CD19+ деплеция трансплантата.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28571
[VALUE] => 10.18620/ctt-1866-8836-2022-11-1-50-57
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2022-11-1-50-57
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28572
[VALUE] => Array
(
[TEXT] => <p>Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina,
Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, <span style="border: 1px solid black; margin: 0; padding: 2px 2px;">Valery G. Savchenko</span>
</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina,
Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, Valery G. Savchenko
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28573
[VALUE] => Array
(
[TEXT] => <p>National Medical Research Center for Hematology, Moscow, Russia</p><br>
<p><b>Correspondence:</b><br>
Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia<br>
Phone: +7 (916) 262-23-16<br>
E-mail: vasilievaVA4@mail.ru</p>
<br>
<p><b>Citation:</b> Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => National Medical Research Center for Hematology, Moscow, Russia
Correspondence:
Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia
Phone: +7 (916) 262-23-16
E-mail: vasilievaVA4@mail.ru
Citation: Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28574
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells. </p>
<p style="text-align: justify;">We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.</p>
<h2>Keywords</h2>
<p style="text-align: justify;">Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells.
We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.
Keywords
Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28575
[VALUE] => A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28576
[VALUE] => 2807
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2807
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28577
[VALUE] => 2808
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2808
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Elena N. Parovichnikova, Vera A. Vasilyeva, Olga A. Aleshina, Mariya V. Dovydenko, Larisa A. Kuzmina, Mikhail Yu. Drokov, Irina A. Lukyanova, Vera V. Troitskaya, Evgenii E. Zvonkov, Alla M. Kovrigina, Valery G. Savchenko
National Medical Research Center for Hematology, Moscow, Russia
Correspondence:
Dr. Vera A. Vasilyeva, PhD, MD, Head Immunochemotherapy Department for BMT patients, National Medical Research Center for Hematology, 4 Novyi Zykovskii Lane, Moscow, 125167, Russia
Phone: +7 (916) 262-23-16
E-mail: vasilievaVA4@mail.ru
Citation: Parovichnikova EN, Vasilyeva VA, Aleshina OA et al. A case report of haploidentical hematopoietic stem cell transplantation for diffuse large B-cell lymphoma developing in the course of immunosuppressive therapy after kidney transplantation. Cell Ther Transplant 2022; 11(1): 50-57.
Post-transplant lymphoproliferative disease (PTLD) is one of the most common complications after organ transplantation. The main goal of PTLD treatment is to achieve stable remission of the disease and preserve the transplanted organ. However, it is not uncommon that after PTLD therapy immunosuppressive therapy for the transplanted organ is returned, which may again lead to a recurrence of PTLD. Autologous hematopoietic stem cell transplantation is a rare option for treatment PTLD. The role of allogeneic hematopoietic stem cell transplantation (HSCT) in PTLD therapy after solid organ transplantation has not been determined, due to the high risks of toxicity for the transplanted organ, the development of a graft-versus-host disease may lead to rejection of the transplanted solid organ, and the presence of a solid organ transplant may increase the rejection of hematopoietic stem cells.
We have described a case report of haploidentical hematopoietic allogeneic stem cell transplantation with TCR αβ+/CD19+ cell depletion for a patient with second remission of diffuse large B-cell lymphoma associated with immunosuppressive therapy for a previously performed allogeneic cadaveric kidney transplantation.
Keywords
Post-transplant lymphoproliferative disease, hematopoietic allogeneic stem cell transplantation, haploidentical, TCR αβ+/CD19+ cell depletion.
