Initial report on a phase I clinical trial: Prevention and treatment of post-operative Acute Kidney Injury with allogeneic Mesenchymal Stem Cells in patients who require on-pump cardiac surgery
Anna Gooch1, John Doty2, Jean Flores2, LeAnne Swenson2, Florian E Toegel1,3, George R Reiss4, Claudia Lange5, Axel R Zander5, Zhuma Hu1, Scott Poole1, Ping Zhang1 and Christof Westenfelder1,6
1Division of Nephrology, Department of Medicine, University of Utah Health Sciences Center and George E. Wahlen VA HCS, Salt Lake City, Utah, USA; 2Division of Cardiovascular Surgery, Intermountain Medical Center, Murray, Utah, USA; 3Jacobi Hospital, Albert Einstein College of Medicine affiliated Medical Center, Bronx, New York, USA; 4Division of Cardiovascular Surgery, Department of Surgery, University of Utah Health Sciences Center, and Research Service, George E. Wahlen VA HCS, Salt Lake City, Utah, USA; 5Bone Marrow Transplantation Center, University of Hamburg, Germany; 6Department of Physiology, University of Utah Health Sciences Center, Salt Lake City, Utah, USA
Correspondence:
Christof Westenfelder, MD, Section of Nephrology (111 N), George E. Wahlen VA Health Sciences Center, 500 Foothill Blvd., Salt Lake City, UT 84148, USA
E-mail: christof.westenfelder@hsc.utah.edu
Accepted 15 December 2008
Published 24 December 2008
Summary
Based on our extensive pre-clinical data that show that ischemia/reperfusion-induced Acute Kidney Injury (AKI), an essentially treatment resistant complication in patients, can be effectively treated by the administration of allogeneic Mesenchymal Stem Cells (MSC), an FDA approved, Phase I Clinical Trial (www.clinicaltrials.gov; NCT00733876) in patients who are at high risk of developing severe AKI post open heart surgery is currently being conducted. In this safety trial, patients who are undergoing on-pump coronary artery bypass surgery or cardiac valve repair, who are older than 65 years, with underlying renal disease, diabetes mellitus, hypertension, coronary artery disease, congestive heart failure and/or chronic obstructive pulmonary disease will be infused with allogeneic MSC following completion of surgery. The MSC are dosed in an escalating fashion, the initial five patients being infused via a femoral catheter that is placed into the suprarenal aorta with a defined low dose of MSC/kg body weight. This report summarizes the clinical course of the first five patients that have been treated according to this protocol. The renal function did not deteriorate post operatively in any of these patients, nor were adverse (AE) or severe adverse events (SAE) observed to date. However, one patient died suddenly 26 days after discharge from causes that both the principal investigator and the members of the Data and Safety Monitoring Board judged as being unrelated to the study drug and its route of administration. The next group of five study subjects will receive an intermediate dose of MSC/kg body weight, and if no safety concerns arise with this dose, the final five patients will be treated with a high dose of MSC/kg body weight. Preliminary efficacy of MSC therapy in the prevention and treatment of post-operative AKI in this high risk cohort of cardiac surgery patients will be assessed by comparing outcomes in study subjects (frequency, severity and duration of post-operative AKI, dialysis dependency [temporary, permanent], length of stay, and death at 30 days) to those in a large number of historical controls (data base at www.STS.org).
Keywords
Clinical trials, mesenchymal stem cells, acute kidney injury, cell therapy
Introduction
AKI remains a common, serious, and essentially treatment resistant syndrome of rapidly declining renal function. The mortality rates from AKI range from 15% in the general community to 80% for patients with multi-organ failure or for those who develop it post-operatively [1]. Even when renal function appears to fully recover after AKI, it is now recognized that a significant proportion of patients develop end stage renal disease (ESRD) as a consequence of undiagnosed, incompletely resolved AKI, characterized by continued inflammatory and fibrotic processes, and microvascular rarefaction [2]. Consequently, those patients who seemingly recover from AKI frequently go on to develop chronic kidney disease (CKD), eventually requiring chronic hemodialysis or a renal transplant [3].