Experimental studies
Array
(
[KEYWORDS] => Array
(
[ID] => 19
[TIMESTAMP_X] => 2015-09-03 10:46:01
[IBLOCK_ID] => 2
[NAME] => Ключевые слова
[ACTIVE] => Y
[SORT] => 500
[CODE] => KEYWORDS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 19
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 4
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => Y
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => Y
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Ключевые слова
[~DEFAULT_VALUE] =>
)
[SUBMITTED] => Array
(
[ID] => 20
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата подачи
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUBMITTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 20
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28578
[VALUE] => 10/13/2021 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10/13/2021 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата подачи
[~DEFAULT_VALUE] =>
)
[ACCEPTED] => Array
(
[ID] => 21
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата принятия
[ACTIVE] => Y
[SORT] => 500
[CODE] => ACCEPTED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 21
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28579
[VALUE] => 01/28/2022 12:00:00 am
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 01/28/2022 12:00:00 am
[~DESCRIPTION] =>
[~NAME] => Дата принятия
[~DEFAULT_VALUE] =>
)
[PUBLISHED] => Array
(
[ID] => 22
[TIMESTAMP_X] => 2015-09-02 17:21:42
[IBLOCK_ID] => 2
[NAME] => Дата публикации
[ACTIVE] => Y
[SORT] => 500
[CODE] => PUBLISHED
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 22
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => DateTime
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Дата публикации
[~DEFAULT_VALUE] =>
)
[CONTACT] => Array
(
[ID] => 23
[TIMESTAMP_X] => 2015-09-03 14:43:05
[IBLOCK_ID] => 2
[NAME] => Контакт
[ACTIVE] => Y
[SORT] => 500
[CODE] => CONTACT
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 23
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Контакт
[~DEFAULT_VALUE] =>
)
[AUTHORS] => Array
(
[ID] => 24
[TIMESTAMP_X] => 2015-09-03 10:45:07
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHORS
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => E
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => Y
[XML_ID] => 24
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 3
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] => EAutocomplete
[USER_TYPE_SETTINGS] => Array
(
[VIEW] => E
[SHOW_ADD] => Y
[MAX_WIDTH] => 0
[MIN_HEIGHT] => 24
[MAX_HEIGHT] => 1000
[BAN_SYM] => ,;
[REP_SYM] =>
[OTHER_REP_SYM] =>
[IBLOCK_MESS] => N
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] =>
)
[AUTHOR_RU] => Array
(
[ID] => 25
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Авторы
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 25
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28580
[VALUE] => Array
(
[TEXT] => <p>Дима Джуджех<sup>1</sup>, Абдулджалил Гревати<sup>1</sup>, Чади Суккариех<sup>2</sup>, Аднан Альмаррави<sup>1</sup>, Джамал А. Н. Дарвича<sup>3</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Дима Джуджех1, Абдулджалил Гревати1, Чади Суккариех2, Аднан Альмаррави1, Джамал А. Н. Дарвича3
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Авторы
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_RU] => Array
(
[ID] => 26
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Организации
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 26
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28581
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Департамент биотехнологической инженерии, Факультет технической инженерии, Университет Алеппо, Сирия<br>
<sup>2</sup> Департамент биологии животных, Факультет наук, Университет Дамаска, Сирия<br>
<sup>3</sup> Департамент фармакологии и токсикологии, Факультет фармации, Арабский международный университет, Сирия </p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Департамент биотехнологической инженерии, Факультет технической инженерии, Университет Алеппо, Сирия