AKI is most frequently seen in patients with shock, sepsis, trauma, and after major surgery. Patients undergoing cardiac surgery are at particularly high risk with up to 30% of all cardiac surgery patients developing AKI [4]. Many studies of cardiac patients have consistently found certain factors to be associated with increased risk of developing AKI following surgery. These risks include but are not limited to: the type of procedure performed (valve procedures are found to be of particularly high risk); patient age greater than 65; female patient gender; pre-operative serum creatinine value above 1.2 mg/dL, or underlying renal disease; pre-operative capillary glucose above 140 mg/dL; congestive heart failure; combined surgeries; on-pump vs. off pump surgery; and cardiopulmonary bypass surgery time greater than two hours [4-6]. The treatment resistant nature of AKI, combined with high morbidity and mortality, as well as the now recognized frequent progression of AKI to chronic kidney disease (CKD) underscores the urgent need for advances in treatment modalities.
Recent studies from our laboratory have led to the development of a novel approach to AKI treatment. This treatment administers allogeneic or syngeneic MSC to prevent further damage and to facilitate repair of acutely injured kidneys [7-9]. We observed that immediate (post reflow) or delayed (24 hrs post reflow) treatment of I/R AKI in rats with either autologous or allogeneic MSC significantly protects renal function, improves survival and hastens renal repair, mediated by complex paracrine mechanisms (anti-apoptotic, mitogenic, anti-inflammatory, vasculoprotective, angiogenic, anti-fibrotic) 7-10]. The striking hypoimmunogenic and immune modulating properties of MSC make their therapeutic use in allogeneic protocols possible and safe, as has been demonstrated in numerous clinical (www.clinicaltrials.gov) and pre-clinical trials [11, 12].
Compared to vehicle treated animals with I/R AKI, early allogeneic MSC therapy has important late benefits (3 months post AKI) such as maintained creatinine clearance, decreased interstitial fibrosis, and down regulation of pro-fibrotic gene expression levels in the kidney (TGFβ, PAI-1, TIMP-1). In addition, MSC therapy for AKI results in well maintained microvascular density in the kidney, while there is significant micorvascular rarefaction in vehicle treated animals [7]. In AKI, administered MSC do not engraft and disappear from the kidney and other organs within 1 to 3 days.
The aforementioned preclinical studies indicate that effective and specific treatment of AKI with MSC is an intervention that also prevents progressive loss of renal function, a complication that is increasingly recognized to result in ESRD in patients in whom AKI was not diagnosed and treated early after a renal insult [13]. Accordingly, a Phase I Clinical Trial employing this treatment is currently underway (www.clinicaltrials.gov; NCT00733876). This safety trial involves administration of MSC to fifteen patients divided into three cohorts of five patients each. Each cohort receives a defined dose of MSC, low, intermediate or high. As of this writing, dosing of the first cohort is complete, and we report here the outcomes of the first cohort of five patients.
Study Design and Methods
The FDA and the Institutional Review Board of Intermountain Medical Center, Murray, Utah, the site where the trial is carried out, approved the design and conduct of this Phase I Clinical Safety Trial. In addition, prior to initiation of the trial an independent Data Safety and Monitoring Board (DSMB) was appointed, consisting of a general nephrologists, a nephrologist/medical epidemiologist, and a cardiovascular surgeon. This DSMB reviewed the trial protocol and approved the trial, and continues to monitor the clinical data from all enrolled and treated subjects.
The study design is a Phase 1 Safety Trial. The primary objective is to test whether infusion of allogeneic MSC into the suprarenal aorta of patients who have undergone on-pump cardiac surgery (Coronary Artery Bypass Grafting and/or valve surgery) and who are at high risk for AKI following surgery is safe. This is assessed by monitoring patients post operatively for the occurrence of adverse events (AEs) and serious adverse events (SAEs) that are related to the MSC therapy. Specifically, detailed, monthly examinations for six months regarding the development of AEs or SAEs are carried out, and the study subjects are reassessed annually for another three years.