2 Департамент биологии животных, Факультет наук, Университет Дамаска, Сирия
3 Департамент фармакологии и токсикологии, Факультет фармации, Арабский международный университет, Сирия
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Организации
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_RU] => Array
(
[ID] => 27
[TIMESTAMP_X] => 2015-09-02 18:01:20
[IBLOCK_ID] => 2
[NAME] => Описание/Резюме
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 27
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28582
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Терапия стволовыми клетками является перспективнмым видом лечения болезней печени. В данной работе изучали эффект мезенхимных стволовых клеток (МСК), полученных из костного мозга, для лечения повреждения печени, вызванного CCl<sub>4</sub>. </p>
<h3>Материалы и методы</h3>
<p style="text-align: justify;">Мышам Balb/c вводили CCl<sub>4</sub> (1 мл/кг массы тела) или физиологический раствор (в качестве контроля) дважды в неделю на протяжении 7 недель. Затем животным вводили внутривенно МСК с пассажа 0. Через 4 нед. после трансплантации определяли уровни АЛаТ, АСаТ, щелочной фосфатазы и альбумина в сыворотке крови, проводили гистологическое исследование печени, и измеряли уровни IL-4 и IFN-γ посредством методики ИФА.</>
<h3>Результаты</h3>
<p style="text-align: justify;">По сравнению с группой контроля (с введением физ.раствора), в группе, леченной МСК, были показаны более низкие уровни АЛаТ и АСаТ. Были также выявлены позитивные изменения сывороточного альбумина. Данные гистологического исследования согласовывались с данными биохимических анализов, указывая на лучшие показатели в группе, леченной МСК, по сравнению с контрольной группой. Кроме того, трансплантация МСК сопровождалась повышением продукции IL-4 и IFN-γ по сравнению с контролем.</p>
<h3>Выводы</h3>
<p style="text-align: justify;">Наши результаты показали, что трансплантация сингенных МСК может облегчить восстановление после химической индукции повреждения печени, несмотря на вызванный иммунный ответ. Поэтому трансплантация МСК может быть основой для новой концепции лечения заболеваний печени.</p>
<h2>Ключевые слова</h2>
<p style="text-align: justify;">Мыши, повреждение печени, CCl<sub>4</sub>, стволовые клетки костного мозга, мезенхимные, трансплантация клеток.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Терапия стволовыми клетками является перспективнмым видом лечения болезней печени. В данной работе изучали эффект мезенхимных стволовых клеток (МСК), полученных из костного мозга, для лечения повреждения печени, вызванного CCl4.
Материалы и методы
Мышам Balb/c вводили CCl4 (1 мл/кг массы тела) или физиологический раствор (в качестве контроля) дважды в неделю на протяжении 7 недель. Затем животным вводили внутривенно МСК с пассажа 0. Через 4 нед. после трансплантации определяли уровни АЛаТ, АСаТ, щелочной фосфатазы и альбумина в сыворотке крови, проводили гистологическое исследование печени, и измеряли уровни IL-4 и IFN-γ посредством методики ИФА.
Результаты
По сравнению с группой контроля (с введением физ.раствора), в группе, леченной МСК, были показаны более низкие уровни АЛаТ и АСаТ. Были также выявлены позитивные изменения сывороточного альбумина. Данные гистологического исследования согласовывались с данными биохимических анализов, указывая на лучшие показатели в группе, леченной МСК, по сравнению с контрольной группой. Кроме того, трансплантация МСК сопровождалась повышением продукции IL-4 и IFN-γ по сравнению с контролем.
Выводы
Наши результаты показали, что трансплантация сингенных МСК может облегчить восстановление после химической индукции повреждения печени, несмотря на вызванный иммунный ответ. Поэтому трансплантация МСК может быть основой для новой концепции лечения заболеваний печени.