The major endpoint to be measured is safety, as documented by the comparative incidence of Adverse Events, Severe Adverse Events and complications in patients receiving cell-based therapies vs. historical controls for this patient population. AEs will be recorded throughout the course of the study and classified as immediate, postoperative, or delayed. Both common, expected and unusual AEs are listed below.
Potential immediate or early AEs related to the infusion of MSC via a femoral catheter into the suprarenal aorta include femoral catheter related complications such as bleeding at the catheter insertion site, infections, cholesterol plaque dislodgement and secondary visceral or peripheral embolic events.
Immediate AEs and SAEs occurring at the time of operation and immediately post-op (up to 24 hours post-op) include the following: post-operative compromise of heart function due to an unexpected ischemic event; post-operative marked impairment of renal function due to an unexpected ischemic coronary or other event (bleeding, hypotension, heart failure); perioperative complications that will require additional time in order to address these.
Later, post-operative complications (1-30 days post-op) include delayed deterioration in renal function post-op, requiring or not requiring dialysis; bleeding requiring >6 units of blood transfusion; arrhythmia requiring cardioversion; mediastinitis; cerebral vascular accident; prolonged ventilator support (> 24 hours postoperatively); reintubation; acute myocardial infarction; wound infection or hematoma; pericarditis; pneumonia; pulmonary embolism; bacteremia, sepsis, shock; multiorgan failure; death.
Delayed (more than 30 days after operation) AEs and SAEs include: dialysis dependency due to irreversible loss of kidney function; arrhythmia requiring cardioversion; mediastinitis; cerebral vascular accident; acute myocardial infarction; wound infection or hematoma; pneumonia; pulmonary embolism; malignancy; ectopic differentiation of MSC into mesodermal cells (bone, cartilage, fat); death.
The secondary objective of this trial is preliminary efficacy of MSC administration for the potential prevention and treatment of post-operative AKI. Although a priori underpowered, preliminary efficacy in this trial is nevertheless assessed by determining the comparative frequency and severity of post-operative AKI using standard and novel biomarkers of AKI (serum creatinine, BUN, urine output, creatinine clearance, electrolyte, acid-base balance, serum cystatin C, IL-18 and NGAL levels), need for temporary or permanent dialysis, length of hospital stay, and associated 30 day mortality. Study data are compared to published historical data that are collected and available for analysis from the Society of Thoracic Surgeons (www.STS.org). Historical data from this data base are collected and analyzed from all participating centers in the USA, and sub-analyzed for a reporting institution, such as IMC, and comparable institutions.
The trial is currently conducted in one center, IMC in Murray, Utah. Allogeneic MSC, derived from healthy, screened donors, using FDA approved protocols, are culture expanded under cGMP conditions at the University of Utah Cell Therapy Facility, Salt Lake City, Utah. MSC are administered in a dose escalation protocol to a total of 15 patients who have undergone elective, on-pump cardiac surgery (CABG and/or valve replacement). Five patients each receive low, medium or high dose of allogeneic MSC via a femoral catheter into the suprarenal aorta immediately after the patient comes off pump and is hemodynamically stable.
Low, Intermediate and High Doses of allogeneic MSC are defined per FDA approved protocol, and are infused into the suprarenal aorta in 50 ml of normal saline via a femoral catheter.