Ключевые слова
Мыши, повреждение печени, CCl4, стволовые клетки костного мозга, мезенхимные, трансплантация клеток.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Описание/Резюме
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[DOI] => Array
(
[ID] => 28
[TIMESTAMP_X] => 2016-04-06 14:11:12
[IBLOCK_ID] => 2
[NAME] => DOI
[ACTIVE] => Y
[SORT] => 500
[CODE] => DOI
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 28
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28583
[VALUE] => 10.18620/ctt-1866-8836-2022-11-1-58-68
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 10.18620/ctt-1866-8836-2022-11-1-58-68
[~DESCRIPTION] =>
[~NAME] => DOI
[~DEFAULT_VALUE] =>
)
[AUTHOR_EN] => Array
(
[ID] => 37
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Author
[ACTIVE] => Y
[SORT] => 500
[CODE] => AUTHOR_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 37
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28584
[VALUE] => Array
(
[TEXT] => <p>Dima Joujeh<sup>1</sup>, Abduljalil Ghrewaty<sup>1</sup>, Chadi Soukkarieh<sup>2</sup>, Adnan Almarrawi<sup>1</sup>, Jamal Abdul Naser Darwicha<sup>3</sup></p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Dima Joujeh1, Abduljalil Ghrewaty1, Chadi Soukkarieh2, Adnan Almarrawi1, Jamal Abdul Naser Darwicha3
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Author
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[ORGANIZATION_EN] => Array
(
[ID] => 38
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Organization
[ACTIVE] => Y
[SORT] => 500
[CODE] => ORGANIZATION_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 38
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28585
[VALUE] => Array
(
[TEXT] => <p><sup>1</sup> Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria<br>
<sup>2</sup> Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria<br>
<sup>3</sup> Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria</p><br>
<p><b>Correspondence:</b><br>
Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria<br>
Phone: (+963) 994-046-745<br>
E-mail: dimajoujeh@gmail.com</p><br>
<p><b>Citation:</b> Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL<sub>4</sub>-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => 1 Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
2 Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria
3 Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria
Correspondence:
Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
Phone: (+963) 994-046-745
E-mail: dimajoujeh@gmail.com
Citation: Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Organization
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[SUMMARY_EN] => Array
(
[ID] => 39
[TIMESTAMP_X] => 2015-09-02 18:02:59
[IBLOCK_ID] => 2
[NAME] => Description / Summary
[ACTIVE] => Y
[SORT] => 500
[CODE] => SUMMARY_EN
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 39
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] => 28586
[VALUE] => Array
(
[TEXT] => <p style="text-align: justify;">Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl<sub>4</sub> treatment was investigated.</p>
<h3>Materials and methods</h3>
<p style="text-align: justify;">Balb/c mice were injected by (1 ml/kg body weight) of CCl<sub>4</sub> twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ. </p>
<h3>Results</h3>
<p style="text-align: justify;">As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.</p>
<h3>Conclusion</h3>
<p style="text-align: justify;">Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.</p>
<h2>Keywords</h2>
<p style="text-align: justify;">Mice, liver damage, CCl<sub>4</sub>, bone marrow stromal cells, mesenchymal, cell transplantation.</p>
[TYPE] => HTML
)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Array
(
[TEXT] => Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl4 treatment was investigated.
Materials and methods
Balb/c mice were injected by (1 ml/kg body weight) of CCl4 twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ.
Results
As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.
Conclusion
Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.
Keywords
Mice, liver damage, CCl4, bone marrow stromal cells, mesenchymal, cell transplantation.
[TYPE] => HTML
)
[~DESCRIPTION] =>
[~NAME] => Description / Summary
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[NAME_EN] => Array
(
[ID] => 40
[TIMESTAMP_X] => 2015-09-03 10:49:47
[IBLOCK_ID] => 2
[NAME] => Name
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 80
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 40