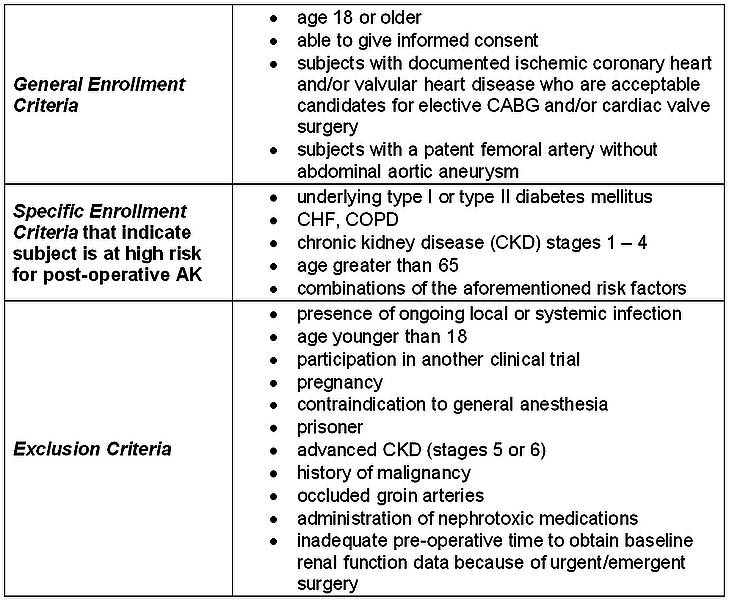
The enrollment and exclusion criteria for the trial are summarized in Table 1, below.
Table 1.
Results
Five eligible patients were enrolled for treatment with the lowest MSC dose. The clinical data on these study subjects are reported with their consent and approval of the IRB. The patients’ pre-operative AKI risk factors and surgical procedures are listed in Table 2. All patients underwent on-pump cardiac surgery for CABG and/or valve repair. All patients had at least one risk factor for post-operative development of AKI.
Table 2.

As stated in the introduction, several cardiac surgery associated factors have been identified as increasing the risk of post-operative AKI. These include the type of surgical procedure being performed, with multiple and/or valve procedures specifically being associated with higher risk; and the length of time on the bypass pump, with a bypass pump time of greater than 2 hours being associated with higher risk [4-6]. Table 3 lists the intra-operative risk factors for each of the five subjects.
Table 3.

Serum creatinine values for each of the five subjects, as markers of renal function, prior to and following surgery up to the present are shown on Figure 1.
Figure 1.

These data demonstrate that none of the first five study subjects developed significant AKI in the immediate postoperative time in the hospital, nor did patients 001-004 after discharge. Subject 005’s post-discharge data are pending. Significantly, no patient required dialysis immediately or later after surgery, and no expected or therapy-specific AEs or SAEs were observed. However, subject 004 died suddenly at home at 26 days after surgery and MSC administration. Both the principal investigator and the members of the DSMB determined that the patient’s death was not related to the study drug or its mode of administration. This SAE was immediately reported to the FDA, IRB and DSMB. The remaining four subjects are doing well as of the time of this report.
Discussion
This report summarizes the clinical course of the first five subjects in this first clinical safety trial world wide in which study subjects received allogeneic MSC after completion of on-pump cardiac surgery. It demonstrates that up to this point after surgery and discharge from the hospital infusion of allogeneic MSC at this low dose is safe, as no AEs or SAEs related to this novel therapy have been observed. Specifically, renal function was well preserved postoperatively, and none of the patients required hemodialysis. The sudden death of patient 004 at 26 days after surgery and MSC administration was judged by both the principal investigator and the members of the DSMB as being unrelated to the administration of allogeneic MSC.
Since close follow-up of each patient is continued for six months, and annual follow-up is conducted for another three years, it is possible that late AEs or SAEs may develop. This may include cardiovascular and pulmonary AEs detailed above, as well as the remote possibility of ectopic differentiation (e.g., in lungs or kidneys) of residual MSC into bone, fat or cartilage cells or oncogenic transformation. However, our detailed pre-clinical studies in experimental animals as well as numerous ongoing clinical trails with MSC (www.clinicaltrials.gov) make the latter AEs unlikely, since we have demonstrated that administered allogeneic MSC do not remain in the animal for more than three days, and that they do not differentiate into target cells and engraft in the kidney that is injured by experimental ischemia and reperfusion, the model that most closely resembles human ischemic AKI.
In the next groups of subjects, the acute and late safety of higher doses of allogeneic MSC will be assessed. At this point, the safety of the higher doses is not predictable and will have to be investigated. However, both our animal data and all reported clinical trials in which similar MSC doses were administered did not result in AEs or SAEs [7, 8, 10];(www.clinicaltrials.gov). It will finally be of interest to determine whether the obtained data from all 15 study subjects will allow an assessment of the preliminary efficacy of allogeneic MSC therapy in this cohort of high risk patients. If demonstrated, using relevant historical controls, it would be the basis for the conduct of a Phase II trial, in which the efficacy of this novel cell-based therapy is tested.
Acknowledgements
We greatly appreciate the excellent work of the University of Utah Cell Therapy facility and its director Dr. Linda Kelley. In this facility, all allogeneic MSC that were administered were characterized, culture expanded and release tested under cGMP conditions. The constructive contributions of the members of the DSMB (Drs. Carl Kablitz, Srinivasan Beddhu and David Affleck) are greatly valued. The conduct of this trial is funded and sponsored by AlloCure, Inc., and partially supported by the National Kidney Foundation (UT, ID), and the Western Institute for Biomedical Research.
References
1. Nickolas TL, O'Rourke MJ, Yang J, Sise ME, Canetta PA, et al. Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Ann Intern Med. 2008;148(11):810-9.
2. Goldberg R, Dennen P. Long-term outcomes of acute kidney injury. Adv Chronic Kidney Dis. 2008;15(3):297-307.
3. Girardi AC, Fukuda LE, Rossoni LV, Malnic G, Reboucas NA. Dipeptidyl peptidase IV inhibition downregulates Na+ - H+ exchanger NHE3 in rat renal proximal tubule. Am J Physiol Renal Physiol. 2008;294(2):F414-22.
4. Rosner MH, Okusa MD. Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol. 2006;1(1):19-32.
5. Hsu CY, Ordonez JD, Chertow GM, Fan D, McCulloch CE, et al. The risk of acute renal failure in patients with chronic kidney disease. Kidney Int. 2008;74(1):101-7.
6. Palomba H, de Castro I, Neto AL, Lage S, Yu L. Acute kidney injury prediction following elective cardiac surgery: AKICS Score. Kidney Int. 2007;72(5):624-31.
7. Togel F, Cohen A, Zhang P, Yang Y, Hu Z, et al. Autologous and allogeneic marrow stromal cells are safe and effective for the treatment of acute kidney injury. Stem Cells Dev. 2008.
8. Togel F, Weiss K, Yang Y, Hu Z, Zhang P, et al. Vasculotropic, paracrine actions of infused mesenchymal stem cells are important to the recovery from acute kidney injury. Am J Physiol Renal Physiol. 2007;292(5):F1626-35.
9. Togel F, Westenfelder C. Adult bone marrow-derived stem cells for organ regeneration and repair. Dev Dyn. 2007;236(12):3321-31.
10. Togel F, Hu Z, Weiss K, Isaac J, Lange C, et al. Administered mesenchymal stem cells protect against ischemic acute renal failure through differentiation-independent mechanisms. Am J Physiol Renal Physiol. 2005;289(1):F31-42.
11. Le Blanc K, Frassoni F, Ball L, Locatelli F, Roelofs H, et al. Mesenchymal stem cells for treatment of steroid-resistant, severe, acute graft-versus-host disease: a phase II study. Lancet. 2008;371(9624):1579-86.
12. Le Blanc K, Tammik L, Sundberg B, Haynesworth SE, Ringden O. Mesenchymal stem cells inhibit and stimulate mixed lymphocyte cultures and mitogenic responses independently of the major histocompatibility complex. Scand J Immunol. 2003;57(1):11-20.
13. Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. Jama. 2005;294(7):813-8.
Accepted 15 December 2008
Published 24 December 2008