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => Y
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28587
[VALUE] => Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study)
[~DESCRIPTION] =>
[~NAME] => Name
[~DEFAULT_VALUE] =>
)
[FULL_TEXT_RU] => Array
(
[ID] => 42
[TIMESTAMP_X] => 2015-09-07 20:29:18
[IBLOCK_ID] => 2
[NAME] => Полный текст
[ACTIVE] => Y
[SORT] => 500
[CODE] => FULL_TEXT_RU
[DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 42
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 200
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Полный текст
[~DEFAULT_VALUE] => Array
(
[TEXT] =>
[TYPE] => HTML
)
)
[PDF_RU] => Array
(
[ID] => 43
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF RUS
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_RU
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 43
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28588
[VALUE] => 2813
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2813
[~DESCRIPTION] =>
[~NAME] => PDF RUS
[~DEFAULT_VALUE] =>
)
[PDF_EN] => Array
(
[ID] => 44
[TIMESTAMP_X] => 2015-09-09 16:05:20
[IBLOCK_ID] => 2
[NAME] => PDF ENG
[ACTIVE] => Y
[SORT] => 500
[CODE] => PDF_EN
[DEFAULT_VALUE] =>
[PROPERTY_TYPE] => F
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 44
[FILE_TYPE] => doc, txt, rtf, pdf
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] =>
[USER_TYPE_SETTINGS] =>
[HINT] =>
[PROPERTY_VALUE_ID] => 28589
[VALUE] => 2814
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] => 2814
[~DESCRIPTION] =>
[~NAME] => PDF ENG
[~DEFAULT_VALUE] =>
)
[NAME_LONG] => Array
(
[ID] => 45
[TIMESTAMP_X] => 2023-04-13 00:55:00
[IBLOCK_ID] => 2
[NAME] => Название (для очень длинных заголовков)
[ACTIVE] => Y
[SORT] => 500
[CODE] => NAME_LONG
[DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
[PROPERTY_TYPE] => S
[ROW_COUNT] => 1
[COL_COUNT] => 30
[LIST_TYPE] => L
[MULTIPLE] => N
[XML_ID] => 45
[FILE_TYPE] =>
[MULTIPLE_CNT] => 5
[TMP_ID] =>
[LINK_IBLOCK_ID] => 0
[WITH_DESCRIPTION] => N
[SEARCHABLE] => N
[FILTRABLE] => N
[IS_REQUIRED] => N
[VERSION] => 1
[USER_TYPE] => HTML
[USER_TYPE_SETTINGS] => Array
(
[height] => 80
)
[HINT] =>
[PROPERTY_VALUE_ID] =>
[VALUE] =>
[DESCRIPTION] =>
[VALUE_ENUM] =>
[VALUE_XML_ID] =>
[VALUE_SORT] =>
[~VALUE] =>
[~DESCRIPTION] =>
[~NAME] => Название (для очень длинных заголовков)
[~DEFAULT_VALUE] => Array
(
[TYPE] => HTML
[TEXT] =>
)
)
)
Dima Joujeh1, Abduljalil Ghrewaty1, Chadi Soukkarieh2, Adnan Almarrawi1, Jamal Abdul Naser Darwicha3
1 Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
2 Department of Animal Biology, Faculty of Sciences, Damascus University, Damascus, Syria
3 Department of Pharmacology and Toxicology, Faculty of Pharmacy, Arab International University, Syria
Correspondence:
Dr. Dima Joujeh, Department of Biotechnology Engineering, Faculty of Technical Engineering, University of Aleppo, Syria
Phone: (+963) 994-046-745
E-mail: dimajoujeh@gmail.com
Citation: Joujeh D, Ghrewaty A, Soukkarieh C et al. Therapeutic potential of mouse bone marrow mesenchymal stromal cells transplantation in ameliorating of CCL4-induced liver damage (in vivo study). Cell Ther Transplant 2022; 11(1): 58-68.
Liver diseases pose a major global health problem. In this study, the effect of bone marrow derived mesenchymal stromal cells MSC(M) in liver damage induced by CCl4 treatment was investigated.
Materials and methods
Balb/c mice were injected by (1 ml/kg body weight) of CCl4 twice a week for 7 weeks. The mice were then intravenously injected with MSC(M) (at the passage 0), or physiological saline (PBS, control group). Four weeks after transplantation, serum levels of ALT, AST, ALP and albumin were measured, liver histopathology was performed, and ELISA technique was carried out to detect the serum levels of IL-4 and IFN-γ.
Results
As compared with PBS-treated animals, MSC(M)- treated group presented with lower levels of ALT and ALP, being also associated with less pronounced changes in serum albumin. Histological study was consistent with biochemical data, suggesting an improvement in MSC(M)-treated group compared with PBS group. Transplantation of MSC(M) increased production of IL-4 and IFN-γ compared to PBS group.
Conclusion
Our results demonstrated that MSC(M) transplantation could facilitate recovery from chemically induced liver damage. Therefore, MSC(M) transplantation may represent a new concept for the treatment of liver diseases.
Keywords
Mice, liver damage, CCl4, bone marrow stromal cells, mesenchymal, cell transplantation.

